|
SETMA’s Disease Management tools For Diabetes, Hypertension and Lipids Used for patient activation and engagement via written Plans of Care and Treatment Plans
Providing our patients a written, personalized Treatment Plan and Plan of Care is a critical aspect in patient activation and engagement. These documents serve as a “baton” which empowers the patient to care for themselves. The following poster which appears in all SETMA’s examination rooms and a framed copy of which appears in all public places at SETMA symbolizes the “baton.”

Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient, If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home are symbolized by the “baton.” Its display will continually remind the provider and will inform the patient, that to be successful, the patient’s care must be coordinated, which must result in coordinated care. As we expand the scope of SETMA’s Department of Care Coordination, we know that coordination begins at the points of transitions of care, and that the work of the healthcare team -- patient and provider -- is that together they evaluate, define and execute that care.
Since 2003, SETMA has been producing Follow-up Documents for each of the chronic diseases tools which we have deployed in our EMR. We have now made modifications in these tools so that the Follow-up Document have become written Treatment Plans and Plans of Care. (This tutorial addresses only the Treatment Plan and Plan of Care. For a full review of the disease management tools see the tutorial on each.)
Assessing Cardiovascular Risk Score of Each Patient
SETMA’s Innovative Use of the Framingham Risk
A plan of care should be founded on the patient’s relative risk of disease. The best tool we have for assessing that risk, particularly cardiovascular risk is the Framingham Risk Scores. SETMA’s deployment of these scores can be found at: Framingham Cardiovascular and Stroke Risk Assessment Tutorial. This tutorial explains the changes and use of SETMA’s deployment of the 12 risk calculators published by the Framingham Heart Study. These tools are not absolute and must be used simply as an indication of potential cardiovascular and cerebrovascular risk and not as an absolute indicator of future disease.
If You Make a Change it Will Make a Difference
The most innovative use of the Framingham Risk Calculators were suggested by SETMA’s associates at the Diabetes Center of Excellence in Boston (SETMA is the only multi-specialty Affiliate of the Joslin Diabetes Center). Drs. Richard Jackson and Ken Snow, while visiting SETMA, recommended the adding of a “What If Scenario” to our display of all twelve calculators.
The concept is that we are asking patients to make changes which will not show up as benefits for decades. Of course, ignoring those changes will result in irrevocable deterioration in the patient’s health over those decades. But how do you “prove” to a patient that “if you make a change, it will make a difference?” One way is with the Framingham Risk Calculators being presented to the patient with the inclusion of the changes which would result if the patient improved the elements of the risk calculator.
Even though these risk calculators are not perfect, they are still the best we have. And, it is imperative that patients know and that their provider knows what their risk is, because it is with the knowledge of the patient’s cardiovascular risk that a plan of care and a treatment plan can be designed to help preserve the patient’s health.
Remember, “Risk” is an attempt to determine what the future might be like which means it is imprecise. Some people with a high risk will not experience poor health and some who have low risk will. Overall, however, those with high risk will have more heart attacks and strokes than those with low risk.
Dynamic Complexity
The problem with biological systems is that change, even change which results in deterioration of your health, does not occur quickly and it often occurs without any signs or symptoms until the illness, or disease process has already caused significant damage. There is no explanation of this principle more apt to our use of “risk calculators” than Peter Senge’s explanation of “dynamic complexity” in The Fifth Discipline.
Senge defines “dynamic complexity” as a situation “where cause and effect are subtle, and where the effects over time of interventions are not obvious.” This perfectly describes the development of many disease states and the benefit of their treatment. We know that obesity causes, or contributes to most diseases including diabetes, hypertension, heart disease, cancer, etc. In these conditions, “obesity” is the cause; “cancer” is the effect, but the change is slow and is not apparent. Also, the results of treatment are very slow. Consequently, it is hard to sustain the changes necessary to eliminate the “cause,” which is obesity, in order to avoid the “effect” which is cancer.
Shifting the Burden
There are structural problems which aggravate the obvious solutions to a business or a health problem; Senge addresses one of these and calls it “the shifting the burden.” He defines “shifting the burden,” as “an underlying problem generates symptoms that demand attention. But the underlying problem is difficult for people to address, either because it is obscure or costly to confront. So people ‘shift the burden’ of their problem to other solutions - well intentioned, easy fixes which seem extremely efficient. Unfortunately, the easier ‘solutions’ only ameliorate the symptoms; they leave the underlying problem unaltered. The underlying problem grows worse, unnoticed because the symptoms apparently clear up, and the system loses whatever ability it had to solve the underlying problem.”
This happens in healthcare when a person looks to healthcare providers or medications to solve a problem which can only be solved by their own habits, choices, decisions and resolution. A pill, or a procedure, or a prescription is sought in order to overcome the “obesity.” It will work for a short while but not long term. When it fails, more aggressive interventions are tried without addressing the fundamental problem.
The Quick Fix Deception
Senge’s business prescription is a good one for healthcare, also. He says, “Beware the symptomatic solution€š that address only the symptoms€š not fundamental causes, tend to have short-term benefits at best. In the long term, the problem resurfaces and there is increased pressure for symptomatic response. Meanwhile, the capability for fundamental solutions can atrophy.” Senge adds, “The ‘easy solution€š the ‘quick fix’€š solves the problem temporarily€š (but) a shifting of burden structure lurks behind many ‘solutions (and) explains a wide range of behaviors where well-intentioned ‘solutions’ actually makes matters worse over the long term.”
Senge and Medicine
The longer a person delays addressing the “real” cause of their problem, the fewer options and the fewer resources they have for dealing with the “real” cause of the problem. For instance, the longer a person fails to exercise, often resulting in gaining weight and diminishing heart function, the more difficult effective solutions will be once a person determines to improve their health. If a person continues to “shift the burden” of their own irresponsibility to another, expecting an artificial solution to relieve the burden created by the rejection of the real solution, they will never achieve their goal. In this case, the harder the patient pushes for solutions from a healthcare system which cannot solve their problem, for which a natural and obvious solution exists, the less benefit the patient will achieve. It is possible to ignore the real solutions - i.e., activity such as walking - until the knees and other joints have deteriorated and it is not possible to become active. In that case, more and more pressure is placed on the artificial system with less and less satisfaction with the results.
Risk Calculators: Dynamic Complexity and Shifting the Burden
These are the reasons for our using “risk calculators.” Because in a biological system proving the benefit of fundamental solutions by waiting for the negative consequences of poor health choices is not acceptable, we use “risk calculators” to project what those poor choices will lead to. Hopefully, those risk calculators will help patients make a decision to make a change.
At SETMA’s website under Your Life Your Health, twenty-two articles can be found under View Articles by Subject and by accessing Cardiovascular Disease Risk Factors.
What If?
Because it takes SETMA only one second (really) to calculate all twelve risk calculators, we thought we were doing great. However, when we showed this function to our new colleagues from Joslin Diabetes Center, Dr. Richard Jackson commented that these scores overstate the risk and Dr. Kenneth Snow asked if we could show the patient how their risk would be affected if they make a change in their habits? Sadly, we had to admit that we could not. That was on Tuesday November 30, 2010.
We realized that while the patient has to know their risk, to understand “dynamic complexity” and its dangers for their ignoring their health until it is too late, and to avoid “shifting the burden” of responsibility from themselves to another, their healthcare providers have a responsibility to show them that if “they make a change that it will make a difference.”
Completing the Treatment Plan and Plan of Care
In order for the Treatment Plan and the Plan of Care to be precise and specific for each patient, it is important that you first complete the Framingham Cardiovascular and Cerebrovascular Risk Scores and the Global Cardiovascular Risk Score before using the below functions. (Note: You only have to complete the risk scores once on each visit, after which the score is displayed on all of the disease management tools and will work interactively with the Treatment Plan and Plan of Care.)
In completing the Risk Scores, you will also be fulfilling another of the NCQA Medical Home Requirements which is the assessment of the risk of future disease for patients.
Using the Framingham Cardiovascular Risk Score
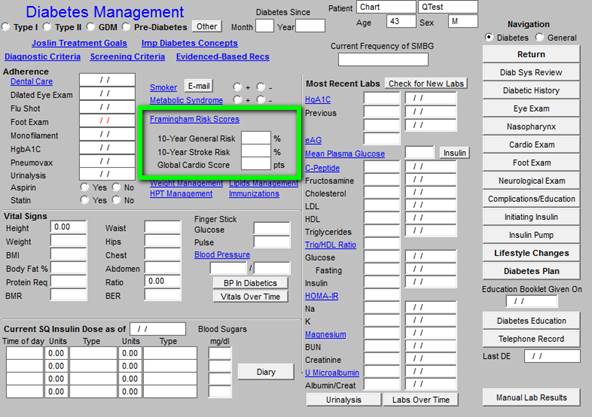
You can find the Framingham Risk Scores calculation tools on each of the Diabetes, Hypertension and Lipid Disease Management tools. The following illustrates its location on the Diabetes Template.
This launches the following template. When this template is opened, all of the Framingham risk scores will be automatically calculated.
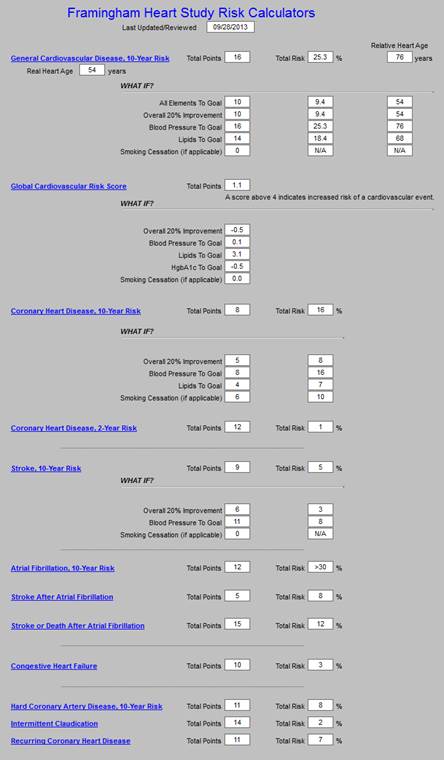
The Risk Score will now be displayed on this template, on each of the disease management tools and it will also be used in preparing your Treatment Plan and your Plan of Care for each patient.
Using the Global Cardiovascular Risk Score
Several years ago, it was recognized that the Framingham Score weighted the patient’s age so heavily that some young people with high cardiovascular risk were missed and some older patients with lower cardiovascular risk were misjudged as being at high risk.
An analysis was done of the Framingham Data and the Global Cardiovascular Risk Score was created. This score uses the Framingham Data but eliminates the age and gender bias, adding Hemoglobin A1C to the assessment. If the score is above 4, the patient is considered to have high Cardiovascular Risk.
To view the detailed elements of the Global Cardiovascular Risk Score, click the following button on the main Framingham template.
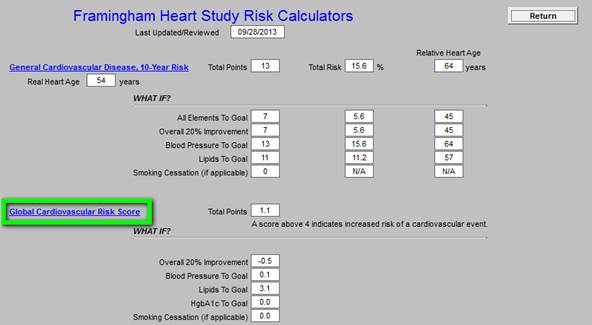
This launches the following pop-up. Activate the button entitled Import. This will aggregate the data required to calculate the score.
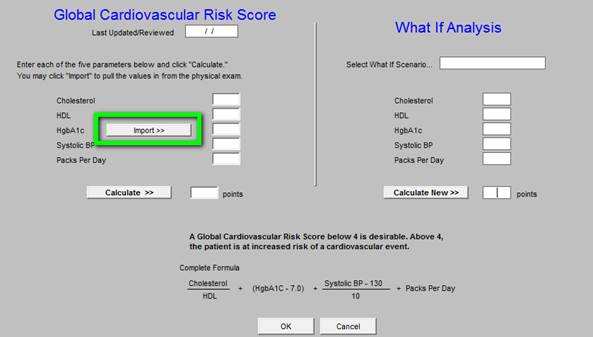
To complete this process, activate the button entitled Calculate
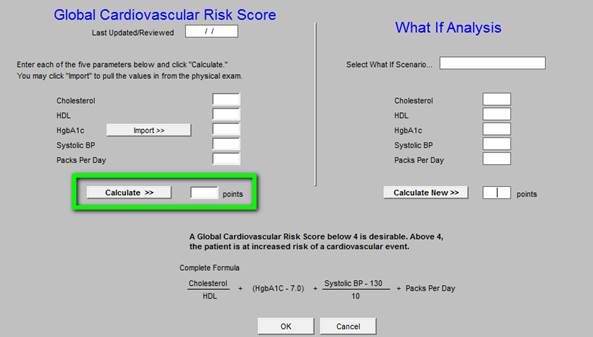
The score will be displayed on this screen, on all of the disease management tools and will be used in preparing your Plan of Care and Treatment Plan on each patient. A value above 4 indicates that the patient is at increased risk.
The principle difference which you will find is that at times young people who have a low Framingham risk score, will have a high Global Cardiovascular risk score and older people who have a high Framingham Score will have a lower Global cardiovascular risk score. This is because of the elimination of the age as a factor.
SETMA’s Disease Management tools For Diabetes, Hypertension and Lipids Used for patient activation and engagement via written Plans of Care and Treatment Plans
Definitions:
- Treatment Plan: “A written plan detailing the medical regimen as ordered by the physician, including periodic monitoring for adverse reactions and other follow-up care.”
- Plan of Care: “a written plan for services that will be provided to the patient to meet their identified needs.”
Diabetes Treatment Plan and Plan of Care
You will find the Diabetes Disease management Tool by going to AAA Home
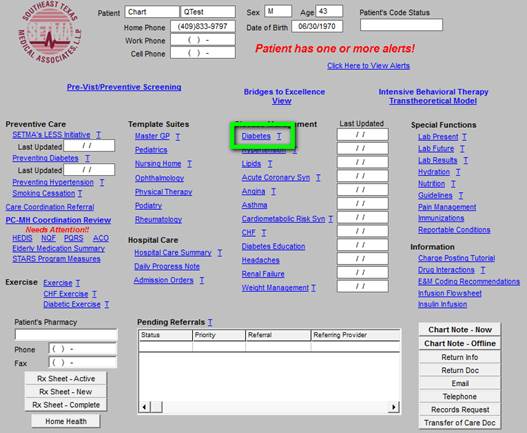
Click on the button entitled Diabetes and the Disease Management tool is launched.
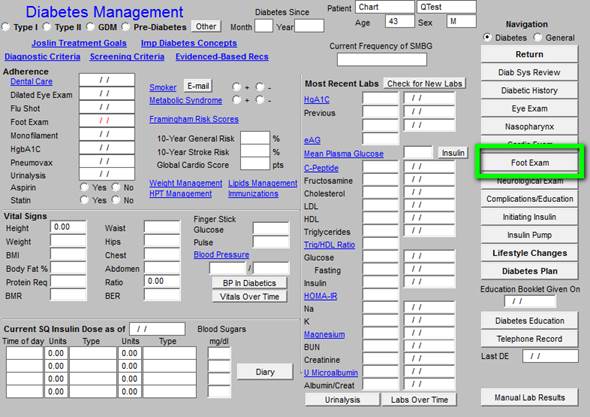
All of the evaluation and documentation which you have done on GP Master will populate this tool as well. While this tool can be used as a complete guide to the treatment of diabetes, it may also be used for our current purpose.
To use the tool for Treatment Plan and Plan of Care, make certain that the “10 Gm Monofilament foot examination” has been done. You will find that examination by clicking on “Foot Exam” above
From the Diabetes Management template, click on the navigation button entitled Lifestyle Changes.
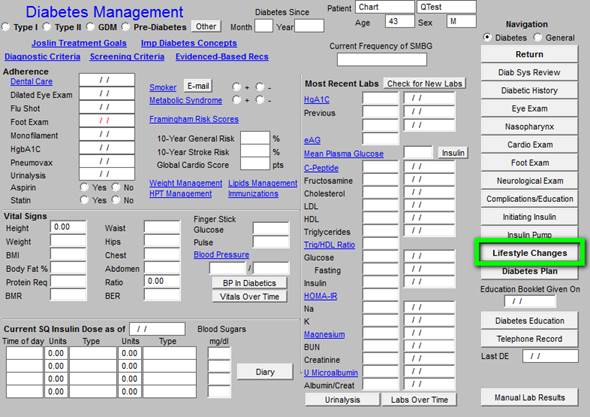
You will then see the following template
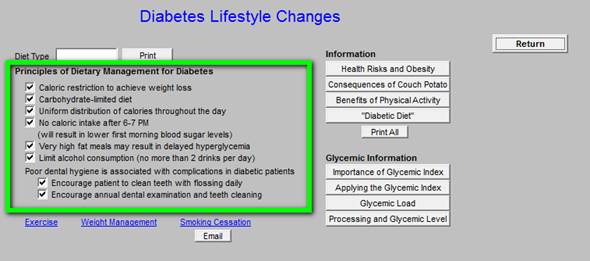
This template automatically selects the Principles of Dietary Management for Diabetes. Click on Return.
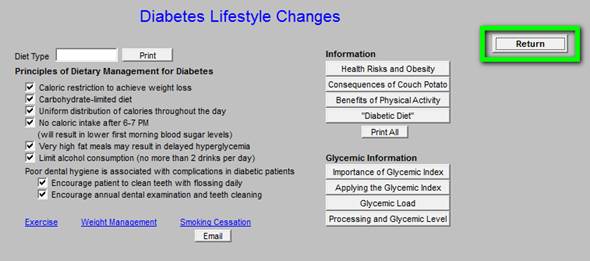
This returns you to the Diabetes Management template.
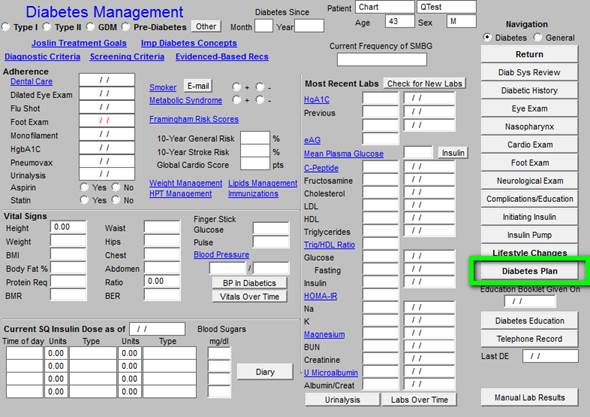
Now, click on Diabetes Plan. This launches the Diabetes Plan template.
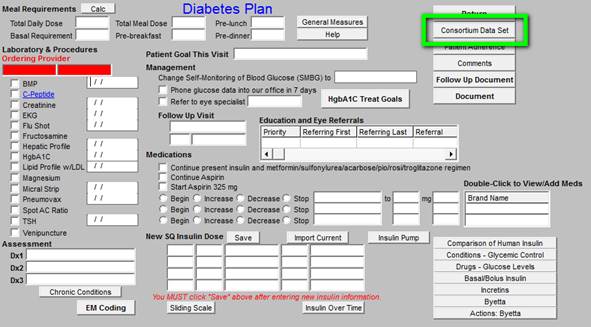
You may review the Consortium Data Set from this template or from the Medical Home Coordination Review template. Once you review the Consortium Data Set to make sure that your comprehensive diabetes measures have been met, click on Follow-up Document.
This creates the Follow-up document which has all of the elements of a written Treatment Plan and a written Plan of Care.
- Print this document and give it to the patient. (You should review one of these documents so that you can tell your patient what this document contains and what you want them to do with it.)
- Make sure they receive the Follow-up Document before they leave the clinic.
- If you do significant modifications to the Treatment Plan and/or Plan of Care after reviewing the patent’s lab work, re-create the Follow-up Document and have it mailed to the patient.
You are through. You have produced a document which is educational to the patient and which meets a standard of care of which you can be proud.
Lipid Treatment Plan and Plan of Care
You will find the Lipid Diabetes Disease management Tool by going to AAA Home
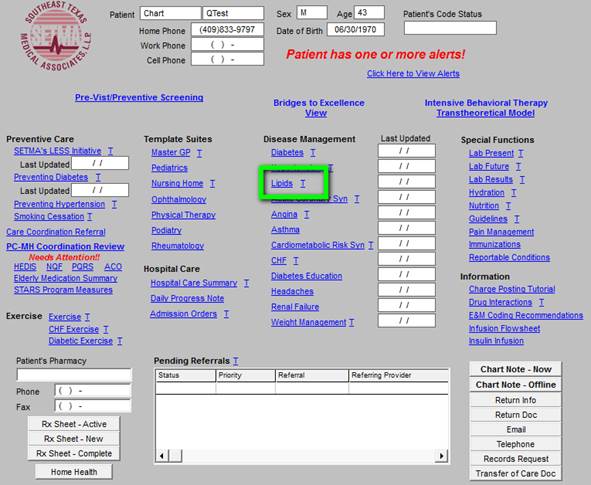
Click on the button entitled Lipids and the Lipids Disease Management tool is launched.
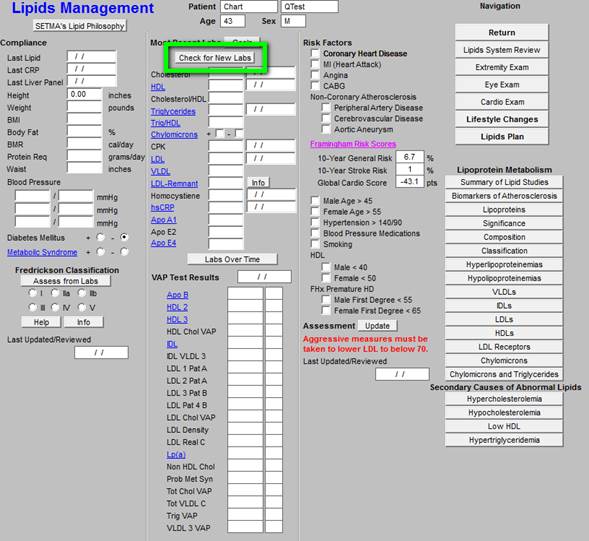
All of the evaluation and documentation which you have done on GP Master will populate this tool. While this tool can be used as a complete guide to the treatment of lipids, it may also be used for our current purpose. In order to make use the Fredrickson Classification function, click on the Check for New Labs button.
To use the tool for Treatment Plan and Plan of Care, click on Assess from Labs button at the lower left hand corner of the template.
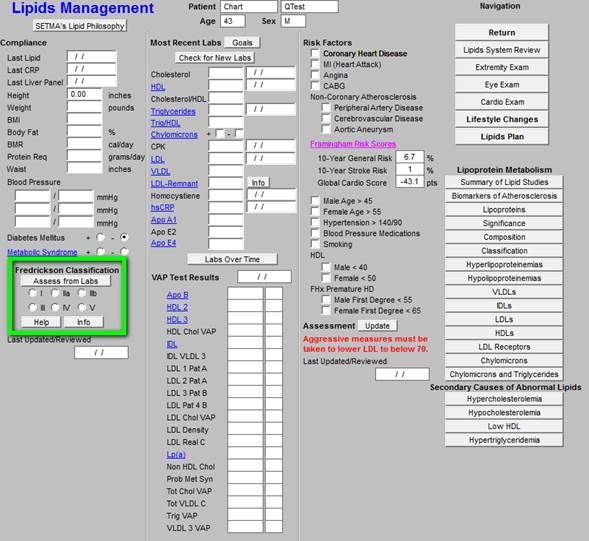
If the patient’s lipid pattern matches one of the phenotypes in the Fredrickson Classification, it will be automatically denoted and an education document on that type will be added to the patient’s Lipid Follow-up Document. This will be done automatically.
If you want to review this patient’s specific lipid-phenotype document, click on the button entitled Info at the bottom left of the template. If no type is automatically selected but you wish to assign one, just check the appropriate box.
If you wish to review the six phenotypes in the Frederickson Classification click on the button entitled Help also at the bottom left of the template.
Next click on the navigation button entitled Lifestyle Changes.
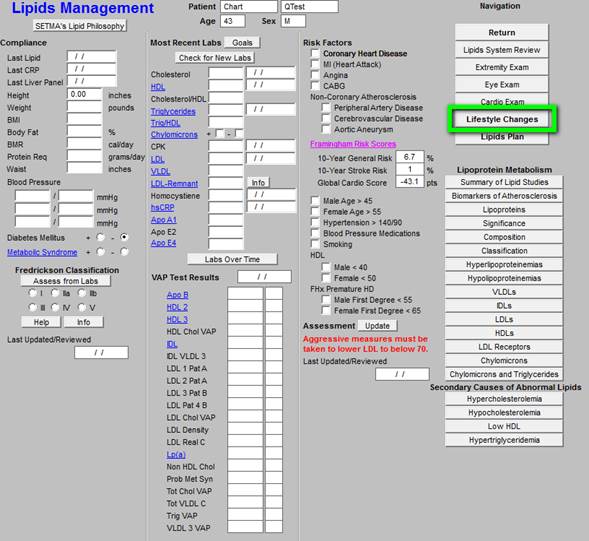
On the Lifestyle template, check the box by any of the diets which apply to your patient. You can click as many as apply. All of the diets which are checked will appear on your Lipid Follow-up Note.
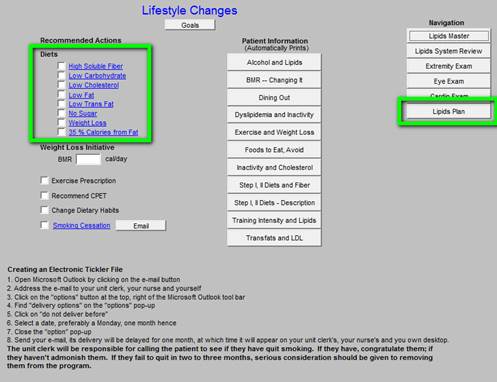
Click on the Lipid Plan navigation button. (see above Lipid Plan button in green)
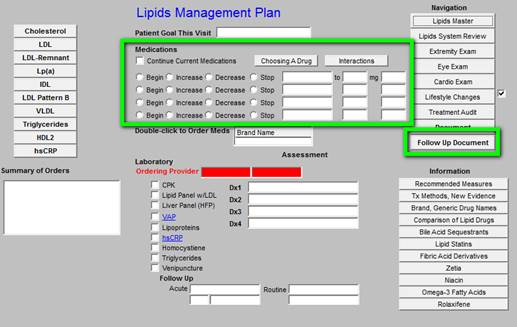
Note any changes in medications or note to “continue current medications”. Then click on the Follow-up Document. Print this document and give it to your patient. You are done.
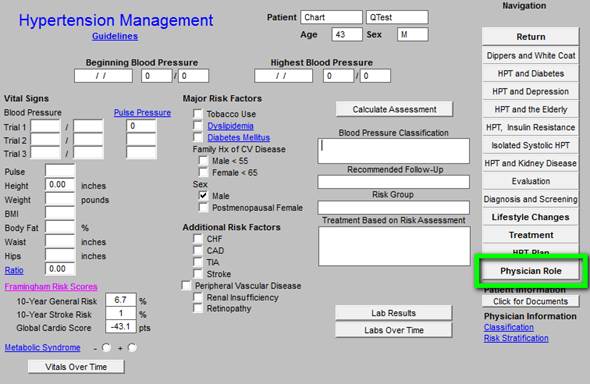
Hypertension Treatment Plan and Plan of Care
You will find the Hypertension Disease management Tool by going to AAA Home
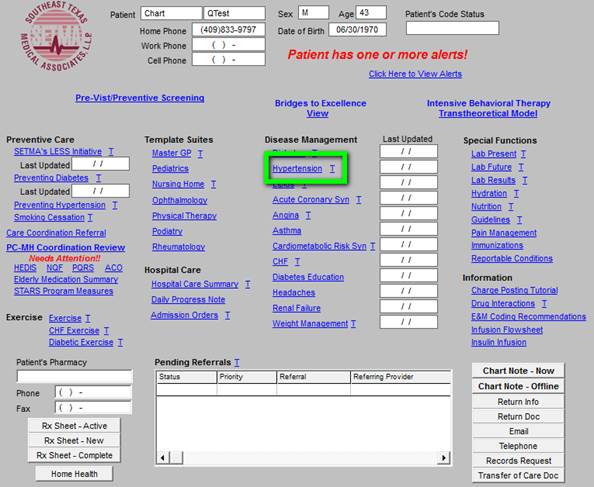
Click on the button entitled Hypertension and the Hypertension Disease Management tool is launched.
All of the evaluation and documentation which you have done on GP Master will populate this tool as well. While this tool can be used as a complete guide to the treatment of hypertension, it may also be used for our current purpose.
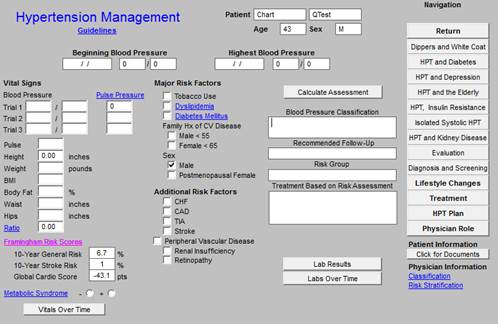
In order for this to fulfill all of the NCQA requirements for hypertension, you must click the button entitled Calculate Assessment
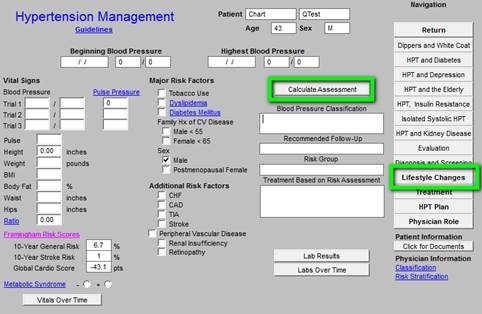
This displays the:
- Blood Pressure Classification,
- Risk Group,
- Recommendation and Treatment Plan based on the Risk Group.
All of these are elements of quality measures for hypertension. Now, in order to use the tool for Treatment Plan and Plan of Care, click on the navigation button entitled Lifestyle Changes.
This will display a template which addresses the major lifestyle changes which will significantly influence blood pressure, along with the potential reduction in systolic pressure which can be achieved by each. All of these will be automatically selected and they will also appear on your Treatment Plan and Plan of Care for hypertension.
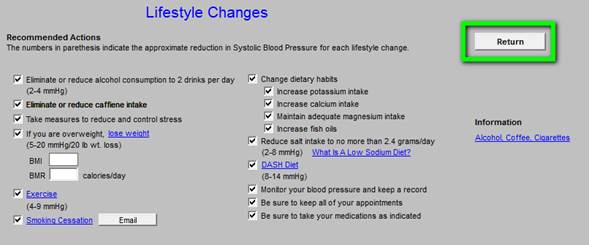
You ought to review the information on this template. There is also the ability for documenting Exercise and Smoking Cessation on this template. Click on Return, which will display the Hypertension Master template.
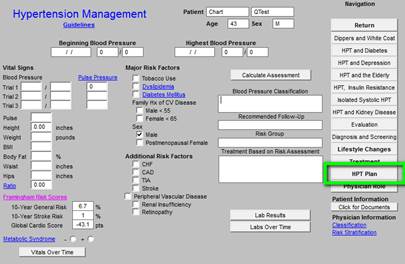
Now click on the button entitled HPT Plan. You need to do three things on this template:
- Complete the section on whether to “continue current medication” or “add or change a medication”
- Then click on the button entitled Follow-up Note.
- Then click on
- Return.
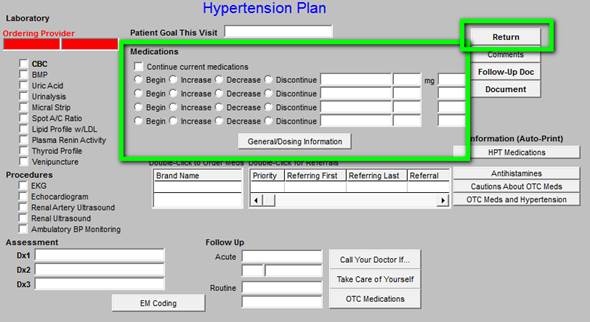
When you click on the Follow-up note, this creates note which you should give to the patient. It will also have material on the DASH diet and a low sodium diet.
This note will fulfill all of the requirements for a written Template Plan and for a written Plan of Care. When you click Return, it will take you back to the Hypertension Master template.
You may assess whether you have completed all of the appropriate measures for hypertension by clicking on the navigation button at the right of the template entitled Physician Role.
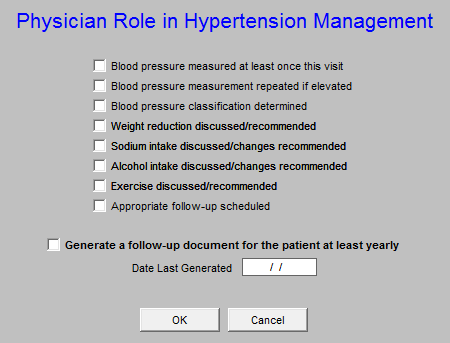
This same material can be reviewed from the Medical Home Coordination Review Template. Once you have reviewed this template, click OK. You are done.
To use these three disease management tools to create robust, personalized, specific and complete Treatment Plans and Plans of Care not only meets NCQA requirements, but improves the quality of care which you will be giving to the members of your Medical Home. Even if your patient has diabetes, hypertension and dyslipidemia, as many of our patients do, it takes only a couple of minutes to complete these tasks and to produce the documents which fulfill one of the most complex NCQA requirements. Once you give these documents to your patient, instruct them to read them and at their next visit review anything they do not understand, you have taken another step toward excellence.
|