www.aqaalliance.org
Introduction
Below is AQA’s description of its mission. After that description is a “Starter Set of Performance Measures” published by AQA as displayed by Southeast Texas Medical Associates, LLP (SETMA, LLP) in our EMR and as reported on our website (www.jameslhollymd.com). AQA is in the process of redefining itself and may be absorbed into other organizations. SETMA has chosen to display these measures because as the process and content of public reporting of quality measures matures, AQA and/or its successor will have been played a significant role and their “Starter Set” will have been a significant step in the process. Our deployment of these measures will help document that history.
Anyone who reviews AQA’s “Starter Set” and compares it to NCQA’s HEDIS measures will see that they are virtually identical. However, the intended uses of the two are different. NCQA’s HEDIS measures are used by health plans as a means of demonstrating to potential buyers of their products that the purchasers will receive quality care. HEDIS results are typically reported retrospectively and generally with a significant delay between the care delivered and the assessment and evaluation of the quality of that care. AQA on the other hand intends that their measurement set will be used in the ambulatory care setting to set a standard for ambulatory care where the overwhelming majority of care is received with the intent to improve the quality of that care. The former is measuring outcomes, while the latter desires to affect the process.
SETMA has developed the ability and is presently using that ability for healthcare providers to employ in the clinical practice of medicine, at the point of care and at the time of care, measurement sets published by:
- The American Medical Association’s (AMA) Physician Consortium for Performance Improvement (PCPI)
- The National Quality Forum (NQF) through its endorsement of quality measures
- The National Committee for Quality Assurance (NCQA) through its HEDIS measures program
- Centers for Medicare and Medicaid Services (CMS) through its Physician Quality Reporting System (PQRS).
- Ambulatory Care Quality Alliance (AQA) through its Starter Set of Performance Measures.
After AQA’s self description, you can review SETMA’s deployment of the “Starter Set” below.
AQA’s History and Mission
In September 2004, the American Academy of Family Physicians (AAFP), the American College of Physicians (ACP), America’s Health Insurance Plans (AHIP), and the Agency for Healthcare Research and Quality (AHRQ), joined together to lead an effort for determining, under the most expedient timeframe, how to most effectively and efficiently improve performance measurement, data aggregation, and reporting in the ambulatory care setting.
Originally known as the Ambulatory Care Quality Alliance, the coalition is now known as the AQA alliance because its mission has broadened to incorporate all areas of physician and other clinicians practice.
The AQA is a large voluntary multi-stakeholder collaborative of physicians and other clinicians, consumers, purchasers, health plans, and others who strive to meet its responsibilities in an effective, efficient, public and transparent manner. The mission of the AQA is to:
- improve patient safety, health care quality and value in all settings through a collaborative process in which key stakeholders agree on and promote strategies to:
- implement performance measurement at the physician and other clinician or group level;
- collect and aggregate data in the most appropriate way; and
- report meaningful information to consumers, physicians and other clinicians, and other stakeholders to inform decision-making and improve outcomes.
The goals of the AQA in 2009 are to:
- Achieve full and active engagement of all AQA constituencies and serve as a catalyst for change as an open forum to exchange ideas and experiences across the broad community of stakeholders.
- Focus all efforts on quality improvement, affordability, efficiency, and accountability, and actively promote the role of measurement to drive those goals.
- Position the AQA as an active and critical resource to its members, other organizations within the quality enterprise, and policy-makers by providing continuous feedback to developers and endorsers on the implementation experience.
AQA’s mission and goals focus on key areas that can help identify quality gaps, control skyrocketing cost trends, reduce confusion over redundant measures and alleviate administrative burdens in the marketplace.
SETMA’s Deployment of AQA’s Starter Set
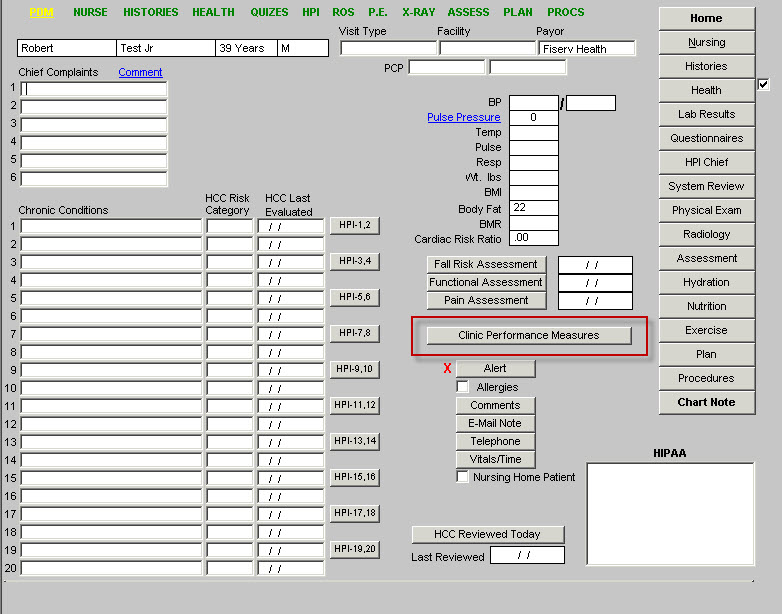
The following is SETMA’s Master Template for ambulatory care. As can be seen, the button outlined in Red is entitled “Clinical Performance Measures.” When depressed this button launches a second template with the same name. The “Clinical Performance Measures” are AQA’s “Starter Set of Quality Measures.”
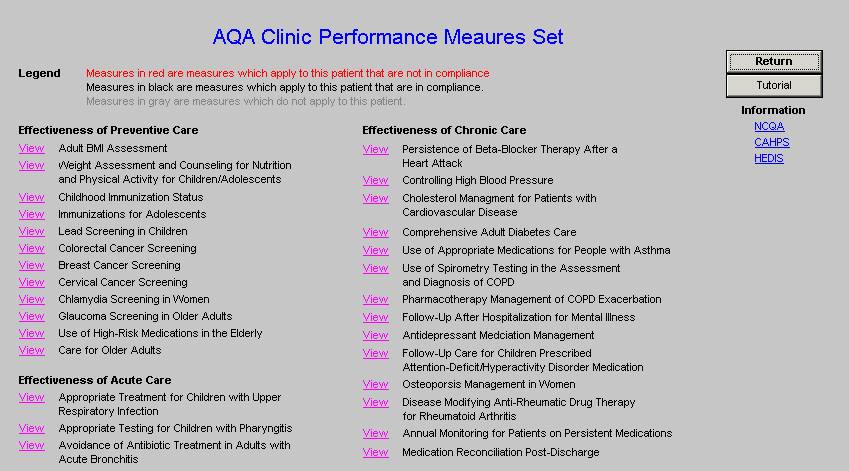
The legend on the second template describes the function of the template which aggregates data from a patient’s encounter to determine if the “Clinical Performance Measures have been met. Measures in black apply to this patient and are fulfilled. Measures grayed out, do not apply to this patient. Measures in red apply to this patient and have not been fulfilled.
If a measure has not been met, the hyperlink entitled “view” can be accessed in order to determine what is required in order to fulfill this particular quality measure.
It is SETMA’s hope and intent that with these quality measurement sets being reviewed at each patient encounter that the quality of care will improve. In addition, with SETMA’s COGNOS project, the auditing and public reporting of provider performance will further motivate improvement in care.
This is another step in SETMA’s mission to “transform healthcare through the power of information and through the power of auditing.”
|