|
Index
Stand Alone Benefit
“G” Codes for Intensive Behavioral Therapy
The content of the Intensive Behavioral Therapy
Transtheoretical Model Stages of Change (TMSC)
SETMA’s Deployment of Transtheoretical Model
Transtheoretical Model in Weight Management, Diabetes, Hypertension
Intensive Behavioral Therapy (IBT) for Obesity
Template for Requirements for Billing IBT Obesity
Failure to Meet Standards for Billing IBT Obesity
Details of IBT Obesity G0477 Face-to-face behavioral counseling for obesity
Intensive Behavior Therapy Cardiovascular Disease
Requirements for IBT for Cardiovascular Disease
Tools for IBT for Cardiovascular Disease
Meeting the Requirements with the Transtheoretic Model
General concepts about the IBT Cardiovascular Disease Billing
Health and Human Services through CMS is becoming increasingly more involved with preventive care and more payments are being made for screening and preventive care which will ultimately make a difference in the care, the health and the cost of care for Medicare beneficiaries. Two new services are:
- Intensive Behavioral Therapy (IBT) for Obesity (G0477)
- Intensive Behavioral Therapy (IBT) for Cardiovascular Disease (G0446)
- The following reference is to CMS’s Intensive Behavioral Therapy (IBT) for Obesity.
- The following reference is to CMS’s Intensive Behavior Therapy (IBT) for Cardiovascular Disease.
The IBT for obesity (up to 22 visits a year) and/or Cardiovascular Disease (once a year) are stand-alone billable services. IBT is separate from the Initial Preventive Physical Examination (IPPE) or the Annual Wellness Visit (AWV). Medicare beneficiaries may obtain IBT for obesity or cardiovascular services at any time following Medicare Part B enrollment.
Each IBT for obesity or Cardiovascular Disease must be consistent with the 5A’s approach adopted by the US Preventive Services Task Force (USPSTF). This approach includes:
- Assess: Ask about or assess behavioral health risk(s) and factors affecting choice of behavior change goals or methods;
- Advise: Give clear, specific, and personalized behavior change advice, including information about personal health harms and benefits;
- Agree: Collaboratively select appropriate treatment goals and methods based on the beneficiary’s interest in and willingness to change their behavior;
- Assist: Use behavior changing techniques (self-help and/or counseling), aid the beneficiary in achieving agreed-upon goals by acquiring the skills, confidence, and social or environmental supports for behavior change, supplemented with adjunctive medical treatments when appropriate; and
- Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoing assistance or support and to adjust the treatment plan as needed, including referral to more intensive or specialized treatment.
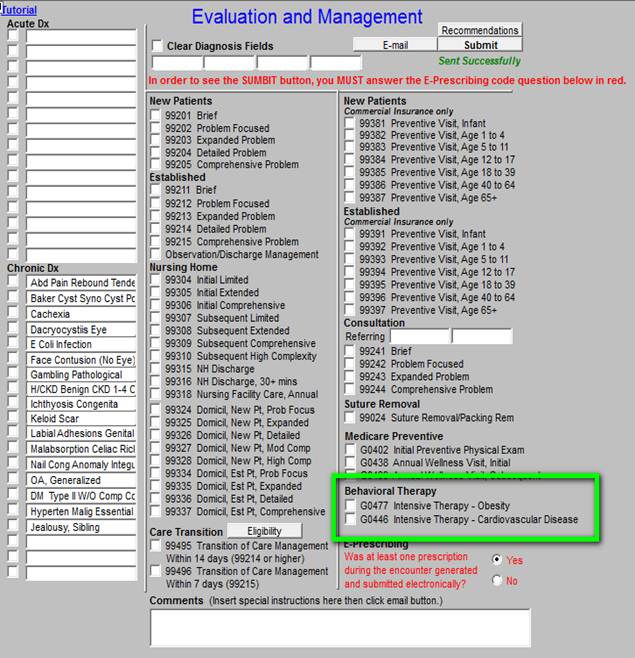
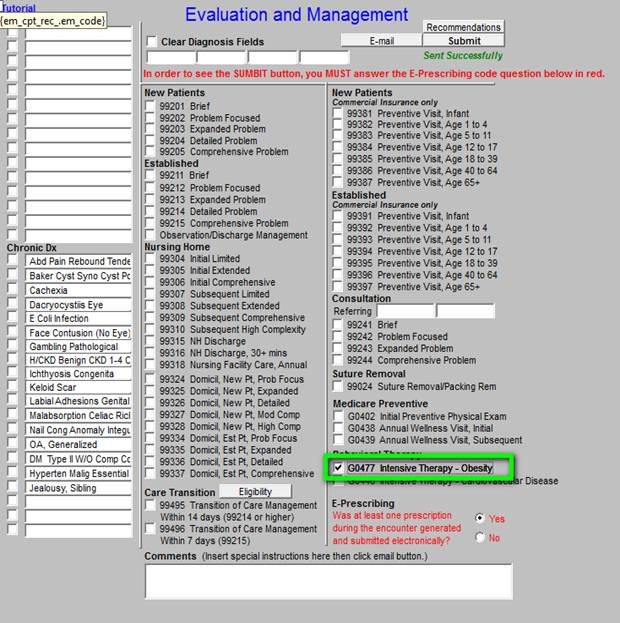
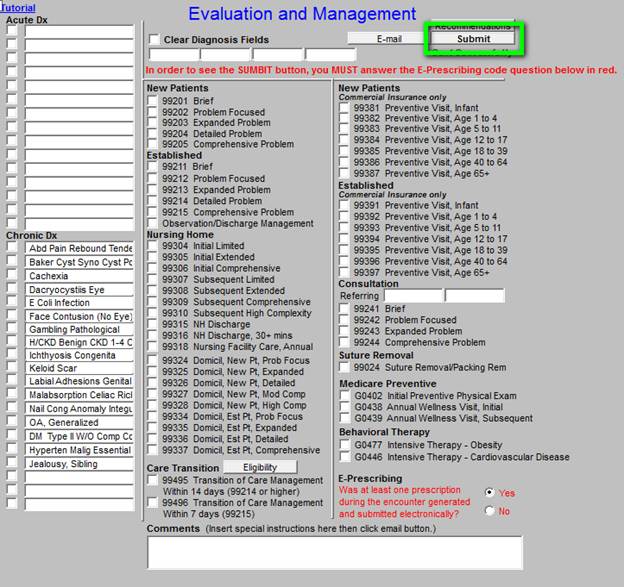
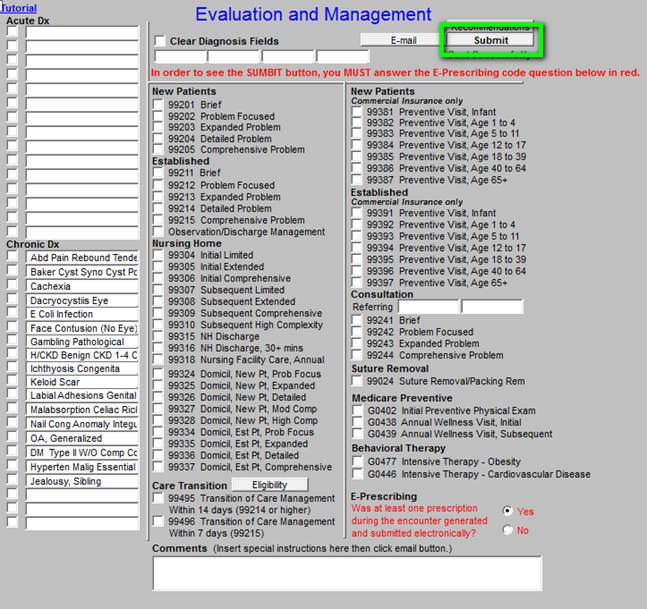
An entire visit can be devoted to one of these services, or they can be conducted in conjunction with other services and the provider can bill for both. The G Codes for these two preventive service are found on SETMA’s Evaluation and Management template and are shown below in green:
This content will be derived from SETMA’s disease management tools for:
- Weight management
- Diabetes
- Cardiometabolic Risk Syndrome
- Hypertension
- Dyslipidemia
- Congestive Heart Failure
- Renal Disease
- Preventing Diabetes and Preventing Hypertension
- LESS Initiative (Lose Weight, Exercise, Stop Smoking)
Tutorials for the use of each of these tools can be found on:
- SETMA’s website at www.jameslhollymd.com under EPM Tools (Electronic Patient Management).
- SETMA’s Intranet,
- Embedded into SETMA’s Electronic Medical Records
- Printed material
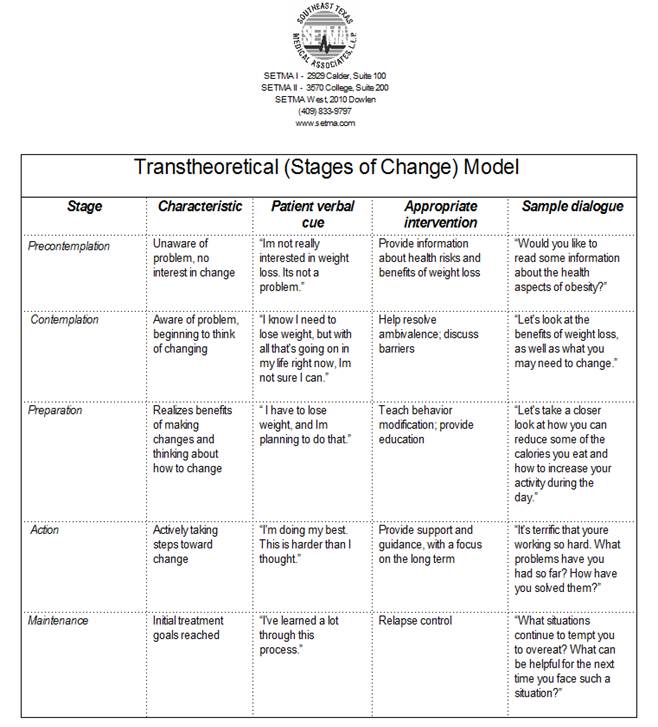
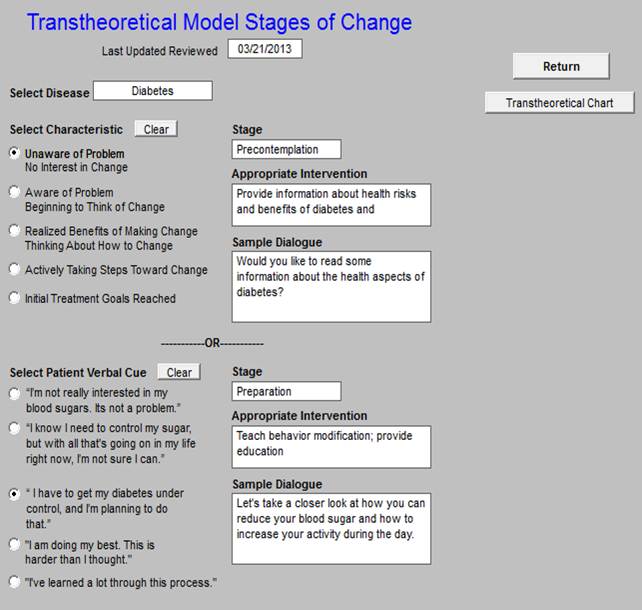
Changing behavior and sustaining that change is the crux of the issue relating to IBT. One of the tools which SETMA has built for this effort is the electronic deployment of the Transtheoretical Model Stages of Change. The following is the detail on this tool.
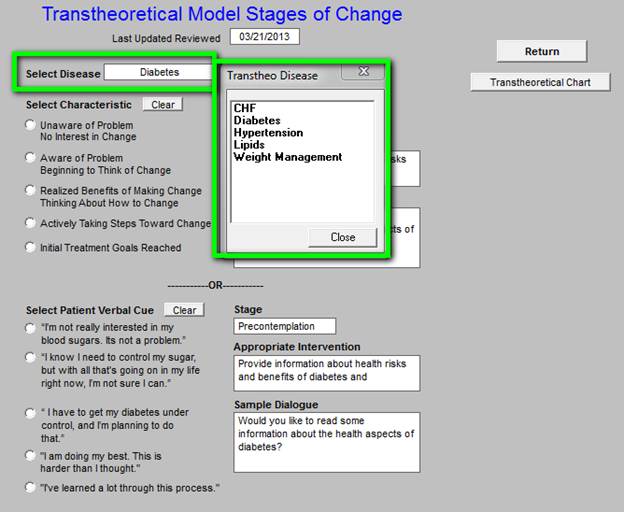
SETMA has created the ability to utilize the TMSC in five distinct conditions as seen on the template below outlined in green.
Because human beings are not static in their response to their health and behavior, this deployment allows SETMA providers to assess a patient’s:
- Stage of Change
- Characteristics
- Patient Verbal Cue
- Appropriate Intervention
- Sample Dialogue
for each IBT encounter. As the patient’s attention to, concern for and self-motivation for change moves through the continuum of stages of change, the discussion with the patient can be adjusted to meet their current needs with an effective patient/provider dialogue rather than the healthcare provider having a one-size-fits all monologue with the patient conducted by the provider only.
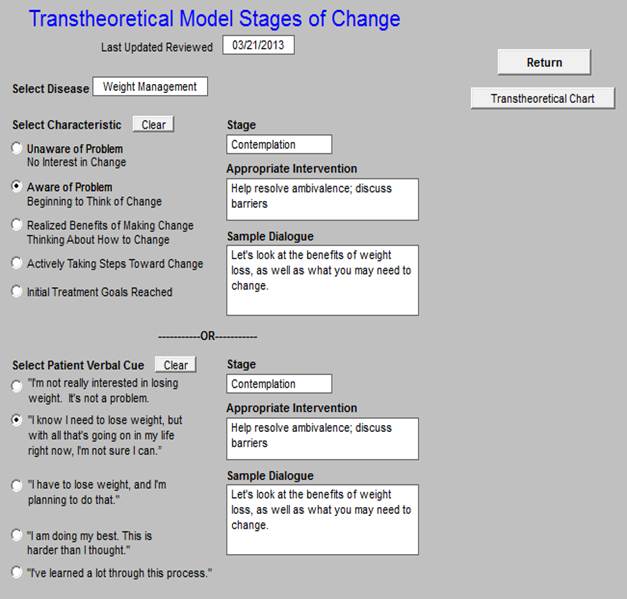
The following illustrates the use of this tool in weight management, diabetes and hypertension:
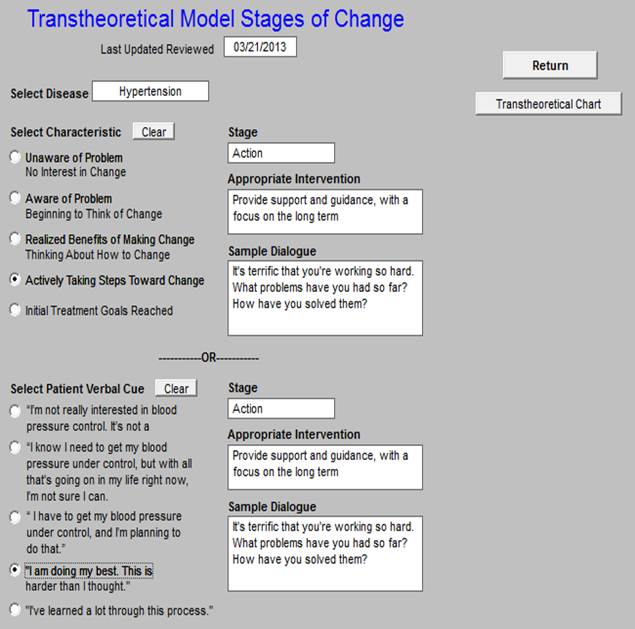
The Transtheoretical Model can be accessed from SETMA’s AAA Home as shown below outlined in green, or from the Intensive Behavioral Therapy for Obesity or the Intensive Behavioral Therapy for Cardiovascular Disease templates which will appear when a provider accesses the IBT for obesity or cardiovascular disease (see below).
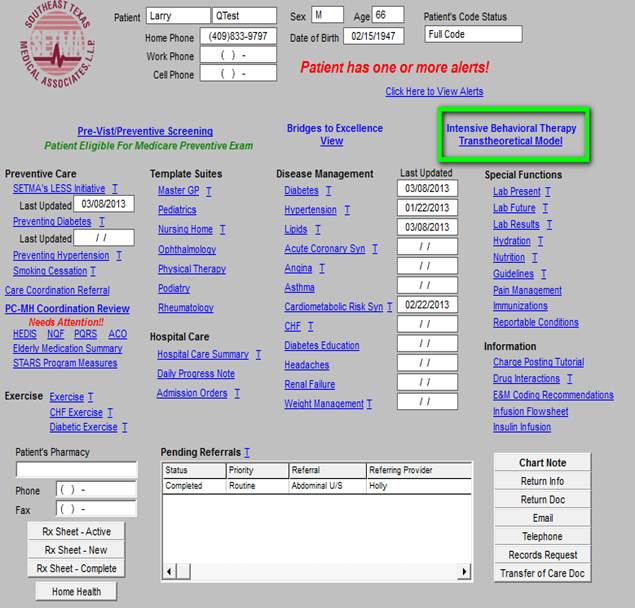
With SETMA’s deployment, it is possible to review over time the patient’s “stage of change” for each of the five tools which were used in their care. This will allow the patient to see their consistency in pursuing their health goals.
If:
- The provider spends fifteen minutes counseling the patient about obesity
- The patient has a BMI equal to or great than 30
- The patient is mentally competent and alert
The provider can bill for IBT for Obesity. You do that by click the G code as shown below surrounded in green.
As you consider the use of the IBT Obesity code, do not forget the LESS Initiative (Lose Weight, Exercise and Stop Smoking) and SETMA’s Weight Management tool. Both of these tools provide the guidance and documentation required to fulfill the elements of the IBT Obesity. In addition, the Plan of Care and Treatment Plan associated with each of these tools (some of which were listed previously) serve as excellent connectors between the IBT and the patient’s daily life. Tutorials for these two functions can be found at:
LESS Tutorial
Adult Weight Management Tutorial -- part of this tutorial is a twenty-page explanation of the Transtheoretical Model Assessment of Change
When you click the box next to G0477 (see outlined in green above), the following template will appear which requires you to answer three questions.
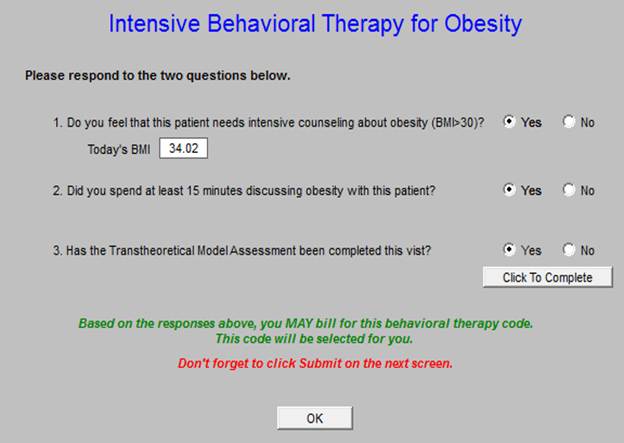
If you answer “yes” to all three questions, the wording will appear, “Based on the response above, you MAY bill for this behavioral therapy code. This code will be selected for you.” If you have not completed the Transtheoretical Model of Change, you may do so by clicking on the button “Click to Complete.”
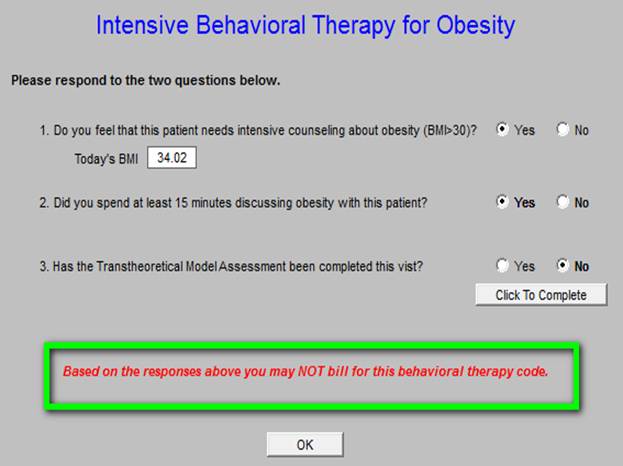
If you answer “no” to any question, as shown below outlined in green you will be alerted to the fact that you cannot bill for IBT Obesity.
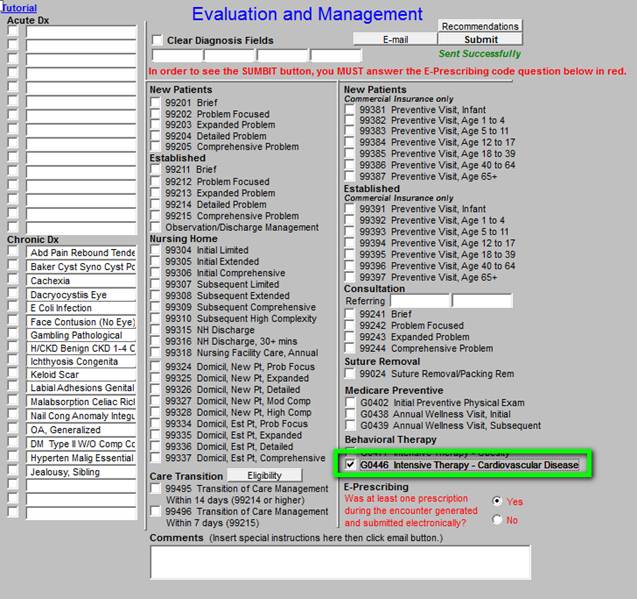
Once you have received notification that you can bill for IBT Obesity, you need to click the Submit button as seen below outlined in green.
Stand Alone Benefit - this means that it can be done in association with other care or it can be done as a separate care by itself.
- The IBT for Obesity benefit covered by Medicare is a stand alone billable service.
- It can be billed with or apart from the IPPE, or the Annual Wellness Visit (AWV).
- Medicare beneficiaries may obtain IBT for obesity services at any time following Medicare Part B enrollment, including during their IPPE or AWV encounter.
Criteria for providing this service - Patient must:
- Have BMI > or equal to 30 kilograms per meter squared.
- Must be mentally competent at the time of counseling
- Must be counseled by Primary Care Provider: family physician or nurse practitioner
A maximum of 22 visits are permitted in a 12-month period, allocated as such:
- one face-to-face visit every week for the first month;
- one face-to-face visit every other week for months 2-6; and
- one face-to-face visit every month for months 7-12, if the patient meets the 3 kg (6.6 lbs) weight loss requirement during the first 6 months.
In the event a Medicare patient qualifies for and receives IBT for obesity in your primary care setting, report HCPCS Level II code G0477 Face-to-face behavioral counseling for obesity, 15 minutes and the appropriate ICD-9-CM code for BMI 30.0 or over (V85.30-V85.39, V85.41-V85.45). ICD-10 Crosswalk: Z68.30 - Z68.39, Z68.41 - Z68.45
Each IBT for obesity must be consistent with the 5A’s approach adopted by the USPSTF. This approach includes:
- Assess: Ask about or assess behavioral health risk(s) and factors affecting choice of behavior change goals or methods;
- Advise: Give clear, specific, and personalized behavior change advice, including information about personal health harms and benefits;
- Agree: Collaboratively select appropriate treatment goals and methods based on the beneficiary’s interest in and willingness to change their behavior;
- Assist: Using behavior change techniques (self-help and/or counseling), aid the beneficiary in achieving agreed-upon goals by acquiring the skills, confidence, and social or environmental supports for behavior change, supplemented with adjunctive medical treatments when appropriate; and
- Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoing assistance or support and to adjust the treatment plan as needed, including referral to more intensive or specialized treatment.
Effective November 8, 2011, Medicare covered intensive behavioral therapy for cardiovascular disease if the service is provided by a primary care practitioner in a primary care setting such as the beneficiary’s family practice physician, internal medicine physician, or nurse practitioner in the doctor’s office.
Effective November 8, 2011, CMS covered intensive behavioral therapy for cardiovascular disease (referred to below as a CVD risk reduction visit), which consists of the following three components:
- Encouraging aspirin use for the primary prevention of cardiovascular disease when the benefits outweigh the risks for men age 45-79 years and women 55-79 years;
- Screening for high blood pressure in adults age 18 years and older; and,
- Intensive behavioral counseling to promote a healthy diet for adults with hyperlipidemia, hypertension, advancing age, and other known risk factors for cardiovascular and diet-related chronic disease.
We note that only a small proportion (about 4%) of the Medicare population is under 45 years (men) or 55 years (women), therefore, the vast majority of beneficiaries should receive all three components. Intensive behavioral counseling to promote a healthy diet is broadly recommended to cover close to 100% of the population due to the prevalence of known risk factors.
Effective for claims with dates of service on and after November 8, 2011, CMS covers one face-to-face CVD risk reduction visit annually for Medicare beneficiaries who are competent and alert at the time that counseling is provided, and whose counseling is furnished by a qualified primary care physician or other primary care practitioner in a primary care setting.
For the purposes of this covered service, a primary care setting is defined as one in which there is provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community. Emergency departments, inpatient hospital settings, ambulatory surgical centers, independent diagnostic testing facilities, skilled nursing facilities, inpatient rehabilitation facilities, and hospices are not considered primary care settings under this definition.
If you spend fifteen minutes counseling the patient about Cardiovascular Risk, then you can bill the G code for IBT Cardiovascular Disease. As you consider using this code and as you calculate your time invested, do not forget the time you spend counseling the patient about the Framingham Risk Scores and the What If Scenarios, the Cardiometabolic Risk Syndrome, the LESS Initiative, diabetes, hyperlipidemia, obesity, smoking cessation, exercise and nutrition.
The following SETMA tutorials and others will be helpful in this regard:
Metabolic Syndrome Tutorial
Framingham Cardiovascular Risk Assessment Tutorial
Lipids Tutorial
Smoking Cessation Tutorial
To bill for the IBT Cardiovascular Disease, go to the E&M template and click on the appropriate G code as shown below.
A pop-up will appear which asks you to answer three questions.
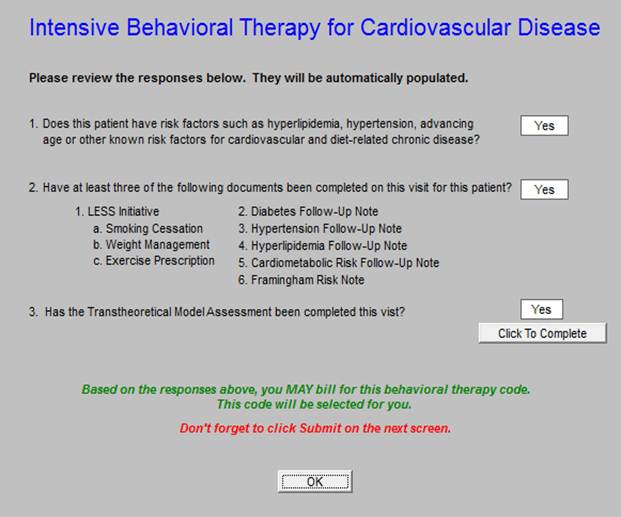
If you answer “yes” to all three questions, you will be alerted to the fact that you can bill for IBT Cardiovascular Disease. Remember, the Transtheoretical Model of Stages of Change must be used in order to bill for the IBT. If you have done so, you can click on the “Click to Complete” button and complete the Model of Change at this time.
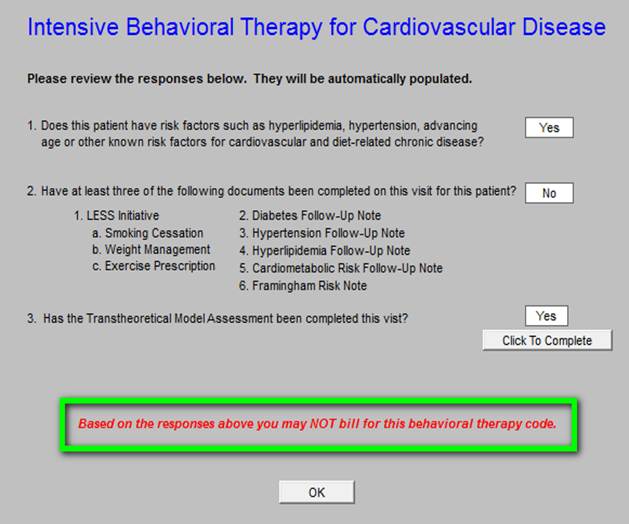
If you answer “no” to either question you will be alerted that you cannot bill for IBT Cardiovascular Disease.
When you complete this process, be sure to click Submit.
G0446 -- Annual, face-to-face intensive behavioral therapy for cardiovascular disease, individual, 15 minutes, will be effective November 8, 2011, and will be included in the January 2012 update of the Medicare Physician Fee Schedule Database (MPFSDB) and Integrated Outpatient Code Editor (IOCE).
The CMS reviewed the USPSTF recommendations and supporting evidence for intensive behavioral therapy for cardiovascular disease and determined that the criteria listed above was met, enabling the CMS to cover this preventive service. Effective November 8, 2011, Medicare will cover intensive behavioral therapy for cardiovascular disease if the service is provided by a primary care practitioner in a primary care setting such as the beneficiary’s family practice physician, internal medicine physician, or nurse practitioner in the doctor’s office.
Effective November 8, 2011, CMS covers intensive behavioral therapy for cardiovascular disease (referred to below as a CVD risk reduction visit), which consists of the following three components:
- Encouraging aspirin use for the primary prevention of cardiovascular disease when the benefits outweigh the risks for men age 45-79 years and women 55-79 years;
- Screening for high blood pressure in adults age 18 years and older; and,
- Intensive behavioral counseling to promote a healthy diet for adults with hyperlipidemia, hypertension, advancing age, and other known risk factors for cardiovascular and diet-related chronic disease.
We note that only a small proportion (about 4%) of the Medicare population is under 45 years (men) or 55 years (women), therefore, the vast majority of beneficiaries should receive all three components. Intensive behavioral counseling to promote a healthy diet is broadly recommended to cover close to 100% of the population due to the prevalence of known risk factors.
Effective for claims with dates of service on and after November 8, 2011, CMS covers one face-to-face CVD risk reduction visit annually for Medicare beneficiaries who are competent and alert at the time that counseling is provided, and whose counseling is furnished by a qualified primary care physician or other primary care practitioner in a primary care setting.
For the purposes of this covered service, a primary care setting is defined as one in which there is provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community. Emergency departments, inpatient hospital settings, ambulatory surgical centers, independent diagnostic testing facilities, skilled nursing facilities, inpatient rehabilitation facilities, and hospices are not considered primary care settings under this definition.
The behavioral counseling intervention for aspirin use and healthy diet should be consistent with the Five A’s approach that has been adopted by the USPSTF to describe such services:
- Assess: Ask about/assess behavioral health risk(s) and factors affecting choice of behavior change goals/methods.
- Advise: Give clear, specific, and personalized behavior change advice, including information about personal health harms and benefits.
- Agree: Collaboratively select appropriate treatment goals and methods based on the patient’s interest in and willingness to change their behavior.
- Assist: Using behavior change techniques (self-help and/or counseling), aid the patient in achieving agreed upon goals by acquiring the skills, confidence, and social/environmental supports for behavior change, supplemented with adjunctive medical treatments when appropriate.
- Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoing assistance/support and to adjust the treatment plan as needed, including referral to more intensive or specialized treatment.
|