|
by James L. Holly, MD
In SETMA’s February, 2015 provider training, we will continue the discussion we briefly had on January 22nd about the benefits SETMA receives from fulfilling a number of quality metrics which are defined by The Healthcare Effectiveness Data and Information Set (HEDIS@). A registered trademark of the National Committee for Quality Assurance (NCQA), HEDIS@ was originally titled the "HMO Employer Data and Information Set" as of version 1.0 of 1991. In 1993, Version 2.0 of HEDIS@ was known as the "Health Plan Employer Data and Information Set". Version 3.0 of HEDIS@ was released in 1997. In July 2007, NCQA announced that the meaning of " HEDIS@" would be changed to "Healthcare Effectiveness Data and Information Set." (HEDIS@) is a widely used set of performance measures which are used by over 90 health insurance programs in order to measure the whether the purchasers of healthcare, generally employers, are getting “their money’s worth” with the services they are buying.
The 75 HEDIS@ measures are divided into six "domains of care":
- Effectiveness of Care
- Access/Availability of Care
- Experience of Care
- Utilization and Relative Resource Use
- Health Plan Descriptive Information
Only the first of these domains is directly dependent upon the healthcare provider’s performance. The HEDIS@ measures for quality performance in effectiveness of care are divided into three categories:
- Effectiveness of Acute Care
- Effectiveness of Preventive Care
- Effectiveness of Chronic Care
Historically, healthcare providers’ care was audited on the HEDIS@ standard by companies hired by insurance carriers who did chart audits to determine how providers were performing. Typically, providers received their results 12-24 months after the audited services were delivered. While the purpose of HEDIS@ was to measure quality, HEDIS@ did not affect quality as very few healthcare providers knew what HEDIS measures were and being published one to two years after the care was delivered, providers largely did not care.
As emphasis on quality and safety increased, and as more and more emphasis was placed on both for the purposes of payment, interest in HEDIS@ and other quality metrics also increased. In 1999, SETMA determined that the only way we were going to sustain improvements in the quality of the care we provide was to measure that quality ourselves. In 2000, we realized that in order to improve we had to know the standard on the basis of which we were being judged. In 2005, we began tracking our performance on HEDIS@ measures internally. In 2009, SETMA began to publicly report by provider name on our performance on HEDIS@ measures.
The following is the rationale for the above. SETMA determined that if we were going to be:
- Given a test
- Where the test questions were going to be given to us before the test
- Where the test is an “open book test”
- Where there is no time limited set on taking the test
Why not look up the answers before the test?
Furthermore, in that the purpose of the test should not only be to evaluate the one being tested but also hopefully to teach the one being tested, it is necessary for the provider to know his/her performance at the point of care. This means that if HEDIS@ is going to affect the quality and safety of the care being given, the provider has to know how he/she is performing on HEDIS@ at the time the care is being given.
The foundation of the quality measurements for ACO payments and for enhanced payments for Medicare Advantage on the basis of the STARS rating system is HEDIS@.
This presentation summaries SETMA’s deployment of all HEDIS@ measures, of HEDIS@ measures for ACO payments, and of HEDIS@ measures for the STARS program. For a detailed explanation of each, see the following links to tutorials on SETMA’s website:
- All HEDIS@ Measures - beginning with page 42 on the following tutorial:
- HEDIS@ Measures related to qualifying for ACO shared savings payments.
- HEDIS@ Measures related to increasing the STAR rating for the Medicare Advantage Plan. Going from a 3.5 to a 4 STAR can mean millions of dollars of increased payments to providers for the care they provide.
SETMA’s Deployment of HEDIS@
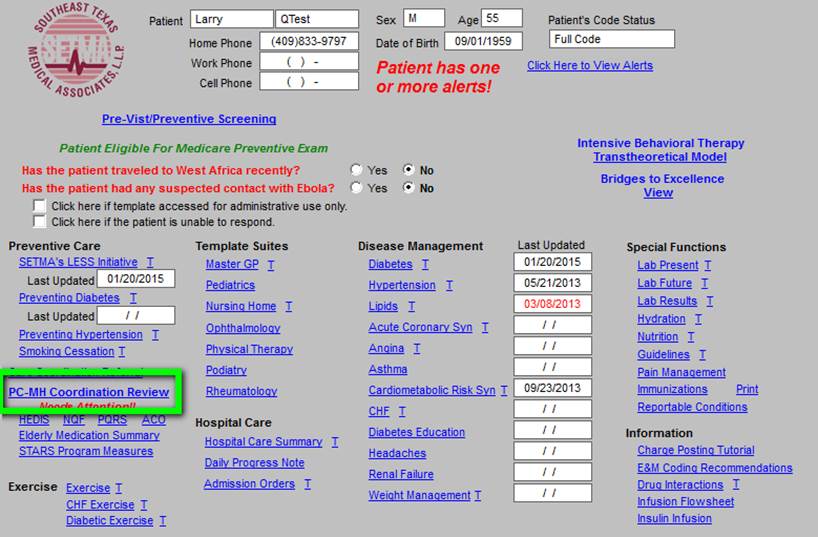
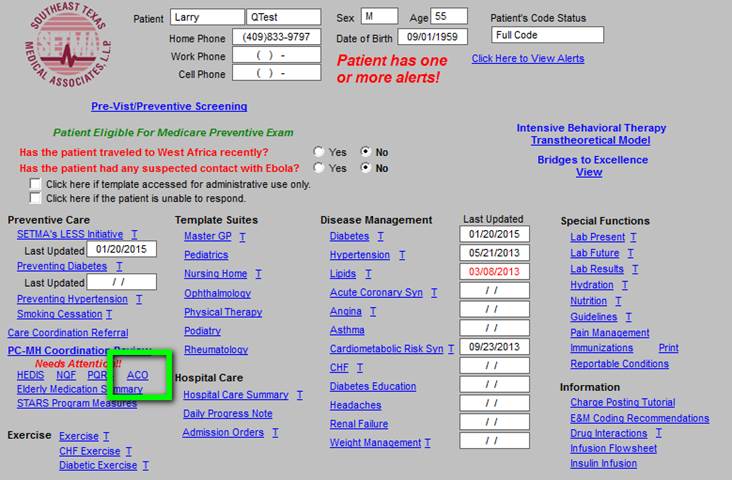
The first screen of SETMA’s Electronic Medical Record is seen below. In the first column is a hyperlink entitled PC-MH Coordination Review (seen outlined in Green below).
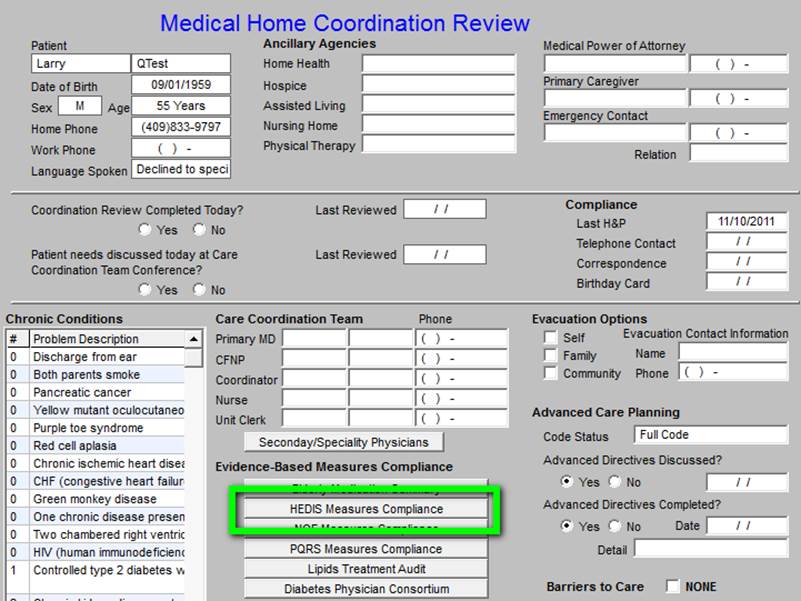
When this link is activated, the Medical Home Coordination Review appears. As indicated above and as seen in the hyperlink outlined in Green below, the full HEDIS@ measure sets is listed here.
If a provider wishes to evaluate his/her own HEDIS@ performance on all measures, it can be done so by clicking this button. If you wish to review all HEDIS@ measures which are dependent upon the healthcare provider, you can do so by accessing this link.
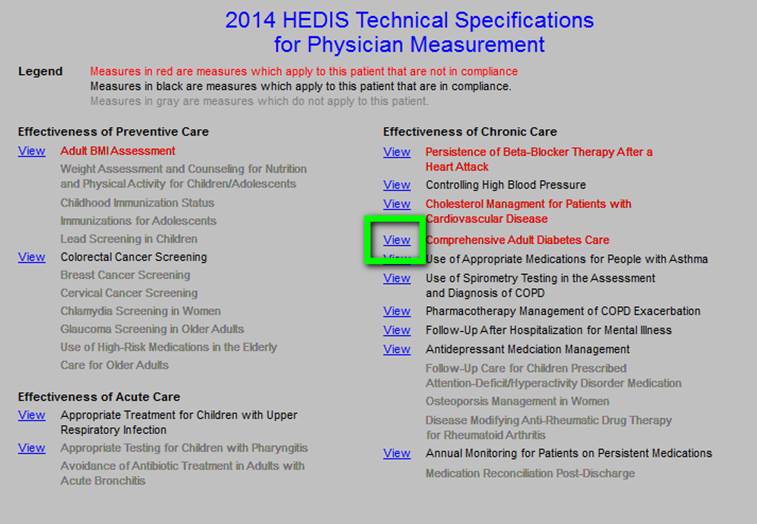
The following is an example of the technical specifications of a HEDIS@ measure. All can be reviewed by accessing each of the measures. To determine whether you have fulfilled HEDIS@ measures you can simple use the color coding: red means the measure applies to this patient and has not been fulfilled; black means the measure applies to the patient and has been fulfilled; grey means the measure does not apply to this patient.
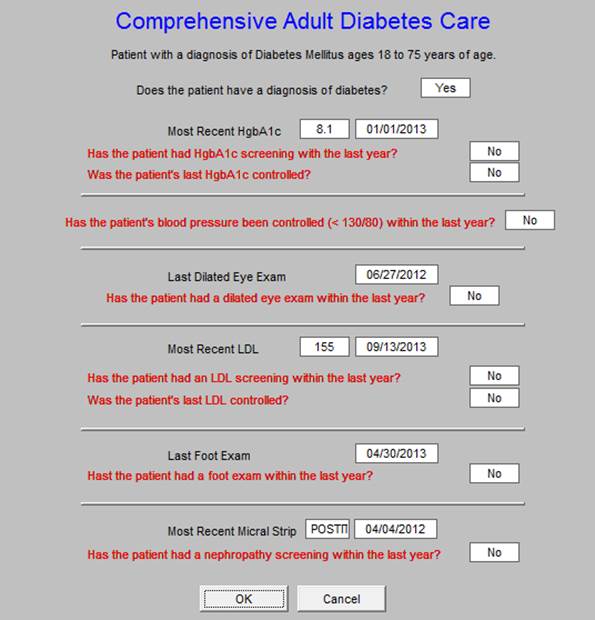
The following is an example of the details of a HEDIS@ measure. To review all of the measures details see above.
ACO HEDIS@ Metrics
To review your performance on the HEDIS@ quality metrics required in order to benefit from the Accountable Care Organziation (ACO) shared-savings plan, you can see the link on the AAA Home Temp;ate below, outlined in green.
Your performance is shown on the template which pops us. The coding is the same: red applies and not done; black applies and done; grey does not apply.
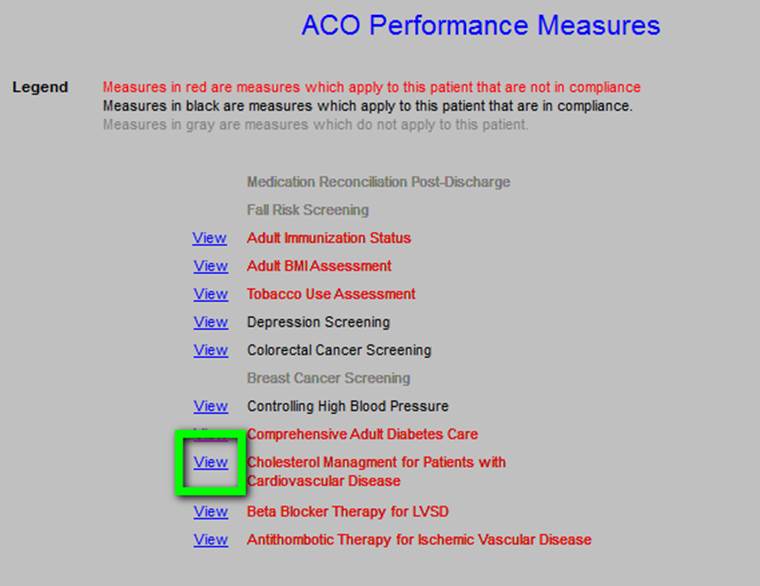
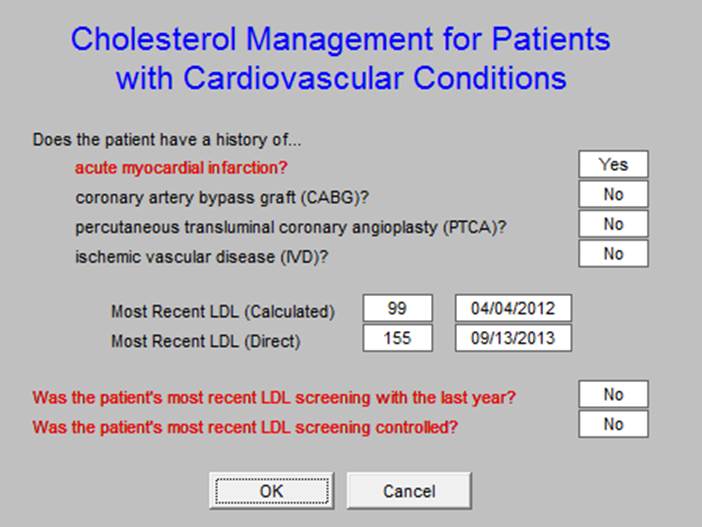
The details of one of the metrics are shown below.
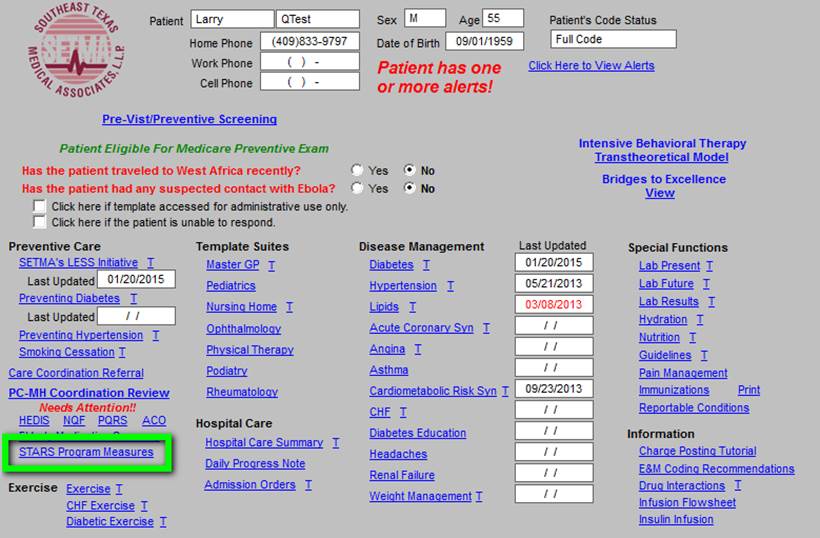
The Medicare Advantage STARS Program quality metrics are launched below by clicking on the hyperlink outlined in green
Overview of STARS Content
The Overall Star Rating combines scores for the types of services each plan offers: What is being measured? For plans covering health services, the overall score for quality of those services covers many different topics that fall into 5 categories:
- Staying healthy: screenings, tests, and vaccines: Includes whether members got various screening tests, vaccines, and other check-ups that help them stay healthy.
- Managing chronic (long-term) conditions: Includes how often members with different conditions got certain tests and treatments that help them manage their condition.
- Member experience with the health plan: Includes ratings of member satisfaction with the plan.
- Member complaints and changes in the health plan’s performance: Includes how often Medicare found problems with the plan and how often members had problems with the plan. Includes how much the plan’s performance has improved (if at all) over time.
- Health plan customer service: Includes how well the plan handles member appeals. For plans covering drug services, the overall score for quality of those services covers many different topics that fall into 4 categories:
- Drug plan customer service: Includes how well the plan handles member appeals.
- Member complaints and changes in the drug plan’s performance: Includes how often Medicare found problems with the plan and how often members had problems with the plan. Includes how much the plan’s performance has improved (if at all) over time.
- Member experience with plan’s drug services: Includes ratings of member satisfaction with the plan.
- Drug safety and accuracy of drug pricing: Includes how accurate the plan’s pricing information is and how often members with certain medical conditions are prescribed drugs in a way that is safer and clinically recommended for their condition. For plans covering health and drug services, the overall score for quality of those services covers all of the topics above.
The following gives the details of the HEDIS@ measures which apply to the MA STARS program.
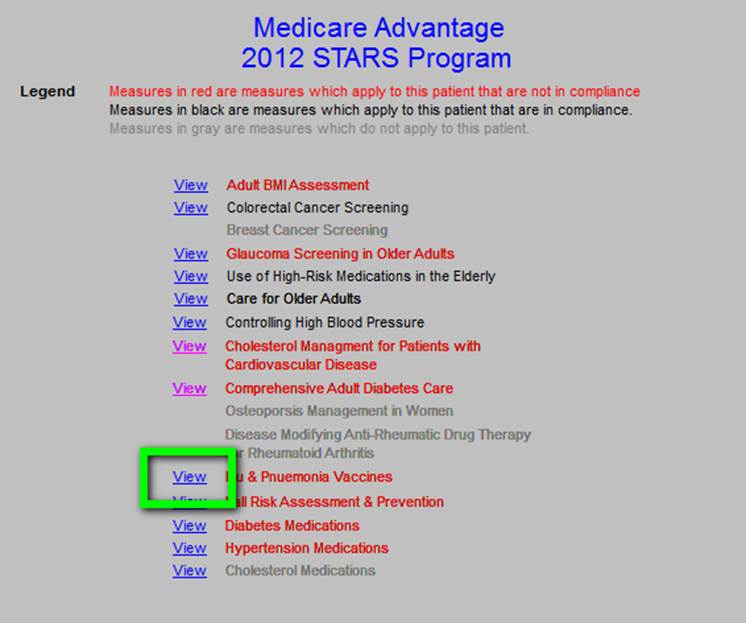
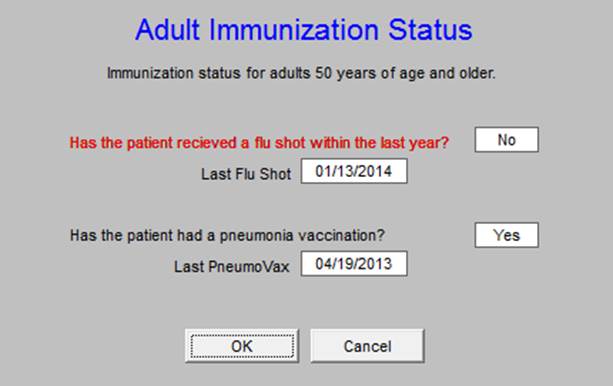
The following is one details of one of the HEDIS@ STARS metrics.
|