|
Medical Home
SETMA, LLP
The Story and the Ideals
The Story and the Ideals
Introduction to Preventive Health Tools
Preventive Care: The Best Way to Treat Illness is “Don’t Get it”
Coordination of Care
Patient-Centric Care
Population Health
Transition of Care - One form of Care Coordination
SETMA's Medical Home Pilgrimage
Concierge Medicine not Medical Home
Medical Neighborhood
Medical Home Description & Standards
NCQA Interview February 14, 2014
Welcome to SETMA’s Medical Home “Story Book.” The contents are the thoughts, ideas and analysis of SETMA about Medical Home and particularly about our medical home.. Formally, our story began February 17, 2009 when we attend a lecture about Patient-Centered Medical Home (PC-MH). In reality, our medical-home pilgrimage began decades ago. The initial part of our story is organized into three sections, each of which represents articles written in the years 2009, 2010 and 2011. A primer to SETMA’s medical home is at: The SETMA Model of Care: Patient Centered Medical Home; Healthcare Innovation, the Future of Healthcare.
Perhaps the most creative initiative in the transformation of health care is the concept of PC-MH.. At a time when there is great pressure for "reforming of the healthcare system," few understand that it is only transformation which will ultimately make a permanent difference. Reform is brought about by external pressure from without to force conformity to someone else’s idea of what healthcare ought to be. Reform only works for as long as pressure is applied and it is often resisted. Transformation is driven by an internalized passion which is generated by principles, convictions and personal vision.
In 2010, SETMA was recognized by the National Committee for Quality Assurance (NCQA) as a Tier 3, Patient-Centered Medical Home and was also accredited by the Accreditation Association for Ambulatory Health Care (AAAHC) and as a Medical Home. In 2011, SETMA was reaccredited by AAACH for both for a three-year term. In 2013 SETMA renewed NCQA’s Tier III Medical Home for 2013-2016. This year, we are applying for URAC medical home accreditation and in 2014 in addition to renewing our AAAHC accreditation we will apply for Joint Commission medical home accreditation.
It is our hope that this material may stimulate others to start their own Medical-Home pilgrimage and that others will begin to collect their own Medical-Home stories. If so, then this notebook's purpose will have been fulfilled. These articles chronicle our development of a medical home. The developmental history of SETMA will show that as early as 1999, we began defining the principles of what would become SEMTA’s Patient-Centered Medical Home. After becoming a Medical Home, SETMA realized that without knowing it, we had spent over ten years developing the functionalities which enabled us to be a medical home.
Our caution to others comes from our own failure which was that initially we focused almost totally on the structures of medical home without understanding the dynamic and spirit of patient-centeredness. Our story will repeatedly illustrate and example the tension between the structure and dynamic of PC-MH.
These structural principles will only take SETMA so far in becoming a true medical home. The next step is a radical change in the dynamic of care, a dynamic which will address how medical colleagues related to one another and how they relate to those they serve. As will be seen below, five months after SETMA defined the structural changes needed for being a medical home, on October 1, 1999, we defined the new dynamic. Under the old model of care, which we might refer to as a paternalistic healthcare system, patients were very often told what to do and it was expected that they would follow the healthcare providers’ instructions without modification. The definition of “paternalism” helps understand the old model of care; it is: “A policy or practice of treating or governing people in a fatherly manner, especially by providing for their needs without giving them rights or responsibilities.”
The dynamic of the medical home redefines the relationship of healthcare provider and patient, and changes how they relate! Rather than the patient encounter being didactic (to lecture or teach, as one with knowledge instructions or informs those who do not) - where the healthcare provider tells the patient what to do, how to do it and when to do it - the patient/provider encounter becomes a dialogue (An exchange of ideas or opinions) - where the healthcare provider and the patient discuss a mutual concern and then together come to a mutual conclusion with a mutually agreed upon plan. This new relationship is somewhat like a partnership.
The following are significant examples of SETMA’s medical home pilgrimage:
How Our Healthcare System Evolved and How It Must Change: Patient-Centered Medical Home
Finally, the dysfunction in the healthcare system, which was created by innovations and advances, was recognized. Gradually, efforts were made to modify this system and to eliminate the dysfunction. Quality measures were published which allowed the care provided by one provider to be measured against the care given by another. Preventive care was emphasized, but remained difficult because preventive care was rarely if ever a primary reason for a patient seeing a provider and it was often not paid for by insurance companies including Medicare and Medicaid. As care evolved efforts were undertaken to move the patient back to the center of the healthcare equation. Providers began to be encouraged to emphasize preventive care and health maintenance rather than just dealing with acute illness.
The patient threatened to kill the next doctor who came into his hospital room but he didn’t expect to meet a friend with a stethoscope.
Stories
Anecdotal medicine is frowned upon as it is based on personal experience without the benefit of "random controlled" or "double-blind" studies. Anecdotal medicine does now allow for analysis to determine if the conclusions of the experience are valid or not.
However, in the case of Medical Home, while there is an objective standard against which to measure the essential functions of a Medical Home, it is the "stories" which are powerful. It is the "stories" which give breath (in this case we refer to respiration and life) and depth (in this case we refer to significance and validity) to the experience. In fact, SETMA would recommend that NCQA, AAAHC, the Joint Commission and URAC - currently, the four agencies reviewing Medical Home applications -- establish a "stories exchange." This would be a place where illustrates of successes in Medical Home could be shared with everyone. Each story will flesh out, in three-dimensions "real life situations," our understanding of what otherwise are two-dimensional abstract ideals such as "coordination," "Care Transitions" and "patient-centric," among others.
Our Stories
SETMA has a growing list of stories which in fact are the sign posts on our pilgrimage. We include only two here. One story is from the first day we started to think about Medical Home. The second occurred two days before this introduction was prepared.
SETMA’s conscious pilgrimage toward Medical Home began February 17, 2009 when five SETMA colleagues attended a medical home presentation in Houston, Texas. The meeting was disappointing but it stimulated SETMA’s studying the concept. In March, 2010, SETMA submitted an application to NCQA for recognition as a Medical Home. In July, we received a Tier III recognition. The following series of articles track that process.
The future of healthcare and the foundation of PC-MH are going to be focused upon health and not simply upon excellent care of disease processes. Yet, the ideal of preserving and/or regaining a healthy state of being is not as easy as it sounds. Often, patients do not see any immediate benefit in making a change which may or may not make a difference in their sense of well being. Also, making a change in one's life style requires the hope that such change will make a difference. Many patients do not have hope. Many do not have the resources or mental or emotional capacity to make those changes. All of this complicates our realizing the promise of preventive care.
Typically, when we talk about "preventive health" we are talking about immunizations, screening and disease avoidance strategies. Another element of preventive health has to include risk stratification. Evidenced-based medicine not only helps us understand what treatment methodologies work but also who needs the most aggressive treatment either in prevention or therapeutics. "Preventive health" also must include life-style changes made by individuals. The difficult thing is that the preventive health and life-style changes take place long before the benefits of those changes become apparent.
To sustain preventive care initiatives and life style changes, healthcare providers with healthcare recipients must be able to sustain change over a long period of time. In order to do that, we need the ability to prove to patients that “if they make a change, that it will make a difference”. If patients are going to participate in “shared decision making,” a key concept in PC-MH, we must be able to demonstrate that a change will make a difference.
The most innovative use of the Framingham Risk Calculators were suggested by SETMA‘s associates at the Diabetes Center of Excellence in Boston (SETMA is the only multi-specialty Affiliate of the Joslin Diabetes Center). Drs. Richard Jackson and Ken Snow, while visiting SETMA, recommended the adding of a “What If Scenario” to our display of all twelve calculators.
The concept is that we are asking patients to make changes which will not show up as benefits for decades. Of course, ignoring those changes will result in irrevocable deterioration in the patient‘s health over those decades. But how do you prove to a patient that if you make a change, it will make a difference? One way is with the Framingham Risk Calculators being presented to the patient with the inclusion of the changes which would result if the patient improved the elements of the risk calculator.
Even though these risk calculators are not perfect, they are still the best we have. And, it is imperative that patients know and that their provider knows what their risk is, because it is with the knowledge of the patient‘s cardiovascular risk that a plan of care and a treatment plan can be designed to help preserve the patient‘s health.
Remember, Risk is an attempt to determine what the future might be like which means it is imprecise. Some people with a high risk will not experience poor health and some who have low risk will. Overall, however, those with high risk will have more heart attacks and strokes than those with low risk.
The problem with biological systems is that change, even change which results in deterioration of your health, does not occur quickly and it often occurs without any signs or symptoms until the illness, or disease process has already caused significant damage. There is no explanation of this principle more apt to our use of risk calculators than Peter Senge‘s explanation of dynamic complexity in The Fifth Discipline.
Senge defines dynamic complexity as a situation where cause and effect are subtle, and where the effects over time of interventions are not obvious. This perfectly describes the development of many disease states and the benefit of their treatment. We know that obesity causes, or contributes to most diseases including diabetes, hypertension, heart disease, cancer, etc. In these conditions, -obesity is the cause; cancer is the effect, but the change is slow and is not apparent. Also, the results of treatment are very slow. Consequently, it is hard to sustain the changes necessary to eliminate the cause, which is obesity, in order to avoid the - effect which is cancer.
Increasingly pre-diabetes and cardiometabolic risk syndrome are key elements of the risk stratification of our patients, not only letting us know that a patient needs to change but giving us a tool with which to motivate that change.
Quantifiable risk factors give a patient the ability to “see” the change which will make the difference. This is where science, patient behavior and medical home join forces to improve the health of patients.
Preventive health initiatives can be measured and they should be. But, if those measurements are going to make a difference, the results must be transparently shared with provider, patient and the public. In a conversation with the staff of the American Medical Association's Physician Consortium for Performance Improvement (PCPI) Department, SETMA addressed the "missing element" in quality measures and in the three-part Performance Improvement Continuous Medical Education described by the AMA in 2004. That missing element is a systematic and consistent auditing of a practice's and/or of a provider's performance on those quality measures.
As a result, SETMA has added a major new tool to our preventive health initiatives which is our Business Intelligence COGNOS Project. This will be described later in the Population Health Section of SEMTA’s medical home. In summary, this is the ability for SETMA to report internally to our providers and staff and externality to our patients and community how we are performing on over 300 quality-of-care metrics. SETMA's BI Project involves the auditing of:
- What preventive measures a patient needs, before they are seen.
- What preventive measures a patient receives whey they are seen.
- What preventive measures remain to be fulfilled.
- SETMA's LESS Initiative was begun in 2002 and was accepted by the Agency for Healthcare Research and Quality (AHRQ) in 2011. This Initiative is the core of SETMA’s preventive health program. Each patient seen at SETMA is confronted with these three needs. The LESS is intended to globally improve the health of those who receive their care at our clinic. LESS stands for:
L -- Lose weight
E -- Exercise
S -- Stop
S -- Smoking
While no one would argue that each of these is not valuable in the life or health of anyone, to our knowledge, there has never been a concentrated effort to confront an entire patient group with all three elements consistently every time they seek healthcare. Here is how the Initiative will work. Every time a patient is seen in the clinic, no matter what the occasion for the visit is, they will be alerted to the health risk of:
Their current weight, as measured by their body mass index (BMI) and their body fat content. They will be given a Weight Management Assessment which tells them their BMI, their disease risk associated with their current BMI and waist measurement, their percent body fat and an explanation as to how a 5% change in their body fat will impact their health and future.
The benefit which their heart and lungs are receiving from their current participation in exercise as indicated by the "aerobic points" which that exercise achieves for them and a recommend minimum exercise level which they need in order to achieve a "good" aerobic status for their age and sex. This exercise prescription will include information on how to increase the number of steps they take each day in order to have an "active" lifestyle which is defined by taking 10,000 or more steps a day. The average America takes fewer than 6,000.
The imperative for stopping smoking . Even the tobacco companies' websites now state, "The only way to avoid the health hazards of tobacco smoke is to stop smoking completely." This is clever because with this warning, the tobacco companies which continue to encourage tobacco smoking have immunized themselves from future litigation because they have warned you that their product is harmful. Now, legally, the only one to blame for the harmful effects of smoking is the smoker. Also, the initiative includes the questioning of patients about exposure to "environmental tobacco smoke" either at home or at work.
It is no longer enough to caution patient’s to avoid using all tobacco products, but they must also be counseled and encouraged to avoid environmental tobacco smoke (also referred to as secondary tobacco smoke or passive tobacco smoke). It is now known that in addition to primary tobacco smoke (smoking), secondary tobacco smoke (being around smokers) that “tertiary” tobacco smoke is carcinogenic. Tertiary smoke exposure is that which you smell on the clothing and body of others. There is NO safe level of exposure to tobacco smoke. As patients are “activated” in their medical home, i.e., they are informed and empowered to take charge of their own health, the first step is “stop smoking.” When you smell tobacco on others, you are inhaling carcinogenic materials.
A sedentary life style is either causative or contributory to all diseases including diabetes, cancer, heart and lung disease. SETMA’s LESS Initiative includes a personalized exercise prescription with special formulations for patients with diabetes and congestive heart failure. There are five complications of diabetes which impact the kind of exercise in which a patient should engage. SETMA’s exercise diabetes prescription addresses appropriate modifications for each of those. Patients with severe physical limitations should not avoid exercise. SETMA’s CHF Exercise prescription describes how a poorly condition person should begin with two minutes of activity until they can work up to 15 minutes, then thirty, etc.
It is simplistic to say, but the best way to treat any disorder is “don’t get it.” This is particularly true in the case of Type 2 Diabetes, Hypertension and Obesity. SETMA’s medical home is focused on health and wellness, which includes the prevention these most common disorders. The following tutorials explain SETMA philosophy and plans in this prevention effort.
Assessing patients at risk for diabetes and giving them strategies for preventing the development of diabetes.
Recognizing that everyone who does not have hypertension at age 55, has a 90% life-time risk of developing hypertension strategies are recommended to patients for how to avoid hypertension.
Beyond wellness and preventive care, the heart of PC_MH is the coordination of care. The following gives details about SETMA’s Care Coordination. One of the “catch phrases” to medical home is that the care is “coordinated.” While this process traditionally has referred to scheduling, i.e., that visits to multiple providers with different areas of responsibility are “scheduled” on the same day for patient convenience, it has come to mean much more to SETMA. Because many of our patients are elderly and some have limited resources, the quality of care they receive very often depends upon this “coordination.” It is hard for the frail elderly to make multiple trips to the clinic. It is impossible for those who live at a distance on limited resources to afford the fuel for multiple visits to the clinic. “Coordination” has come to mean to SETMA, scheduling which translates into:
- Convenience for the patient which
- Results in increased patient satisfaction which contributes to
- The patient having confidence that the healthcare provider cares personally which
- Increases the trust the patient has in the provider, all of which,
- Increases compliance in obtaining healthcare services recommended which,
- Promotes cost savings in travel, time and expense of care which
- Results in increased patient safety and quality of care.
As with the structure of quality metrics in tracking, auditing, analyzing and public reporting process and outcomes measures, coordination requires intentional efforts to identify opportunities to:
- Schedule visits with multiple providers on the same day, based on auditing the schedule for the next 30-60 days to see when a patient is scheduled with multiple providers and then to determent if it is medically feasible to coordinate those visits on the same day.
- Schedule multiple procedures, based on auditing of referrals and/or based on auditing the schedule for the next 30-60 days to see when a patient is scheduled for multiple providers or tests, and then to determine if it is medically feasible to coordinate those visits on the same day.
- Scheduling procedures or other tests spontaneously on that same day when a patient is seen and a need is discovered.
- Recognizing when patients will benefit from case management, or disease management, or other ancillary services and working to resources those needs.
- Connecting patients who need help with medications or other health expenses to be connected with the resources to provide those needs such as The SETMA Foundation, or sources.
Time, energy, and expense are conserved with these efforts in addition to increasing compliance thus improving outcomes. In order to accomplish this and to gain the leverage, synergism and advantage of coordination, a system is necessary which brings us to a new position designed by SEMTA entitled, Director of Coordinated Care.
The Director of Care Coordination is responsible for building a department of Care Coordination. In many ways this could be called the “Marcus Welby Department,” as it recognizes the value of each patient as an individual and has as its fundamental mission the meeting of their healthcare needs and helping them achieving the degree of health which each person has determined to have. The driving force is to make each patient feel as if they are SETMA’s ONLY patient, just like Dr. Welby.
Initially, the DCC will work as a department of one but will have others assigned to the department as the demands of the mission expand. The DCC will establish protocols and methods for facilitating the care of patients with: special needs, complex-care needs, disease management and case management needs.
An illustration of this new function will be that of a patient who is seen at SETMA’s Wilson clinic on the West End of Beaumont. The provider determines that the patient needs an echocardiogram. The nurse will call the Care Coordination Department, which will determine if the patient can be sent to the Ultrasound Department immediately to have the test done that day. We believe that this will increase patient satisfaction as well as compliance which will improve the quality of care the patient will receive.
The medical home sees the patient as a whole and not as a collection of isolated and disconnect disease processes. While this is not new and has always been the ideal of health care, it becomes a significant focus of the patient-centered medical home. Not only is the patient the major focus of the attention given, but all elements of the patient’s needs are attended to and future needs are anticipated and addressed. No longer is a patient encounter simply used to address current needs but potential future needs are identified and addressed. For instance, the young person who is seen for an upper respiratory condition but who is moderately obese, and who has a family history of diabetes, has his disease-risk addressed. In addition, recommendations are made for diabetes prevention and wellness including exercise, weight reduction, avoiding tobacco and others. Future contacts are scheduled, with our without a clinic visit, for assessing whether the patient has made the changes necessary to maintain their health.
Furthermore, through NextMD, SETMA’s secure web portal, the patient is referred to education material for achieving the desired results and a follow-up contact via e-mail is scheduled to remind the patient, without a clinic visit and without cost, to pay attention to their health.
A medical home measures the quality of care which patients are receiving both through process analysis and outcomes measurement through quality metrics. Quality Improvement Initiatives are planned for the improvement of care across an entire population of patients. For instance, while it is anticipated that the new Director of Coordination of Care will result in improved care, that must be measured and analyzed before it will become obvious that the anticipated improvement has occurred.
As the Director of Care Coordination works with SETMA’s Call-Center staff to address preventive health needs of our patients, it will be important to see if more people are getting their mammograms, bone densities, immunizations, etc. If they are, then the position will have proved value. If they aren’t then new ways will have to be used to improve those outcomes. If the DCC is responsible for scheduling multiple visits or studies on the same day, it will be necessary to measure whether or not that has improved compliance and consequently quality of care. If the DCC is responsible for evaluating whether the post-hospital follow-up call program and the post-clinic-visit follow-up call program is having the desired result, it will be necessary to measure those outcomes. If the desired result does not occur new or additional initiatives will have to be designed.
To be a medical home, a practice must provide communication with a personal physician who accepts primary responsibility for the patient’s care. This is more than a friendly affect when the patient is seen in the clinic. It means answering inquires about health from the patient at times other than when they are seen in the clinic. It means providing telephone access with same-day response; e-mail contact through a secure web portal with same day access; it mean eliminating a patient’s anxiety about whether or not their healthcare provider cares about them by the provider being available to the patient. It may mean in some cases that the patient has the provider’s home telephone number or cell phone number. It means doing whatever is necessary for making sure the patient knows how to access care when it is needed. The reality is that the more confident a patient is that they can reach their provider when needed; the less likely the patient is to pester the provider over trivial or unimportant matters.
Continuity of care in the modern electronic age means not only personal contact but it means the availability of the patient’s record at every point-of-care. One of the AAAHC surveyors said that his standard for judging medical records is, “Could I pick up this chart and provider excellent care for a patient whom I had never seen?” His answer after reviewing dozens of SETMA charts is, “I could easily treat any of these patients as the records are legible, complete and well organized.” Because all of the patient’s health needs are clearly documented; because all preventive and screening health needs are constantly and automatically audited; because every patient’s laboratory results, medications and diagnoses are interactive; every patent can be confident that all of their health needs are being addressed, can be addressed and will be addressed, no matter who the provider is that they see.
Another issue of continuity of care is communication among all providers and institutions that are providing care for each patient. The Health Information Exchange which SETMA is launching will provide the confidence that care given by hospitals, emergency rooms, specialists, other primary care providers, etc., will be accessible to all providers and will be integrated into the patient’s health record. In addition the secure web portal, NextMD, will allow the patient to maintain and periodically review their own personal health record. This places the patient at the center of their healthcare decision-making process, which is the ideal of patient-centered medical home.
These are the elements of the process of care coordination and when fulfilled, they should result in coordinated care. The outcomes of care should be improved and excellent care should be the result of all who are part of a Patient-Centered Medical Home.
This function allows the aggregation of data required for the coordination of patient care including care givers, barriers to care, quality metrics including HEDIS, NQF and others,. This review is done by the provider and his/her staff.
When the Coordination Review has been completed, a document is completed which is given to the patient so that the patient knows the status of their care coordination. This is an important aspect of patient activation, engagement and shared decision making.
This describes the functions of the care coordination department and the function of the ability of providers to send referrals to the department for home health, adult and child protective services, financial assistance and other special needs.
A significant part of care coordination and care transition is enhanced communications with the patient. This includes follow-up calls from the clinic when appropriate and follow-up, care-coaching calls to all patients who are discharged from the hospital.
Healthcare providers need a method for effectively following-up on care needed by patients. This tool allows an electronic reminder to be created so that the provider and the clinic staff can make certain that scheduled care was done whether it is three months or three years later.
CMS contracted with RTI International to study 312 Medical Homes benchmarked against 312 non-coordinated practices for quality, coordination and cost. SETMA’s result is posted here.
Every practice which is or which desires to be a PC-MH must ask itself, “Do we simply have the structure of a medical home, or do we have both the structure and the dynamic. Being a medical hoe has more to do with dynamic than it does with structure. Definitions and understanding of the concepts of this redesign are inextricably related. The authors stated: “Adding to the confusion, the term patient engagement is also used synonymously with patient activation and patient- and family-centered care. Although the concepts are related, they are not identical” If healthcare providers are going to be able to make the transition from expecting “compliance” on their clients part, to the experience of patients “adhering” to a mutually agreed upon healthcare plans of care, it is imperative that we understand the vocabulary.
- “Patient activation-an individual’s knowledge, skill, and confidence for managing his/her own health and health care -- is one aspect of an individual’s capacity to engage in that care. But this term does not address the individual’s external context, nor does it focus on behavior.
- “Patient- and family-centered care is a broader term that conveys a vision for what health care should be: a partnership among practitioners, patients, and their families (when appropriate)’ to ensure that decisions respect patients’ wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care.
- “...Patient and family engagement as patients, families, their representatives, and health professionals working in active partnership at various levels across the health care system-direct care, organizational design and governance, and policy making-to improve health and health care. Although we use the term patient engagement for simplicity’s sake, we recognize that those who engage and are engaged include patients, families, caregivers, and other consumers and citizens.”
HCAHPS an Imperative for Creating a Patent-Centered Experience
The objective assessment of a patient’s experience of care in the hospital (Hospital Consumer Assessment of Healthcare Provider and Systems) and in the ambulatory setting (Consumer Assessment Healthcare Provider and Systems) are critical to providers learning the dynamic of patient-centered medical home.
This gives a definition of terms and how a guide to prepare patients to be a part of their medical home team.
SETMA 8.20.13 Provider Training -- Health Affairs 2.14.13 -- Patient Engagement
"Patient engagement" is a broader concept that combines patient activation with interventions designed to increase activation and promote positive patient behavior, such as obtaining preventive care or exercising regularly. Patient engagement is one strategy to achieve the "triple aim" of improved health outcomes, better patient care, and lower costs.
The Conversation Project is a project of the Institute for Healthcare Improvement and is dedicated to helping people talk about their wishes for end-of-life care. We know that no guide and no single conversation can cover all the decisions that you and your family may face. What a conversation can do is provide a shared understanding of what matters most to you and your loved ones. This can make it easier to make decisions when the time comes.
In the Medical Home Model of healthcare, it is imperative that the patient participates in their own care. Terms like “activated,” “engaged,” and “shared decision making” are important descriptions of the dynamic of the patient participating in and actually “taking charge” of their own care. As part of this process, it is important that the patient’s preparation to change be sustained. In other tools, SETMA discusses the power of “What if Scenario,” which addresses the providers ability to quantify for the patient that fact that “if they make a change, that that change will make a difference in their health.” This is principally done through the Framingham Risk Scores and the ability to display the difference a change in behavior will make. That tool can be reviewed in either:
The assessment of a patient’s preparation to make a change can most effectively be done through the Transtheoretical Model Assessment of the Stages of Change which can measure the patient’s preparation of making the changes recommended in SETMA’s “What if Scenario.” The following steps explain how to use SETMA’s deployment of the Transtheoretical Model.
- Paternalism or Partnership: The Dynamic of the Patient-Centered Transformation
From a 1951 movie, People Will Talk, where the dynamic and principles of the patient-centered medical home are illustrated
From a 1937 movie Citadel about a Scottish doctor who illustrates a physician following prey to entrepreneurism and loses and forgets his professionalism but regains his healthcare soul.
In 1993, John Patrick set IBM on another course and changed the company's future. Reading his story made me wonder, is it possible for SETMA to set medicine on another course and to change the future. John did not want people to work “collaterally,” side by side, maybe going in the same direction, maybe even having the same goal, but working independently and at best in a cooperative manner; he wanted people to work “collaboratively,” synergistically, leveraging the generative power of a team in creating a new future which they partially envision but which even they could not control.
What can we do today in healthcare which would mirror the changes IBM experienced? How can we change “collaterallists” into “collaborativists”? How can we use the power of electronics, analytics, and informatic principles to energize radical change to create a new future in healthcare? Testing and measurement is a science. In most industries, quality is determined by testing performance. But, in healthcare we are involved in a new kind of “testing.” The tests used to measure the performance of healthcare providers are unique.
SETMA’s Disease Management tools For Diabetes, Hypertension and Lipids Used for patient activation and engagement via written Plans of Care and Treatment Plans
Providing our patients a written, personalized Treatment Plan and Plan of Care is a critical aspect in patient activation and engagement. These documents serve as a “baton” which empowers the patient to care for themselves. The following poster which appears in all SETMA’s examination rooms and a framed copy of which appears in all public places at SETMA symbolizes the “baton.”
Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient, If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
We have already stated that accountability and transparency are the principal reasons for public reporting of our performance, but there is more to accountability and transparency in healthcare than that. We b believe that public reporting of quality performance will change provider and patient behavior. Typically healthcare providers only receive delayed, retrospective reviews of their performance, which does not change behavior significantly, in our judgment. In the Old Testament, a verse declares that "because punishment against an evil deed is delayed, the hearts of men are set upon doing evil." The principle is that without immediacy between the consequences and/or evaluation of an action and the action itself, the potential for the consequence to effect positive change is diminished or eliminated. While auditing provider performance is never for punitive reasons, the principle is the same. If the reporting of the results is significantly removed in time from the events being audited, it will have little impact upon provider behavior.
In his book, The Fifth Discipline, Peter Senge of MIT used the classic metaphor of the Frog in Boiling Water to address the same issue from a different perspective. He explains, "If you put a frog into cool water; he will swim around. If you begin to heat that water, the change is so gradual that the frog will not recognize the danger until it is too late for the frog to escape." The same is true of patients and healthcare providers. Because the changes in patient health are generally very slow and without immediate consequences (symptoms), both provider and patient can become complacent.
The medical literature addresses this complacency with the concept of "treatment inertia," the tendency on the part of healthcare providers to do nothing, even when something should have been done. Most of the research on "treatment inertia" has been done in the medical education arena where it is expected that "best practices" will always be present. There is no intent in this project of punishment, or of boiling anyone in hot water, but the intent is to find a way to change provider behavior and to overcome "treatment inertia." SETMA believes, as is also addressed by Senge, that the only effect way to change patient and provider conduct in the face of chronic conditions which cause no short-term discomfort but which have long-term devastating consequences, is to create discomfort in both in order to overcome "treatment inertia" and/or current apathy toward inevitable bad outcomes.
The Physician Consortium for Performance Improvement (PCPI) is an organization created by the AMA, CMS, Institute of Medicine and others to develop measurement sets for quality assessment. The intent is to allow healthcare providers to evaluate their own performance at the time they are seeing a patient. SETMA is tracking a number of these measurement sets including: Chronic Stable Angina, Congestive Heart Failure, Diabetes, Hypertension, and Chronic Renal Disease Stages IV through ESRD, Adult Weight Management, and Care Transitions. Others will be added overtime. The details of these measurement sets and SETMA's provider performance on each can be found at under Public Reporting PCPI.
In addition to Provider Performance Tracking tools such as those produced by PCPI, the National Quality Foundation (see Public Reporting NQF), and National Committee for Quality Assurance (see Public Reporting HEDIS and/or NCQA), SETMA has designed a pre-visit quality measures screening and preventive care tool. This allows a SETMA provider and a patient to quickly and easily assess whether or not the patient has received all of the appropriate preventive health care and the appropriate screening health care which national standards establish as being needed by this patient.
For an analysis of ethnic disparities, our data for the treatment of diabetes for the past twelve months is as follows:

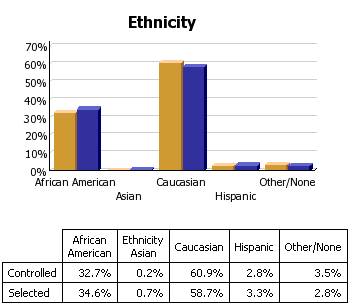
Before the judgment is made that Caucasians receive significantly better healthcare, the bar graph must be described.
- 3783 patients seen by SETMA providers in the past twelve months had diabetes.
- As a percentage of the 3783 patients with diabetes 1,323 were controlled. (For this audit, "controlled" is defined as the patient having had a HgbA1C below 6.5 % for the entire year.) If, as in the case of the National Quality Forum (NQF) Comprehensive Diabetes Measurement Set, "controlled" were defined as below 7% and the measure called for an examination only of the most recent HgbA1C, the percentage of those designated as "controlled" would rise to 59.9%.
- 60.9% of the patients who had diabetes and who were seen in the past twelve months and whose HgbA1c was below 6.5% for the entire year, were Caucasians
- 32.7% of African American treated by SETMA who had diabetes, who were seen in the past twelve months and who had HgbA1C done had a HgbA1C continuously below 6.5%.
- The second classification on this graph is entitled "selected." In the case of the above bar graph, "selected" refers to all patients whose diabetes, at any point in the year, was above 6.5%. There were 2460 of them.
At first glace, it might be assumed that the care of Caucasians was twice as good as that of African Americans. But note that the percentage of "controlled" and "Selected" is not of a subset but a percentage of the same whole. As a percent of the whole, SETMA treats twice as many Caucasians as African Americans. As a percent of those who exhibited continuous control of their diabetes, it is the same proportion of African American as Caucasian. Their treatment judged by process measures or by outcomes measures is identical. The conclusion is that the ethnic distribution of all of SETMA's patients with controlled diabetes is nearly identical to the ethnic distribution of SETMA's patients with uncontrolled diabetes.
- Analytics transform knowledge into an agent for change.
- In reality, without analytics, we will neither know where we are, where we are going or how to sustain the effort to get there.
- For transformation to take place through knowledge, we must be prepared to ask the right questions, courageously accept the answers and to require ourselves to change.
- The greatest frustration to transformation is the unwillingness or the inability to face current reality. Often, the first time healthcare provides see audits of their performance, they say, “That can’t be right!”
- Through analytics - tracking data, auditing performance, statistical analysis of results - we learn the truth. For that truth to impact our performance, we must believe it.
Transitions of Care is one of the forms of Care Coordination
- Evaluation at admission -- transition issues : “lives alone,” barriers , DME, residential care, or other needs
- Fulfillment of PCPI Transitions of Care Quality Metric Set
- Post Hospital Follow-up Coaching -- a 12-30 minute call made by members of SETMA’s Care Coordination Department
- Plan of Care and Treatment Plan
- Follow-up visit with primary provider
While the traditional “discharge summary” should have been the most important document created during a patient’s hospital stay, it historically came to be nothing but a document created for an administrative and billing function for the hospital and attending physician. It has long cease to being a dynamic document for the improvement of patient management. The “discharge summary” rarely provided continuity of care value, or transitions of care information, such as diagnoses, reconciled medication list, or follow-up instructions. In reality, the “discharge summary” was often completed days or weeks after the discharge and was a perfunctory task which was only completed when hospital staff privileges were threatened or payment was delayed.
The “discharge summary” should have always been a transition-of-care document which not only summarized the patient’s care during the hospitalization but guided the patient’s post-hospital care with a plan of care and treatment plan. In this way, the document would have been a vehicle for patient engagement and activation.
In September, 2010, SETMA representatives as an invited participate attended a National Quality Forum conference on Transitions of Care. (http://jameslhollymd.com/Letters/nqf-summary-of-dr-hollys-comments-sept-2-2010) During that conference, SETMA realized that the name “discharge summary” needed to be changed. It was thought that a name change would clarify and focus the intent of this critical document. The name was changed to “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.”
While transitions of care are most commonly thought of as being from inpatient to outpatient, every time a patient eaves a provider’s office, a transition of care takes place. The transition is from the provider to the patient being the principle party responsible for the patient’s care. In fact, the patient is reasonable for their own care for more of the time than is the provider. The patient’s “baton,” - their treatment plan and plan of care - empowers then to “take care of their own health for over 8,740 hours a year.
No matter how talented the members of a relay team are, the most critical point of their collective performance is in the transition from one runner to another. At this point, one runner, moving as fast as he/she can, must hand the baton to another runner, who has started running as fast as he/she can, before the first runner has even arrived in the "transfer zone." As if this were not complex enough, the rules of the race require that the transfer of the baton must take place within a certain zone.
If the baton is dropped or if the transfer is not made in the prescribed time, the team, no matter how gifted will be disqualified and will lose the race. As with life and with healthcare, it is not always the brightest, fastest, best person who wins. It is the person, in this case, the team, which not only performs well in their individual area of responsibility but who also performs well in transferring the results of his/her performance to the next participant and who does so within the constraints of the rules. Often, it is forgotten that the member of the healthcare delivery team who carries the "baton" for the majority of the time is the patient and/or the family member who is the principal caregiver. If the "baton" is not effectively transferred to the patient or caregiver, then the patient's care will suffer.
In healthcare there are transition points-of-care, where the "baton", which now represents the transfer-of-care responsibility from one person to another, must be smoothly, efficiently and timely accomplished, or the value of the care provided by each care giver will be diminished to the point that the overall quality of care may be less than the sum of the contributions of each care giver. This diminishing of the value of care occurs when only a small part of the value of each participant's contribution is successfully transferred to the next point-of-care. This occurs when the "baton" is dropped.
In January, 2013, CMS published two new Evaluation and Management Codes (E&M Codes) which were adopted in order to recognize the value of the processes of transitioning patients from multiple inpatient sites to multiple outpatient venues of care. The value of this work is now being recognized by enhanced reimbursement. CMS has also published three codes for Complex Chronic Care Coordination, which is considered bundled payments in 2013 but in 2014 are scheduled for additional payment to primary care providers.
|