|
HCC RxHCC Risk Tutorial for SETMA
Table of Contents
Introduction to HCC & RxHCC Risk Categories; HCC & RxHCC Coefficients; E&M Codes and Correlation with aggregate HCC & RxHCC Coefficients for Acute Diagnoses; and General Concepts about HCC/RxHCC
In 2007, Medicare Advantage programs (HMO) were funded by CMS (Center for Medicare and Medicaid Services) using both demographics and the Hierarchical Conditional Codes, known as the HCC Diagnoses. 2007 also was the year that RX HCC codes were added to complement the reimbursement for managing patients with illnesses, which while they did not rise to the level of complexity and cost-for-care, as the HCC diagnoses, they did qualify for a lower additional payment due to increased medication costs.
In the interim, the use of HCC and RxHCC designation has been expanded to include not only Medicare Advantage beneficiaries, but also Medicare Fee-for-service beneficiaries through Accountable Care Organizations (ACO) and patients treated in a Medical Home. In the case of the ACO, the savings for the calculations of shared savings will be determined by actual cost of care measured against the benchmark costs including the HCC and RxHCC factor for the patients in the benchmark. In the case of Medical Home, the payment of the per member per month (PMPM) payment will be calculated with the level of Medical Home recognition and the HCC/RxHCC coefficient aggregate value, i.e., if a patient is being treated by a Tier III Medical Home and the aggregate HCC/RxHCC score is 2.0 or above, the provider would be eligible for the maximum PMPM as determined by contract.
RxHCC
The RxHCC designations cover many diagnoses which were not covered in the HCC. As a general rule almost all HCC diagnoses are also RxHCC codes but all RxHCC are NOT also HCC. Here are some examples of diagnoses which are not HCC but are RxHCC codes:
- Hypertension is not an HCC (i.e., 401.1 or 401.9, etc) but it is an RxHCC
- Osteoporosis another common illness is not a medical HCC but is an RxHCC
- CAD in itself is not a medical HCC, but it is an RXHCC. Because CAD is a general term, it is imperative that if the patient has angina or an old MI, the chronic problem list should include angina or old MI as they are HCC diagnoses.
Let’s start from the end and work our way back to the beginning. Because all of the HCC and/or RxHCC are Chronic Conditions, the following would be required:
- They must be identified in the E&M coding event for that encounter and they must appear on the Chronic Problem list for that patient.
- Lab, x-rays and procedures should be appropriate to that condition, when required.
- Medications should be reviewed and appropriate medications for the condition should be present in the documentation for the encounter. (It is possible in NextGen to associated a medication with a diagnosis. We will have our staff complete this task on all GTPA patients.)*
- Physical examination should be specific for that condition - for instance if you state the patient has CHF and do not document the lungs and heart, it would not be a valid evaluation. If you say the patient has cancer of the prostate and you do not comment whether they are currently in treatment or are in surveillance, that would not be valid.
- Documented History should be appropriate for that condition.
Because HCC and/or RxHCC are chronic conditions, a chief complaint is not necessary, unless it applies. There are four ways in which to complete your documentation in the EMR to satisfy this need.
- Through the routine use of Master GP and the documentation functions present there.
- Through the use of the Chronic-Problem evaluation templates which launch from the Master GP
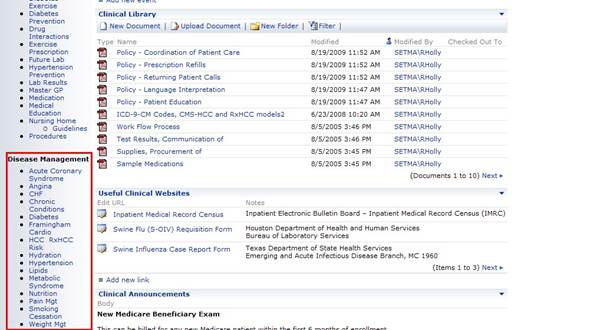
- Through the use of the Disease Management tools in the EMR
- Through the use of the “Detailed Comments” function which launches from the Assessment template by clicking the button entitled “Detailed Comments” which is found in the second column of the Assessment template.
The diagnosis must be:
- Established as applying to this patient.
- Documented in the patient’s record in the Chronic Problem list
- Evaluated at least once in the year prior to the qualification as an HCC or RxHCC
- Reported to the HMO and via the HMO to CMS
Providers simply need to pay attention to the needs and condition of the patient and:
- Add any HCC or RxHCC which you diagnose to both your chronic problem list and to the acute assessment.
- Update your Chronic Problem list so that the HCC and RxHCC are displayed on your diagnoses.
- Evaluate each of the HCC and RxHCC at least once during the year.
- The best way to evaluate whether you have identified ALL of the HCC and/or RxHCC is to review:
- Scanned documents particularly under cardiology, master discharge summaries, radiology, specialty correspondence, pulmonary, echo’s, x-rays, etc.
- The patient’s past history template
- Laboratory results and medications
- Previous encounters
.
Going forward, once this “catch-up” task is done, it will be relatively easy to add
HCC and RxHCC to your chronic problem list as you sign off on reports, correspondence, etc. Also, we are carefully updating all HCC and RxHCC for all patients admitted to the hospital. This is an on-going task. In 2009, some of the HCC and RxHCC will change and some new ones will be added. We will update our system with that information to continue to make it “easier to do it right than not to do it at all.” As mentioned earlier, our support staff will go through the EMR with all HMO patients and associated the diagnoses (ICD-9) codes with the medications which are used to treat the patient.
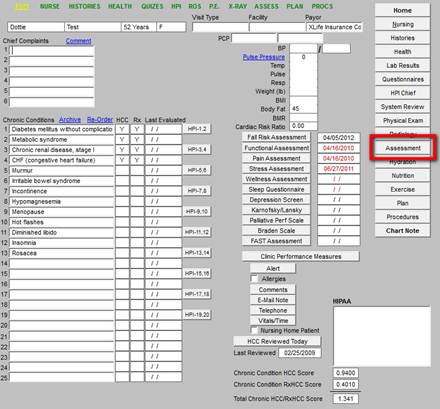
To review the HCC/RxHCC tool in SETMA’s EMR, go to AAA Home
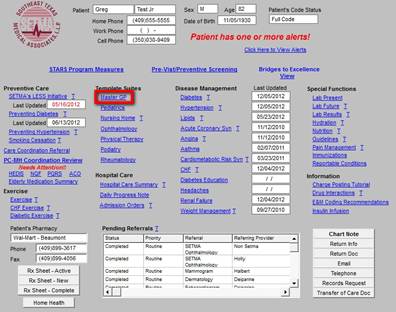
Click on Master
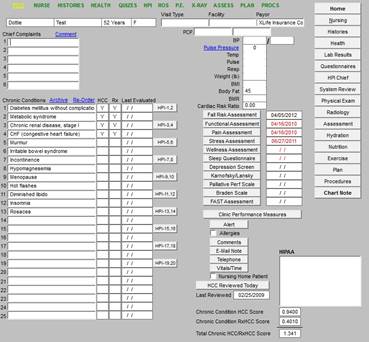
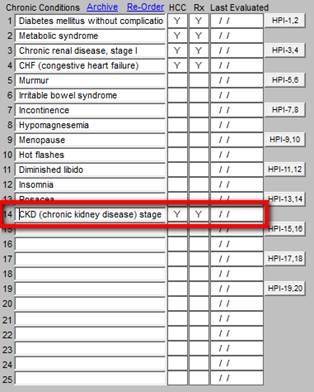
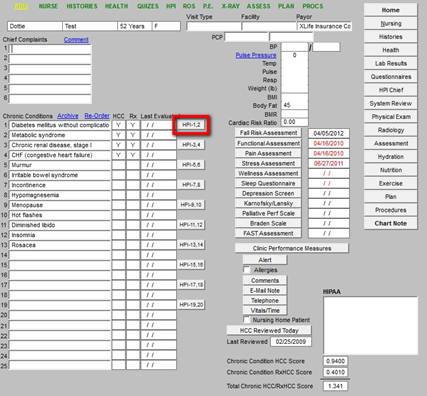
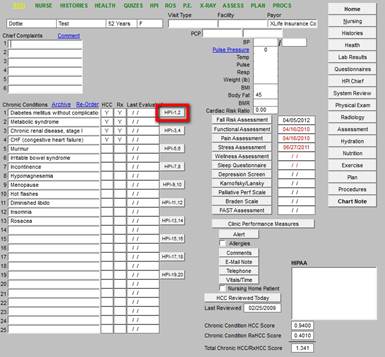
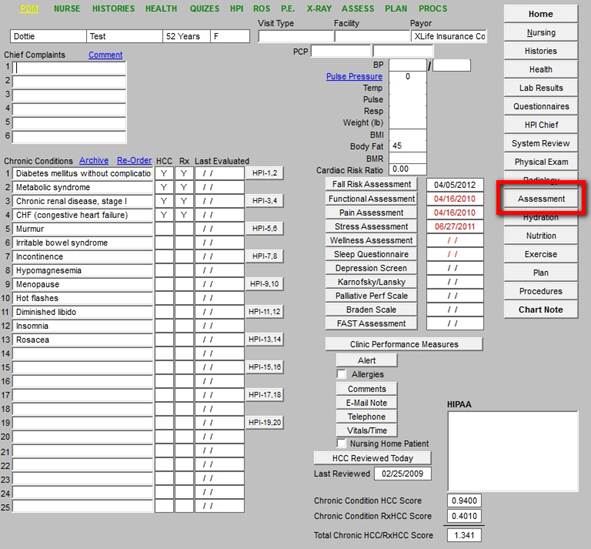
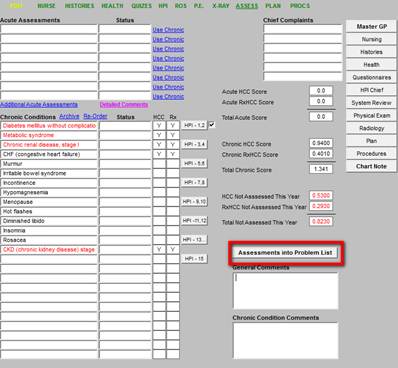
Midway down the GP Master template, you will find the list of Chronic Conditions
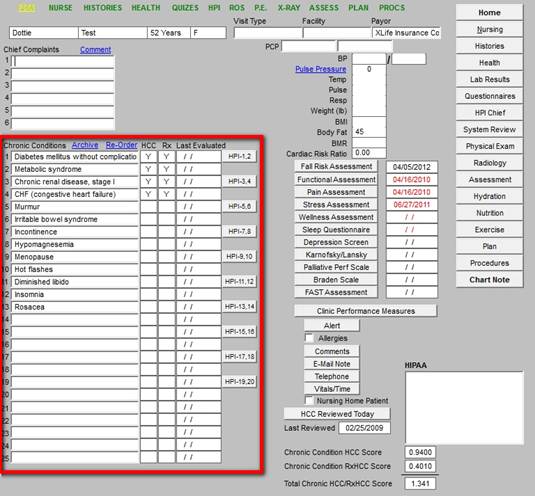
To the right of the Chronic Conditions are four columns entitled:
- HCC Risk Category - this designates that a diagnose is an HCC,
- RxHCC Category - this designates that the diagnoses is an RxHC. (Note: Most HCC diagnoses are also RxHCC, but not all; while most RxHCC are not also HCC.)
- Last Evaluated - this designates the date when this problem was specifically evaluated.
- HPI 1-2, HPI 3-4 etc. - this provides a template whereby the provider can specifically address each of the diagnoses in the Chronic Problem List.
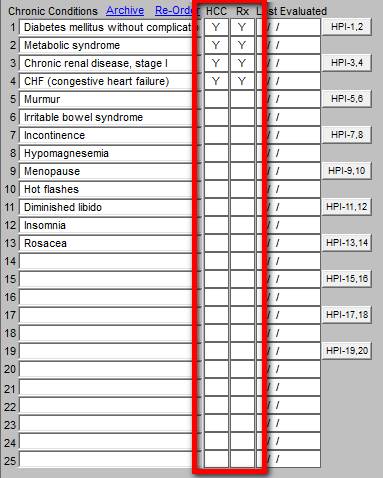
If the diagnosis is an HCC code, the first column, entitled HCC, “Y, If the column is blank, the diagnosis is not an HCC Risk. The designation appears automatically when diagnosis is selected from IMO’s code list. If the diagnosis is an RxHCC, a “Y” will appear in the second column entitled, “Rx.” If the second column is blank, then the diagnosis is not an RxHCC code.
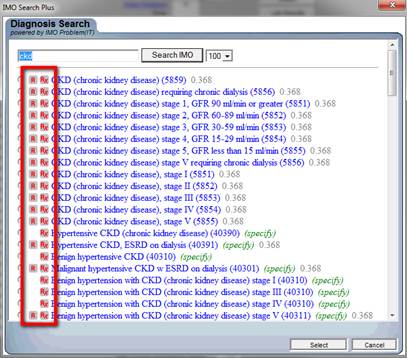
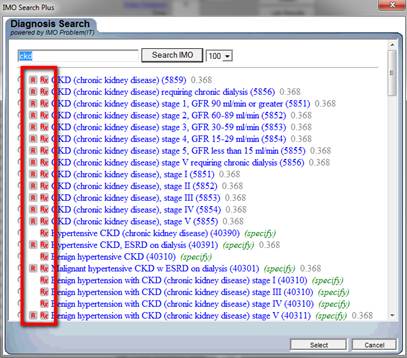
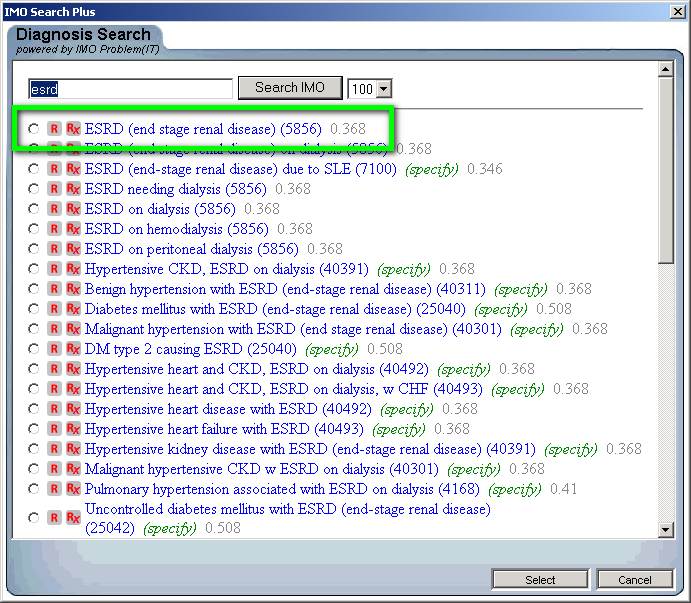
When the IMO ICD-9 Code list, and in 2014, the ICD-10 code list is accessed, the following screen will appear. To the left of the diagnosis, are the designations of “HCC,” which is denoted by the presence of an “R” and the designation of an “RxHCC” by the “Rx” in the second column.
To the right of the diagnoses is a number. This is the “coefficient’ for that HCC or RxHCC diagnosis. The coefficient reflects the increased payment which will be earned by the treatment of patients with these diagnoses. In the section below on HCC and RxHCC coefficients, this will be discussed in more detail. You may go to that section by clicking here.
When you select a diagnosis, if it is either HCC or RxHCC, that designation is automatically placed into the columns entitled “HCC” and “Rx.”.
The HCC/RxHCC designations appear on the:
- Master GP
- IMO’s code list where the HCC and RxHCC are displayed beside diagnoses.
- Assessment Template
- Plan Template
- “Assessment into Problem List Pop-up” (see below for how to use this function)
When you open the IMO function, you will see a list of diagnoses based on the abbreviation you typed or the name you typed in the assessment or chronic condition space. When that list is displayed, you can either select a diagnoses by clicking in the space to the left of the diagnosis. This will place the diagnosis in your record.
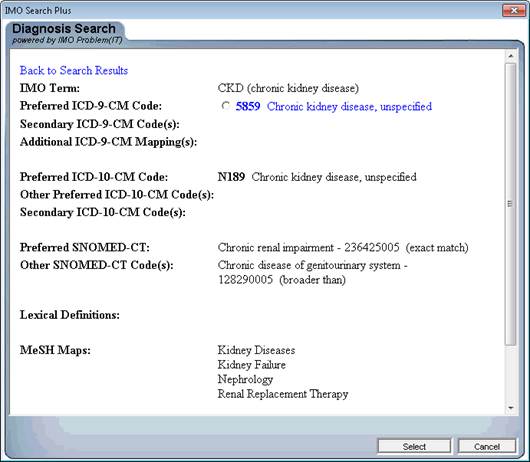
Or, you can click on the diagnosis itself which will launch the following window. This will tell you what the ICD-10 code would be for this ICD-9 Code and it will tell you what the SNOMED diagnostic name will be. In 2014, we will begin using the ICD-10 codes and in 2015, we will begin using the SNOMED nomenclature. Both are already built into the IMO program.
Note: SNOMED CT (Systematized Nomenclature of Medicine--Clinical Terms) is a comprehensive clinical terminology, originally created by the College of American Pathologists (CAP) and, as of April 2007, owned, maintained, and distributed by the International Health Terminology Standards Development Organisation (IHTSDO), a not-for-profit association in Denmark. The CAP continues to support SNOMED CT operations under contract to the IHTSDO and provides SNOMED-related products and services as a licensee of the terminology.
At the bottom of the GP Master, you will see a button entitled “HCC Reviewed Today”.
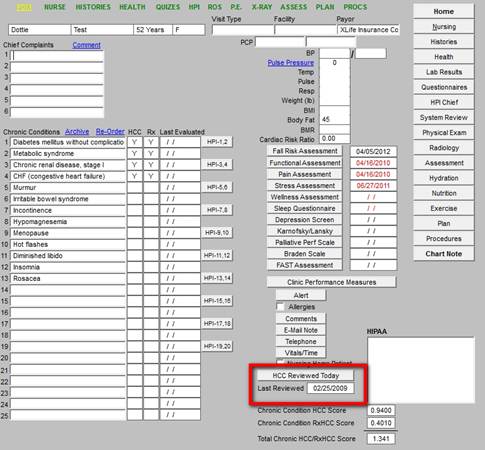
This button and the date beside it, gives you the opportunity to denote when you last did a thorough review of the patient’s entire record and identified all of the HCC and RxHCC codes which apply to this patient. When you click on the button, a pop-up appears which states:
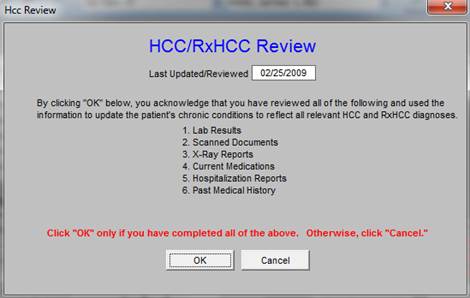
If you have gone through the patient’s entire record, identifying and validating all HCC and/or RxHCC diagnoses, then you may click “OK” and it will indicate to day’s date as when you last checked that patient’s chart thoroughly for HCC and/or RxHCC diagnoses. The following will further support the accurate identification, validation and verification of HCC/RxHCC codes:
- These charts will be reviewed at least once a year by our support staff and in some cases they will be reviewed more often.
- Every time a patient is in the hospital, the HCC/RxHCC lists will be updated.
- When you received correspondence from specialist or the results of procedures, you should update the HCC/RxHCC according to the validated and verified diagnoses.
With these steps the accuracy and completeness of SETMA’s HCC and RxHCC Coding will be supported and sustained by:
- Provider attention to the ICD-9 Codes they select during a patient encounter.
- Providers adding additional diagnoses when they review tests and procedure results such as lab work, echo reports, etc.
- Hospital Service team adding diagnoses to the chronic problem list when a patient is discharged from the hospital.
Four steps are needed to meet the requirement to have CMS recognize a diagnosis as an HCC or RxHCC code in the treatment of your patient; they are:
- Establish that this diagnosis applies to this patient. There are several steps to this process: identify the diagnoses, verify, and validate it.
- Document the diagnosis in the patient’s record in both the encounter assessment for the day in which it was added and in the Chronic Problem list on the patient’s chart.
- Evaluate the problem at least once in the year prior to its qualification as an HCC or RxHCC. i.e., evaluate the problem in 2008 for inclusion as an HCC or RxHCC in 2009. Remember, there are four ways in which you can support your evaluation of each problem:
- By use of the Chronic Condition evaluation templates which launch from the Master GP
- By use of the Disease Management Tools which launch from AAA Home.
- By use of the “Detailed Comment” function which launches from the Assessment Template by clicking the button entitled “Detailed Assessment” in the second column of the Assessment template.
- By use of the Master GP Functions in a routine evaluation making certain to address history, physical, assessment, lab and procedures which relate to a particular problem.
- Report the diagnosis to the HMO and, via the HMO to CMS
The steps described above fulfill the requirements for steps one and two. The third step (Evaluate the problem at least once in the year prior to the qualification as an HCC or RxHCC) is met by using the two other columns which appear next to the Chronic Problem List and which are entitled “HCC Last Evaluated” and “HPI 1-2”
In order to qualify as an HCC or RxHCC diagnosis, your evaluation must have:
- a history (most often contained in the review of systems) and
- a physical examination relating specifically to that particular problem.
In addition, when it is appropriate:
- laboratory test and/or
- other procedures should be done at appropriate intervals,
- along with any consultations or
- treatments documented.
Finally, your evaluation should document:
- The diagnosis’ status
- Medications ordered, reviewed or changed
Of course, these are steps you already take in treating a patient.
There two ways in which the third column, entitled “Last Evaluated,” can be populated; one is manual and the other is automatic.
Manually, you can add the date of the encounter in which you completed a patient evaluation, which gave attention to the history, physical, lab and procedures related to a specific HCC or RxHCC.
Simply click in the space in the “HCC Last Evaluated” column, next to the Chronic HCC or RxHCC condition you have evaluated. A pop-up will appear which states:
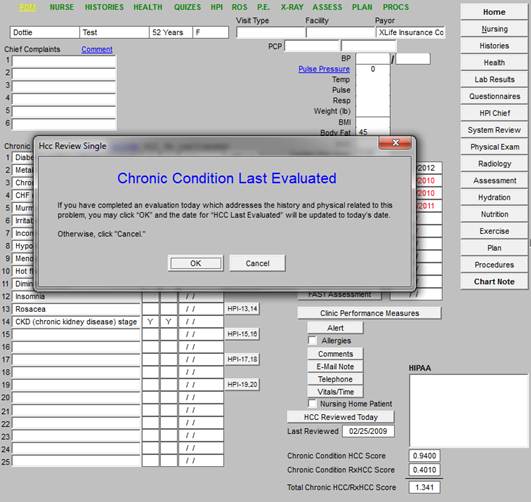
If you have not completed an evaluation which is specific to this diagnosis, click “cancel” and either evaluate the problem another day, or complete the evaluation on this date; then return to this field to denote your work.
Once you have clicked “OK,” today’s date will be added indicating that this problem was evaluated today.
NOTE: Soon, another function will be added such that when you complete this step, the ICD-9 Code associated with the HCC/RxHCC which you evaluated will be added to your E&M Template for this visit.
The “HCC Last Evaluated” field can be automatically added if you use the Chronic-Condition-evaluation pop-up, which is launched by clicking in the third column, which is entitled, “HIP 1-2” etc. In addition, when you use this function that Chronic Condition will automatically be added to your E&M Evaluation.
The Chronic Conditions Evaluation Functions are found to the right of the Chronic Conditions as displayed on the Master GP template.
When you click the HPI button in the fourth column next to the Chronic Conditions, the pop-up will have two Chronic Conditions on it.
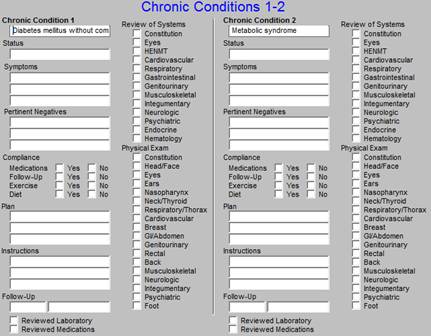
You may evaluate one or both of these chronic problems. There is some redundancy which cannot be eliminated in the use of this function but it will make certain that your evaluation is specific to the problem with which you are dealing and that you have fulfilled the requirements for evaluating this problem.
The pop-up has a place for you to address the following elements of the Chronic Condition under consideration:
- Review of Systems
- Physical Examination
- Status
- Symptoms
- Pertinent Negatives
- Compliance
- Plans
- Instructions
- Follow-up
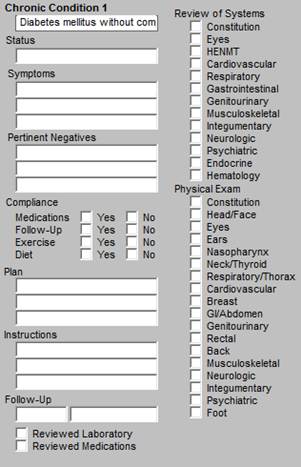
The ROS and Physical Examination which you completed under the GP Master functions will automatically populate the Chronic Conditions evaluation function and will appear on your note for each of the systems you open in your evaluation of a Chronic Problem.
Soon, If you use the Chronic Condition evaluation function, each of the Chronic Conditions you so document will automatically be added to your E&M code without your having to do anything else.
SETMA has designed Disease Management Tools for:
- Angina
- Asthma
- Headache
- Lipids
- CHF
- Hypertension
- Cardiometabolic Risk Syndrome
- Weight Management
- Chronic Renal Disease
- Weight Management
The use of any of these Disease Management Tools will provide all of the documentation which is required to satisfy the evaluation of an HCC or RxHCC.
Once the disease management tool is completed for any of these conditions, the provider can manually update the “HCC Last Evaluated” with confidence. Eventually, we will have that update be automatic. Tutorials for each of the Chronic Disease Management Tools can be found one of three ways:
- Clicking on the “T” next to name of the Disease Condition on AAA Home
- Or by going to SETMA’s Intranet and clicking on “Clinical.” Click Here.
- If you would like to study any of these Tutorials from a book, you check one out for loan for two weeks.
The “Detailed Comment” was developed for the Hospital-daily-progress-note function in NextGen, but is also available to be used with the clinic note. At present, there are sixteen conditions for which we have developed “categories” for evaluation of chronic conditions.
To find the “Detailed Comment” function, go to the Assessment Template in the Master GP Suite of templates by clicking on Assessment in the SETMA navigation list.
This step launches the Assessment Template. At the top of the second column of this template, there is a button entitled “Detailed Comments”.
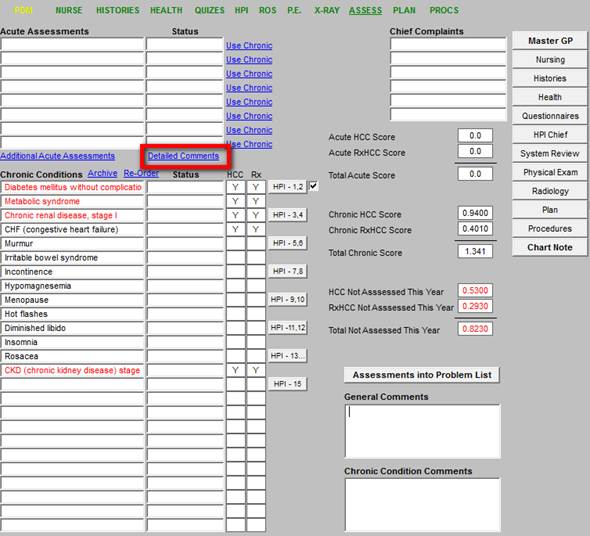
Depressing this button launches the following screen:
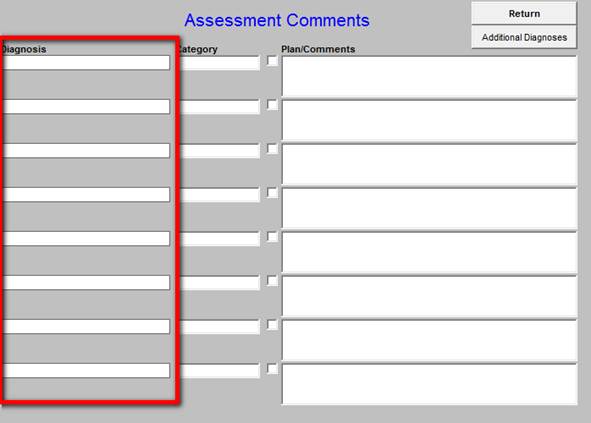
In the left hand column, the conditions on the Acute Assessment of the current encounter will appear. If there are more than 8 diagnoses, the additional ones can be found by clicking on the “Additional Diagnoses” button at the top right of the template
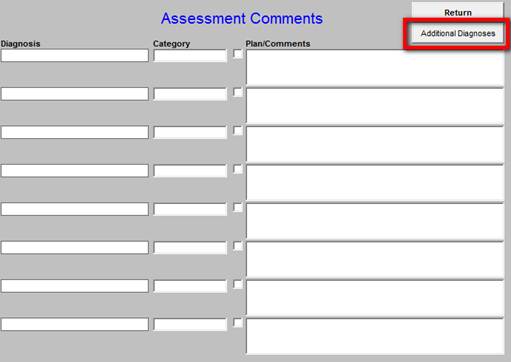
Under the title “Categories”, if you click in the empty box beside the diagnoses you wish to evaluate for an HCC or RxHCC, you will launch a pop-up with the current 16 conditions for which the evaluation tool exists.
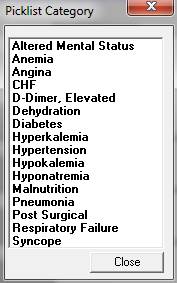
If you then select the “Category” which corresponds with the HCC or RxHCC diagnoses which you are evaluating, a template will appear which will allow you efficiently to complete the evaluation of the condition.
For instance, if you are evaluating Diabetes, and if you click on the diagnosis of Diabetes in the list of conditions under “Category,” the following will appear:
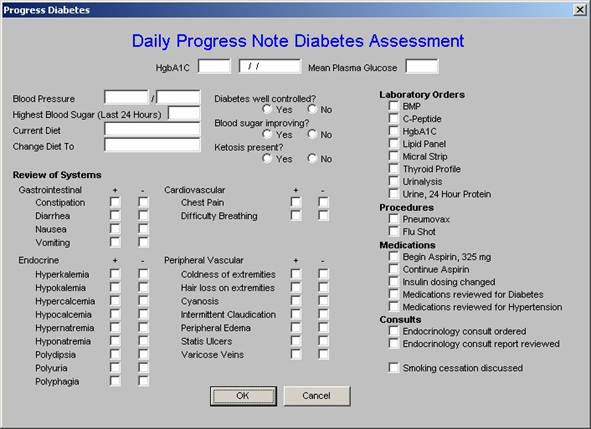
You can then quickly and effectively evaluate that problem and that evaluation will appear on your chart note. Also the ROS section will be automatically populated with your previous ROS, as will the vital signs and the appropriate laboratory results.
Having completed the evaluation of this “category,” you can return to the Master GP template and put today’s date in the “HCC Last Evaluated” box. Eventually, we will make that notation automatic as well.
If there are multiple HCC or RxHCC codes which you wish to evaluate; you just repeat this process for each one.
It is obvious that it is possible to do a global evaluation of a patient utilizing the elements of the Master GP suite of templates. Such a global evaluation, if it contains the elements of history, physical, assessment and plan for each of the HCC and/or RxHCC codes, will suffice for the requirement of documenting such an evaluation.
Introduction
In NextGen’s Medication Module, it is possible to associate the patient’s medications with the specific diagnosis for which the medication is prescribed. Some day, I suspect, the standard of care in medicine and perhaps even the law of medicine will require this to be done.
The idea behind RxHCC is that the conditions so designated have an increased cost of care because of the chronic need for one or more medications to treat the condition.
One of the problems with this association, as far as the functionality of NextGen is that once the visit in which the medication prescribed is locked, in order to create this association, you must renew the medication.
Thus, it is helpful, when it is possible, and I understand and accept the fact that we are already asking for a great deal to be added to your workflow, it is ideal to make this association at the time that you add a medication for the treatment of an HCC or an RxHCC diagnosis.
Steps to Completing the Association of a Medication with a Diagnosis
From the Master GP template, click on the Assessment button in SETMA’s list of navigation buttons.
At the second column on the Assessment template midway down the screen, you will see a button entitled “Assessments Into Problem List.”
When you click on the “Assessments Into Problem List” button, the following screen appears:
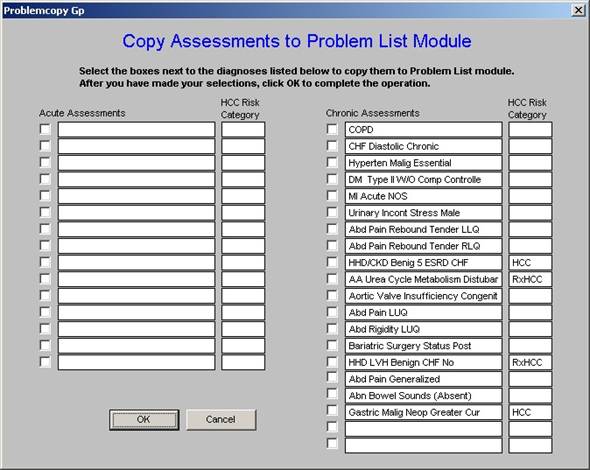
As you can see this displays both the Acute Assessments and the Chronic Problems and identifies the diagnoses which are HCC and RxHCC, as well as those which are not, in this last case by the absence of a designation.
At the top of the pop-up which is launched by this step, which is entitled “Copy Assessments to Problem List Module”, you will read the following note:
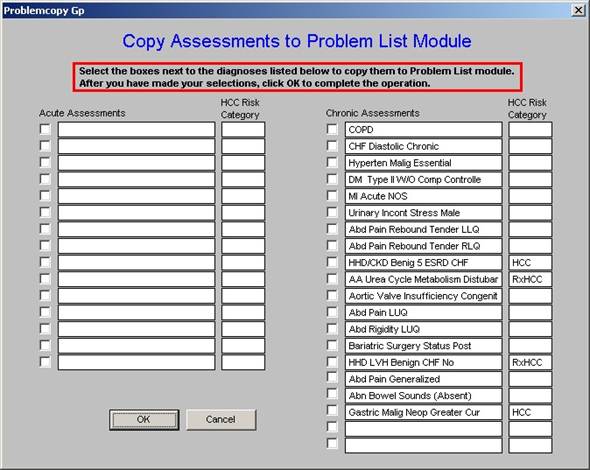
In order to increase efficiency, I would recommend transferring only HCC and RxHCC diagnoses to the Problem List Module. Once you have done this, you can review the Problem List Module by clicking on the center icon at the right hand bottom of the Main Tool Bar. This is the icon which has a “scroll with Dx” in the center of it.

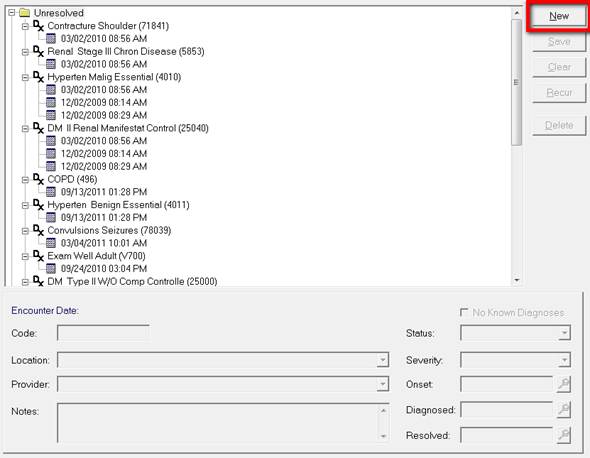
When you click on this icon, it will display your Diagnostic Problem List.
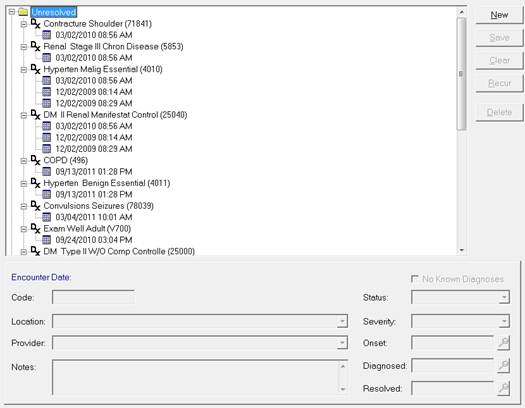
There are two categories on this list: unresolved and resolved. There are also five buttons to the right of the screen:
- New - this allows you to add a diagnosis as a new problem from this function but I recommend the custom solution SETMA has devised.
- Save - this makes your selection permanent
- Clear - this removes the status, severity, onset, diagnosed, resolved field at the bottom right of the Problem List template
- Renew - this is used to reactivate a problem from the “resolved” column to make it “unresolved” again
- Delete - this deletes a selected diagnosis from the Problem list.
Once you understand the function of the Problem List feature, you are ready to take the step of associating medications with the problem for which they were prescribed.
Click on the Medication Module icon, which is the bottom left icon of the nine icons at the bottom of the Main Tool Bar.

In the top window, you will see a list of the medications the patient is on. At the very bottom, you will see a window which is entitled “Problem.”
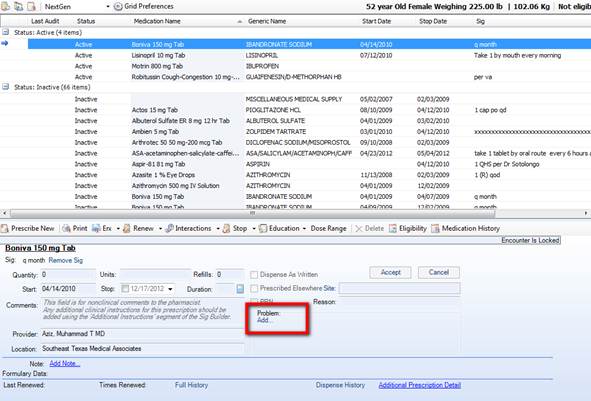
If the visit in which that medication was prescribed is not locked, just below “Problem” there will be an “Add” followed by an ellipsis (this is the three dots in a row, such as €¦).
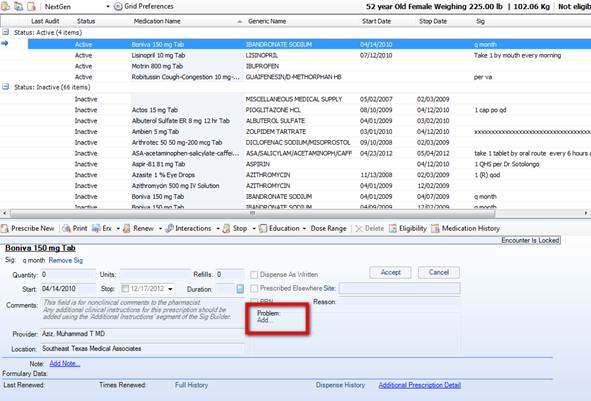
If the ellipses is not present, click on the “Renew” medication button and the ellipses will appear.
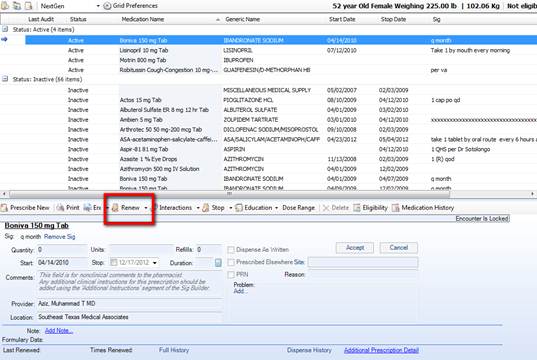
Click on the ellipses button and a the patient’s problem list will appear to the left.
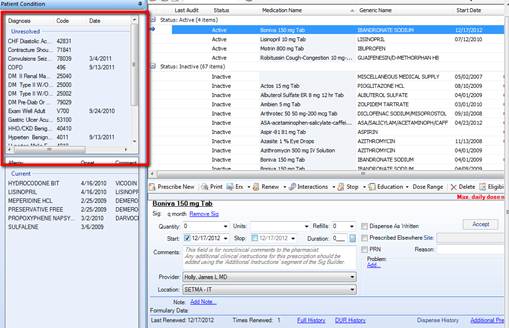
Find the diagnosis which is being treated by this medication and double-click it. You may select more than one if you like. You will see that diagnosis appear in the Problem window.
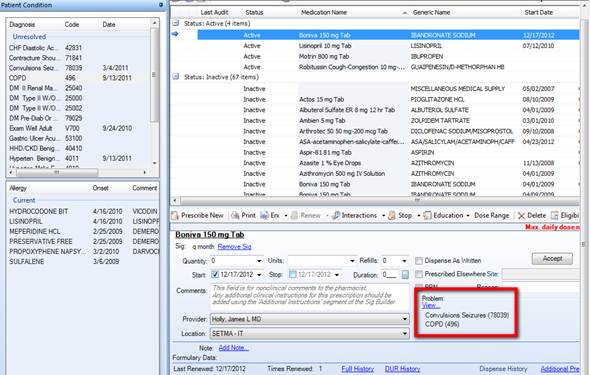
We are able to report this information and with it completed in the EMR, it will make an audit on HCC and/or RxHCC, so far as the medications are concerned, a breeze.
HCC and RxHCC Code Coefficients Definition: the HCC and RxHCC coefficients are a numerical designation by CMS of the relative value of a particular ICD-9 code. In general, when the coefficients are used for payment, a total of 2.0 or higher is where the greatest value is gained.
HCC and RxHCC code documentation and analysis are important for a number of reasons:
- In Medicare Advantage programs, the patient care given become eligible for enhanced payments based on these scores. In that patients such as ESRD and Renal Dialysis are treated at a loss by the MA programs, a loss which can be several thousand dollars a month per patient, it is important to recover as much of that revenue as it possible, in order to make the programs viable.
- In ACOs, risk stratification, such as HCC and RxHCC will be considered in the calculation of revenue savings.
- In the CMS study in which SETMA recently participated, Fee-for-Service Medication beneficiaries cost-of-care calculations were made with risk adjustment by HCC and RxHCC.
- The payment model for care coordination in the Medical Home Model of Care for FFS Medicare will be calculated on the basis of the standard of Medical Home achieved, i.e., Tier 1, 2 or 3, and whether or not the aggregate of the HCC and RxHCC coefficients total 2.0 or higher.
For an explanation of HCC and RxHCC consult SETMA’s Tutorial at HCC RxHCC Risk Tutorial. (To review copy and paste this address into your internet explorer.)
The key to SETMA’s success with HCC and RxHCC was the deployment of a robust ICD-9 Code List with HCC and RxHCC code status denoted in the code list. Recently, SETMA upgraded our code list with the IMO data base (www.e-imo.com). IMO has organized the 15,000 ICD-9 codes with multiple descriptions, creating a database of over 100,000 codes. IMO has also solved the ICD-10 code problem which has 150,000 codes and also has solved the problem of the SNOMED nomenclature. This means that many of the major problems facing healthcare problems are solved with a reasonably priced solution. Because of the number of ICD-9 code descriptions listed by IMO’s product, when ICD-10 is adopted, SETMA providers will already be accustomed to searching through virtually the same number of codes making the transition very simple.
IMO Now Being Used
As will be seen below, SETMA’s use of IMO allows us to do the following:
- Identify all HCC and RxHCC codes, showing those codes which are HCC, RxHCC or both.
- Identifying the coefficient value of each code, i.e., each HCC and each RxHCC is assigned a value which is represented by a number such as .3210.
When the IMO search engine is launched in the Assessment step of the documentation of a patient visit, the description of the diagnosis is typed in. The entire diagnosis is not required but only a key word or series of letters.
The ICD-9 Code is displayed. In front of the description is the denotation as to whether or not the diagnosis is an HCC and/or an RxHCC. Following the ICD-9 Code, the is a another number which is the HCC and/or RxHCC coefficient. When all of the ICD-9 Codes’ HCC coefficients are added together the aggregate HCC Code Coefficient is determined.
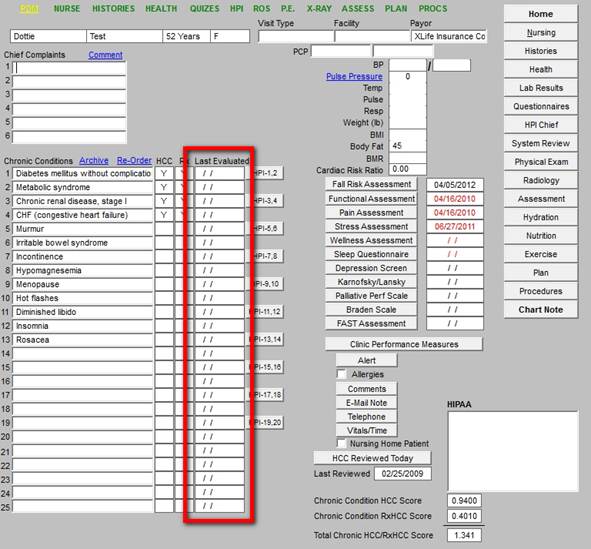
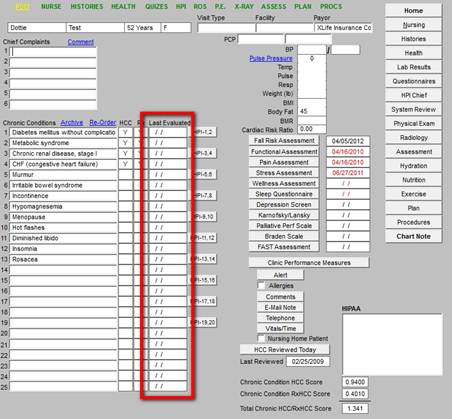
Upgrades to SETMA’s HCC and RxHCC Solution
Two recent improvements have aided SETMA in improving our HCC and RxHCC compliance.
- At the suggestion of Scott Anthony, CFNP, all ICD-9 Codes in a patient’s chronic problem list, which are HCC or RxHCC are highlighted in “red.”
- As the code is assessed each year, making it elibible for payment by CMS, the ICD-9 code is turned to “black.” This means that on January all ICD-9 Codes which are HCC or RxHCC will turn to “red,” as none of them would have been assessed for the current year.
- On December 31st, most and hopefully all of those codes will be “black” indicating that they have been assessed for the year.
- With the deployment of IMO and the identification of the HCC and RxHCC coefficients, three numbers will now appear;
- Summation of HCC and RxHCC coefficients for all valid diagnosis in the patient's chronic problem list
- Summation of the HCC and RxHCC coefficients for all diagnoses in the acute assessment for the current visit
- Summation of the HCC and RxHCC coefficients which have not been assessed for the current calendar year.
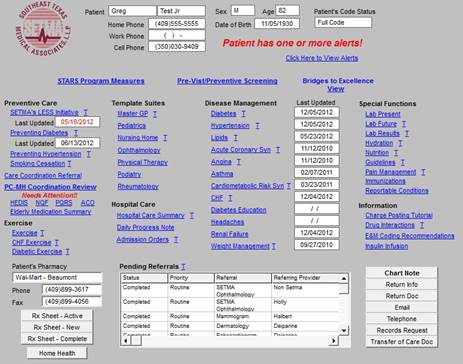
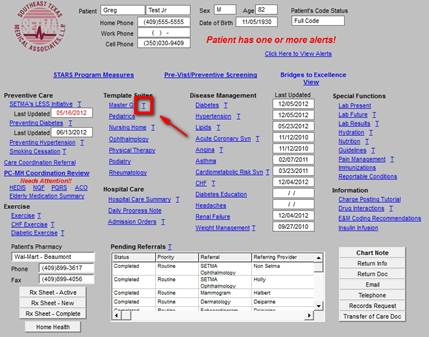
Examples of Real Patients
The following screen shots illustrate the deployment of the red color and the three new numbers which result from the aggregation of HCC and/or RxHCC coefficients. Remember, all of these will not total to the same number. When two HCC codes, or two RxHCC codes are in the same Hierarchical Code Category (HCC), only the diagnosis with the highest coefficient will be counted toward the coefficient aggregation.
This means that the total codes available to be assessed by an evaluation of the ICD-9 codes in the chronic problem list, minus the codes assessed in the current visit, may not match the aggregate of the code coefficients which remain to be assessed. This is true for two reasons:
- Some codes will have been assessed in previous visits.
- All of the codes will not be paid by CMS because there be two or more codes in the same Hierarchical Code Category.
The following illustrate the above.
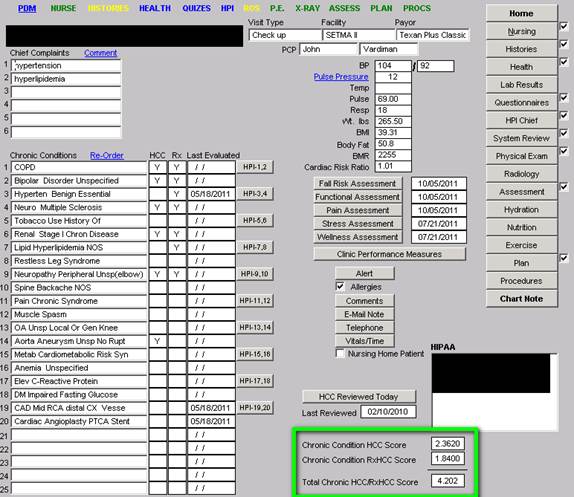
The following is the Master GP template. It illustrates that in the list of chronic conditions the HCC and RxHCC codes are noted. Also, there are functions for documenting that the codes have been assessed for the year.
In the right, lower corner the aggregate of the coefficients are totaled for:
- Chronic Condition HCC
- Chronic Condition RxHCC
- Total for the two
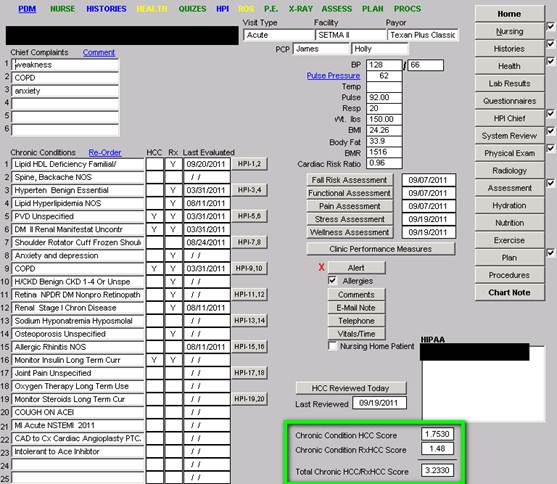
The following is another example of the same template and shows the difference in the two patients.
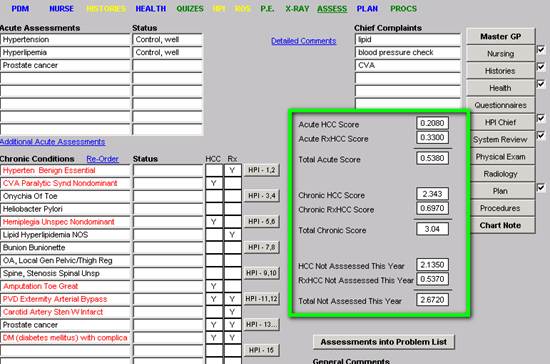
The following template is from a real patient’s Assessment. It shows the ICD-9 codes which are HCC and/or RxHCC Codes and which have not been assessed for the year in “red.”
The box outlined in “green” shows three groups of numbers:
- From the Acute Assessment, the HCC and RxHCC aggregated coefficients are shown and then the two are totaled
- From the Chronic conditions, the HCC and RxHCC aggregated coefficients are shown and the two are totaled.
- From a review of all visits for the calendar year, the HCC and/or RxHCC aggregated coefficients which have not been assessed for the year are denoted.
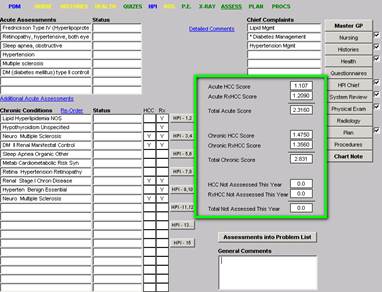
The last template is one which reflects what we hope all patients’ records look like. It is also from the Assessment template:
- All chronic conditions are in “black” which means that all HCC and/or RxHCC have been assessed for the year and are qualified to be submitted for payments.
- And the aggregation of the HCC and RxHCC coefficients shows that none need assessment for this year. However, on January 1st, all will turn red and all will be show as needing assessment.
With the use of IMO, when ICD-10 is deployed in 2014, all of these functions will work equally well.
By James L. Holly
This study examines an implied relationship between Evaluation and Management Codes (E&M) and the Hierarchical Code Categories (HCC) which has two sections the HCC Risk and the RxHCC. The first is based on the diagnosis and is the result of the Center for Medicare and Medicaid’s judgment that caring for a patient with a specific diagnosis is costlier. All ICD-9 diagnostic codes were organized into 189 categories of which 89 were chosen for additional reimbursement. Therefore, if a patient is actively being treated for a specific diagnosis, which is an HCC, a higher payment will be made. The RxHCC refers to the diagnosis but in regard to the pharmaceutical support required to care for a patient with a particular diagnosis. If a patient has an RxHCC code a higher payment will be made.
In general, there are more RxHCC diagnoses than HCC. Almost all HCC diagnoses are also RxHCC, but most RxHCC are not also HCC. The additional payment for HCC is significantly higher than for RxHCC, but because there are more RxHCC diagnoses, generally the greater total value to the practice will come from RxHCC. They should not be ignored. Initially, the HCC system only had value to Medicare Advantage programs but with the advent of Accountable Care Organizations, their value has spread. Ultimately, payments for Patient-Centered Medical Home will be based on a risk-adjusted evaluation of the practice’s population of covered lives. The foundation of that risk adjustment will be the HCC program, making it valuable in Medicare Advantage, Accountable Care Organizations and in Patient-Centered Medical Home.
A detailed explanation of the HCC system is given at the following link: HCC RxHCC Risk Tutorial
Evaluation and Management Codes
The most critical aspect of proper E&M coding is the determination by the provider of the Complexity of Medical Decision Making. There are four levels of this Decision Making. SETMA’s deployment of the E&M Code Calculator, which was created by SETMA without reference to any previously or subsequently published calculator, incorporates all of the elements of E&M coding such as number of systems addressed in the ROS, in the Physical examination, Personal and Family history, disease management tools, etc.
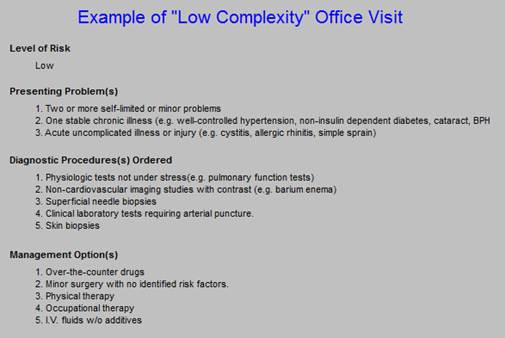
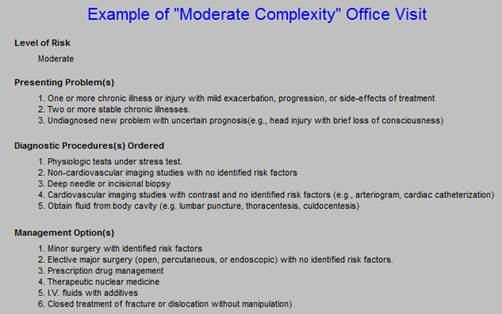
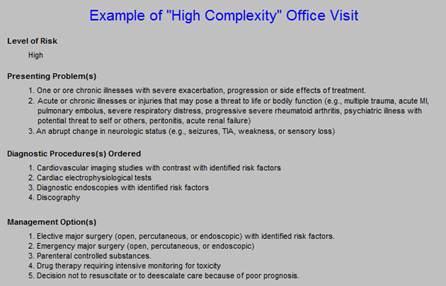
At the following link: E and M Codes Tutorial you will find SETMA’s tutorial for the E&M code determination. This tutorial is also accessible from the Evaluation and Management Template which is deployed from the Plan Template. Details of the proper selection of E&Ms are given there. Because Medical Decision Making is such an important part of E&M coding, and because the HCC and RxHCC system establishes the relative risk of at he complexity of the care a patient requires, we will review the Medical Decision Making aspect of the E&M coding. There are four Medical Decision Making Categories associated with each of four E&M codes: Straight Forward (99212), Low Complexity (99213), Moderate Complexity (99214), and High Complexity (99215).
Medical Decision Making in the Selection of E&M Codes
The following are screen shots of SETMA’s E&M tutorial referenced above. They give the details of Medical Decision Making. There are two principles of E&M Coding which are inviolable:
- If you do not have a chief complaint, you do not have a visit with Medicare. The exceptions to this are the new wellness assessment which is being paid for by Medicare and the provision for the evaluation of two or more chronic conditions qualifying for a 99213 or 99214 visit.
- The driver of the distinction between each of the four E&M codes is Medical Decision Making. The application of this principle is that if the Medical Decision Making is “straight forward,” no matter how extensive a review of systems or physical examination you do, you cannot get to a 99214 or 99215 visits.
As a general concept, 99215 visits in a clinic will be a very low percentage of a clinic’s E&M codes.
Straight Forward (99212)
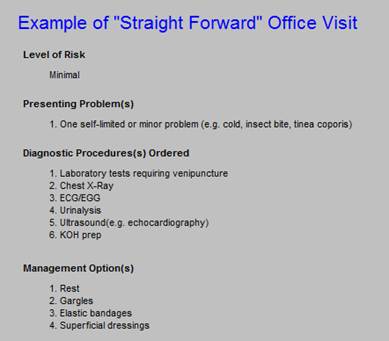
As you review the Medical Decision Making criteria for a 99213 visit, you will see that most visits in a multi-speicality clinic will result in virtually no 99212 visits. The step from 99212 and 99213 is very short. In addition, it is possible to begin seeing the correlation between HCC and E&M. If a patient has an HCC coefficient aggregate score above 0.75, they are certainly going to have at least one “stable chronic illnesses such as well-controlled hypertension, or diabetes,” etc. And, if either of those are not well-controlled, you quickly go in your management, with proper documentation from a 99213 to a 99214.
If any one of SETMA’s disease management tools is used effectively, the 99213 visit is reached and if two of them or used, the 99214 visit is reached. This requires that the tool be used effectively but it is an efficient process.
Low Complexity (99213)
As stated, the step from a 99212 to a 99213 visit is very short. The step from a 99213 to a 99214 is slightly longer but still a relative short step. Again, relating E&M to the appropriate and necessary evaluation and treatment of a patient with multiple HCCs and/or RxHCCs diagnoses, which diagnoses result in a coefficient-aggregate score over 1.00, to the Medical Decision Making criteria for a 99214 visit, shows that patients with this level of risk will most often result in a visit with an E&M code of 99214.
It should be possible, therefore, to compare an individual provider’s E&M code distribution with the mean of his/her HCC coefficient aggregates. The higher the HCC coefficient aggregates the higher one should expect the E&M code distribution to be.
Reviewing the Complexity of Medical Decision Making for the 99214 visit below, it is seen that going from a 99213 to a 99214 involves the evaluation of two or more chronic conditions. Remember, all of this is dependent upon your having evaluated an adequate number of systems review and systems in physical examination. Whether you have or not will be told to you by SETMA’s E&M Code calculator.
Moderate Complexity (99214)
Moving from 99212 to 99213 and from 99213 and 99214 in regard to Complexity of Medical Decision Making is relatively easy. Now, however, the step from a 99214 to a 99215 is a huge leap. It is possible to make this leap, as in the case of malignant hypertension with exacerbation, COPD with exacerbation, CHF with exacerbation, etc, but it will be rare.
High Complexity (99215)
Because SETMA’s electronic patient record displays whether a diagnosis is an HCC, an RxHCC or both, and because our system aggregates the coefficients for all of the diagnoses which are documented in a patient’s care, it is possible for a provider to know on each patient he/she treats:
- The coefficient aggregate for the acute diagnoses documented for each visit.
- The coefficient aggregate for the Chronic Diagnoses documented for each patient.
- The coefficient aggregate which has not been evaluated on a patient for the current year.
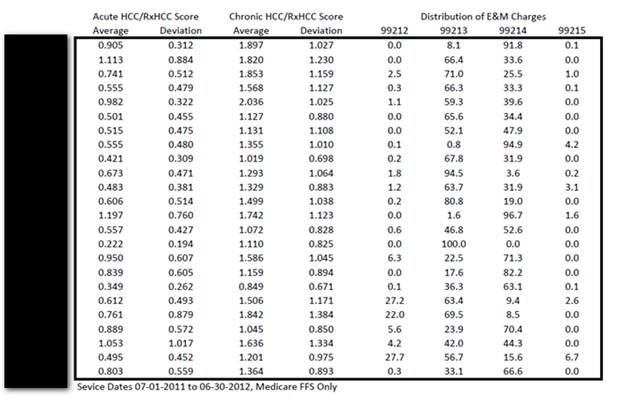
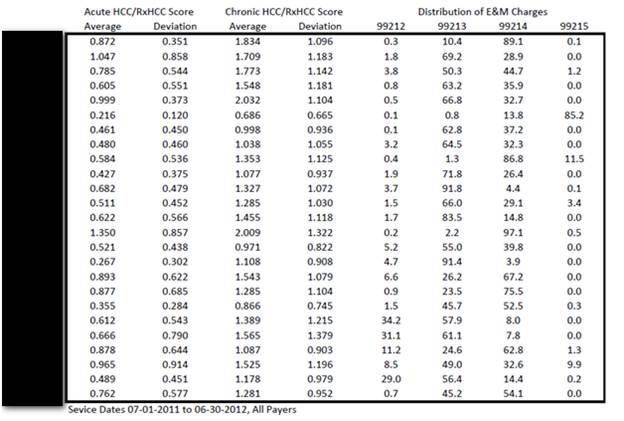
The following tables contrast:
- Medicare Fee-for-Service HCC/RxHCC coefficient aggregates with Medicare Advantage HCC/RxHCC aggregates
- Medicare Fee-for-Service contrasted with Medicare Fee-for-Service E&M Code distribution by provider name.
- All Payers HCC/RxHCC aggregates contrasted with E&M Codes
The following is a contrast between Medicare FFS and Medicare Advantage’s Mean HCC/RxHCC coefficient aggregates and their standard deviations. It can be seen that Medicare FFS coefficient aggregates are significantly lo0wer than the Medicare Advantage Coefficients.
The question is, “Is this because the populations are significantly different?,” or is it because we have not been as effective in capturing HCC/RxHCC for Medicare Fee-for-Service patients?. Now that SETMA is participating in an ACO, where patients are also risk stratified as to cost and revenue attributed to that group of patients, we need to make sure that we are being as effective in FFS as in MA.
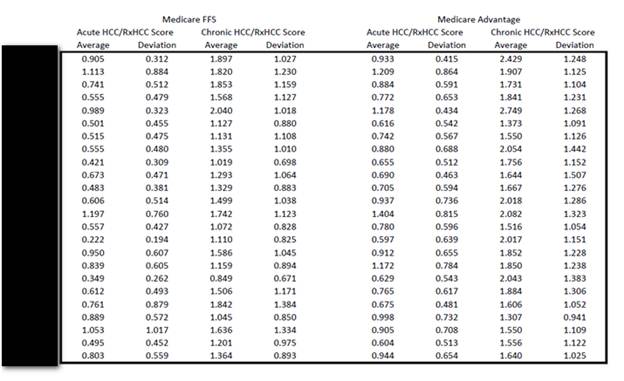
The next display is of Medicare Fee-for-Service coefficient aggregates both for acute diagnoses which have been evaluated at a visit and the chronic diagnoses which represent the patient’s problem list for which he/she is being treated. Later, this is contrasted with the E&M code distribution for each provider.
By implication, we think there is a correlation between the acute diagnoses’ HCC/RxHCC coefficient aggregate and the E&M code. The higher the HCC/RxHCC coefficient aggregate for the acute visit, the higher it is reasonable to expect the E&M coding to be, IF the documentation is present in the record related to two or more chronic conditions.
The following displays the HCC/RxHCC coefficient aggregates for all payers contrast with the distribution of E&M Codes. This is a good control on Medicare Fee-for-Service and Medicare Advantage.
Summary:
The correlation between HCC/RxHCC coefficient aggregates is not proved and it is not supported by CMS policy. It is a new idea, which I think has benefit in our understanding of risk and reward.
Because HCC/RxHCC now has validity beyond Medicare Advantage, contrasting ACO, MA, and Medical Home populations - which in the future will probably become the same population - helps us make sure that our management of these patients is the same.
|