|
STARs Tutorial
Medicare Advantage Plan Star Ratings and Bonus Payments in 2012
A Tutorial for Utilizing SETMA’s Deployment of the STARS MA Program
Increasingly, health plans and particularly Federal programs are requiring evidence of quality performance with reimbursement tied to that evidence. In 2007, the Institute for Healthcare Improvement (IHI) enunciated The Triple Aim for the future of healthcare which is: improved health, improved care, lower cost. The IHI identified “integrators” of health as the organizations which would move healthcare in the direction and to the destination, we need to go.
Three of those “integrators” are:
- Medicare Advantage
- Medical Home
- Accountable Care Organizations
Each of those “integrators” have a defined set of quality measures which are required in order to participate and in order to receive the maximum reimbursement.
- Medicare Advantage - Stars Program - 53 Quality Metrics
- Medical Home - National Quality Forum endorsed measures - 10 required by NCQA
- Accountable Care Organizations - 33 define quality metrics
There is significant overlap to these requirements. Because SETMA reports on numerous quality measures and groups of measures - NCQA, PCPI, AQA, HEDIS, NQF, Guidelines Advantage, Core Measures (Hospital), Bridges to Excellence, PQRS, Joslin, SETMA Developed Measurement SETS and STARS, ACO measurements - we are preparing a spreadsheet which will show how many measurement sets each metric appears in. The ideal will be for a single measurement set be developed. The only limitation to that ideal is there are legitimate cases where a metric is relevant to one entity and not to another.
SETMA’s deployment of the STARs measures is to insure that the Golden Triangle Physicians Alliance (GTPA), a qualified Independent Physician Association (IPA), achieves a 5-Star rating. Because the provider-performance-dependent metrics are HEDIS measures and because SETMA has been tracking and auditing HEDIS performance for five years, the Stars program is nothing new to us. In fact, SETMA’s HEDIS results, by provider name, are reported on our website under Public Reporting.
We do believe that the specific attention to the Stars subset of HEDIS measures will enable us to know more precisely where our performance falls short and to address improvement strategies. Always remember, any information required to determine if the patient is eligible for a metric and any determination if they are adherent is automatically aggregated.
(The following excerpt is from a “Data Brief” is taken from the Medicare Advantage Plan Star Ratings and Bonus Payments in 2012, supported by the Henry Kaiser Family Foundation.)
For several years, the Centers for Medicare and Medicaid Services (CMS) has posted quality ratings of Medicare Advantage plans to provide Medicare beneficiaries with additional information about plans offered in their area. All Medicare Advantage plans are rated on a 1 to 5 star scale, with 1 star representing poor performance, 3 stars representing average performance, and 5 stars representing excellent performance. The quality scores for Medicare Advantage plans in 2011 are based on 53 performance measures that are derived from plan and beneficiary information collected in three surveys - HEDIS®, CAHPS®, and HOS - and administrative data. For example, the performance measures include whether the plans’ enrollees received the appropriate screening tests, the number of complaints CMS received about the plan, and how enrollees rated the communication skills of the plans’ physicians. CMS assigns quality ratings at the contract level, rather than for each individual plan. This means that every Medicare Advantage plan covered under the same contract receives the same quality rating (and most contracts cover multiple plans).
In 2012, Medicare Advantage plans will begin to receive bonus payments based on quality ratings. These payments were initially established in the 2010 health reform law that provides for bonus payments to plans that receive 4 or more stars and to unrated plans beginning in 2012. In addition to the bonus payments established by the health reform law, CMS will also be launching a 3-year demonstration to begin in 2012 that increases the size of bonuses for these plans, and also provides bonuses to plans rated as average (receiving 3 or 3.5 stars), using the same 1 to 5 star scale. The demonstration, according to CMS, aims to encourage “plans to improve performance at various star rating levels” and to test “whether providing scaled bonuses will lead to more rapid and larger year-to-year quality improvements in Medicare Advantage program quality scores,” compared to the bonus structure under the health reform law. Proponents say the demonstration will encourage plans at various star ratings to improve or maintain their quality ratings, while others question the appropriateness of providing bonuses to plans with average ratings, and the costs associated with the demonstration.
Star Ratings. CMS rates Medicare Advantage plans on a scale of one to five stars, with five stars representing the highest quality. The CMS defines the star ratings in the following manner:
| 5 Stars |
Excellent Performance |
| 4 Stars |
Above Average Performance |
| 3 Stars |
Average Performance |
| 2 Stars |
Below Average Performance |
| 1 Star |
Poor Performance |
All Health Maintenance Organizations (HMOs), Point of Service (POS) plans, local Preferred Provider Organizations (PPOs), regional PPOs, and Private Fee-for-Service (PFFS) plans are eligible for bonus payments, and are rated by CMS unless they are too new or have too few enrollees. The star ratings are derived from four sources of data: 1) CMS administrative data on plan quality and member satisfaction; 2) the Consumer Assessment of Healthcare Providers and Systems (CAHPS®); 3) the Healthcare Effectiveness Data and Information Set (HEDIS®); and 4) the Health Outcomes Survey (HOS). CMS groups the individual quality measures for the 2011 stars into the following nine domains:
| Domain |
Number of Measures |
Staying healthy: screenings, tests, and vaccines |
13 |
Managing chronic (long term) conditions |
10 |
Drug plan customer service |
7 |
Ratings of health plan responsiveness and care |
6 |
Health plan member complaints, appeals |
4 |
Drug pricing and patient safety |
4 |
Health plan telephone customer service |
3 |
Drug plan member complaints, members who
choose to leave, and Medicare audit findings |
3 |
Member experience with drug plan |
3 |
SETMA’s Tutorial for Using the EMR’s STARs Deployment
As with all of SETMA’s tracking of quality metrics, one patient at a time, their fulfillment is aggregated incidental to care. The object of patient care is not the fulfillment of quality metrics; it is “better care, better health and lower cost.” But, like a Global Positioning System (GPS), quality metrics can tell you where you are, where you want to go and how to get there. But, also like a GPS, the object of the trip is not simply to know the points along the way. The object is to safely, securely and successfully to reach the goal.
SETMA’s STARS deployment can be found on the AAA Home template by clicking on the button entitled “STARS Program Measures,” which is outlined in green below.
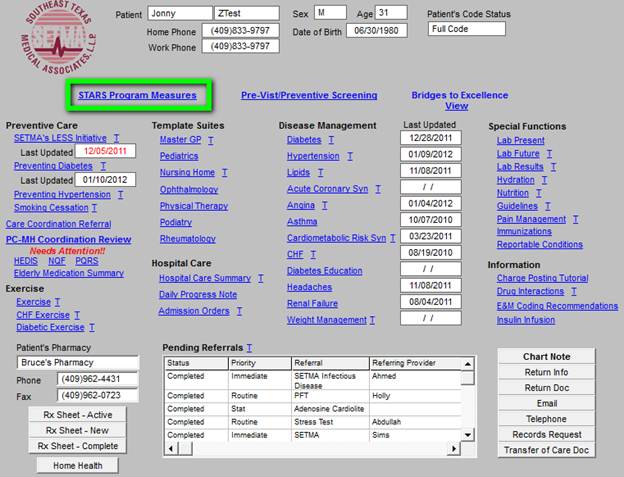
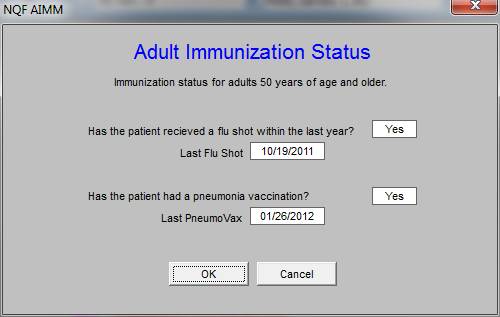
That button launches the Medical Advantage 2012 STARS Program template as seen below. The legend reminds you that all measures which apply to the current patient and that have been met are in black; all which apply and have not been met are in red and all that do not apply are in grey.
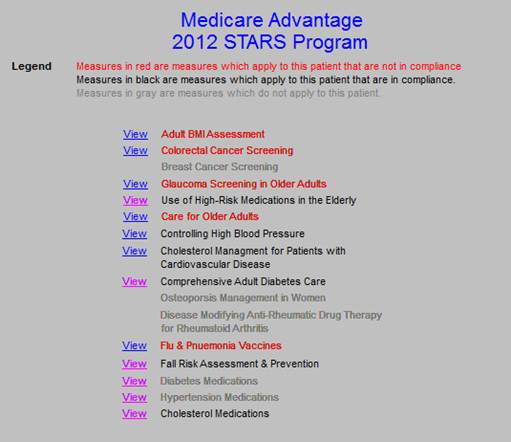
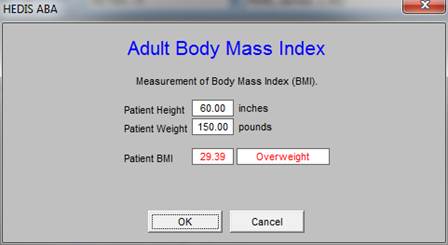
Each of the STARs measures’ content can be reviewed by clicking on the “view button” next to the measure. You will then be able to review who to fulfill the measure.
Remember, if the measure is in black or grey, you do not have to review it; it has either been done or does not apply. If it is in red, you need to review it and to complete its performance on this particular patient.
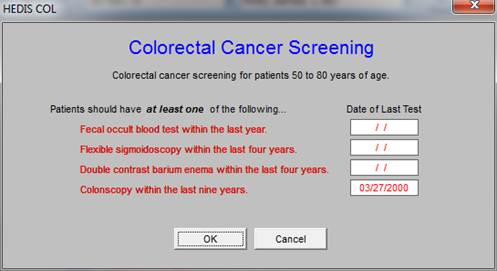
Where there are multiple ways of satisfying a measure such as in colorectal cancer screening, all options will be display. The date of the metric being last met will be shown under “Date of Last Test.” Remember, compliance is by calendar year, not “in last twelve months.” This means that if a patient is seen on December 12, 2012 and they had a fecal occult blood on December 18, 2011, they have had a test in the past twelve months but not the last calendar year and are thus not in compliance for the year 2012.
Interestingly, while Medicare only pays for a mammogram every 2 years or less, the standard for Medicare Advantage is that they have a mammogram every year.

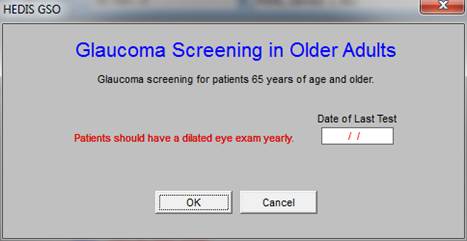
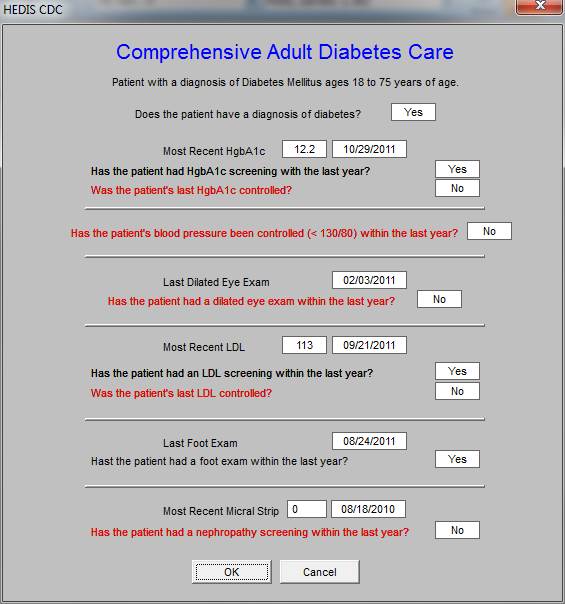
Different measures, measure different functions. Every patient with diabetes should have a dialted eye examination annually. This metric specifically addresses patients by age. All patients over the age of 65 should have an annually dilated eye examination. The value of electronics is that you do not have to remember all of the nuances; the system remembers them for you.
High Risk Medications
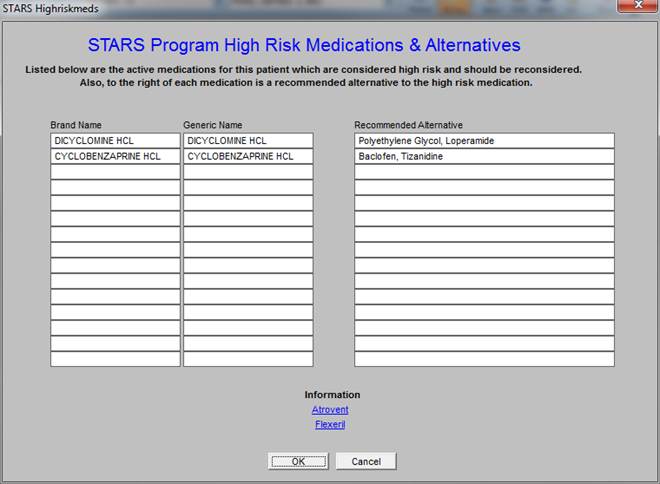
Most of the high risk medications are taken from the HEDIS metrics in which there are five categories of “p0\potentially” high risk medications, which include several hundred medications. SETMA has tracked these for the past five years. In the HEDIS measures, there are two categories: the first are patients who are on one potentially high risk medication and the second are patients on two or more. In the STARS program, the measure is only on those who are on at least one “high risk medication,” as the HEDIS list has been modified from “potentially” high risk to high risk. The threshold for meeting this element of the STARS program is that there must be fewer than 9.3% of your patients on any one these medications.
NOTE: The STARs metric not only alerts you to the presence of a high risk medication in the patient’s medication list, but recommends a substitute medication.
Continuity Medical Education
As part of SETMA’s CME program, our Chief Medical Officer, Dr. Syed Anwar, is writing short descriptions of each medication. These can be deployed by clicking on the name of the medication which appears at the bottom of the template.
Atrovent
The study behind the news analyzed data collected between 1991 and 1993 as part of a large study into the decline of mental functioning in people aged over 65. The new research re-analyzed the participants’ records to look at how their mental decline was linked to their use of drugs with “anticholinergic” side effects (such as dry mouth, reduced mucous secretion and constipation). Anticholinergic drugs block the chemical acetylcholine, which is involved in the transmission of electrical impulses between nerve cells. The drugs in question have a range of applications, from blocking hayfever to improving breathing in some chronic lung conditions. Researchers found that the 4% of people who used drugs with definite anticholinergic effects had a small but significantly greater decline in mental ability compared to people not using these drugs. People using drugs with definite or possible anticholinergic effects had an increased risk of death within the two-year period.
The study was carried out by researchers from the University of East Anglia, University of Cambridge and other institutions in the US and UK. Funding was provided by the Medical Research Council. The study is awaiting publication in the Journal of American Geriatrics Society, a peer-reviewed medical journal This was a retrospective analysis of data from participants enrolled in a large ongoing, observational study, called the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS).
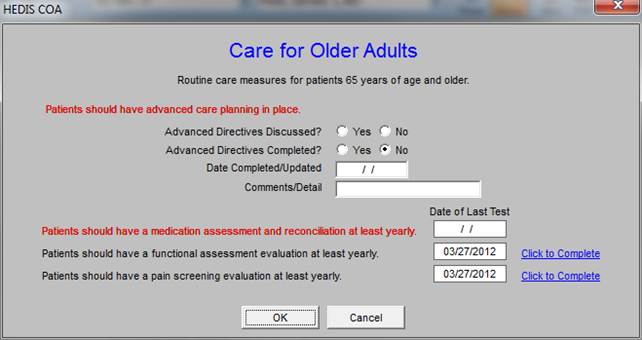
The next metrics is care for older adults. SETMA has functions built for assessing:
- Functional Status
- Pain
- Fall Risk
- Stress
- Wellness
Each of these assessments can be reviewed at Electronic Patient Management Tools, Specialized Tools, Patient-Centered Medical Home Annual Questionnaires
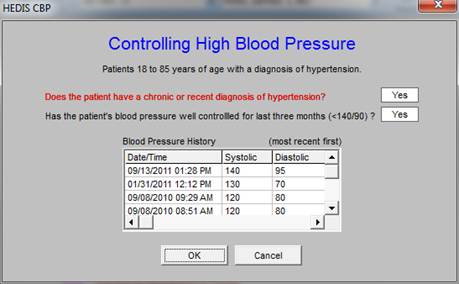
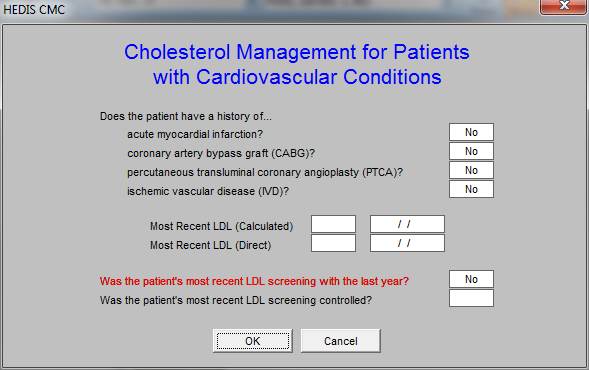
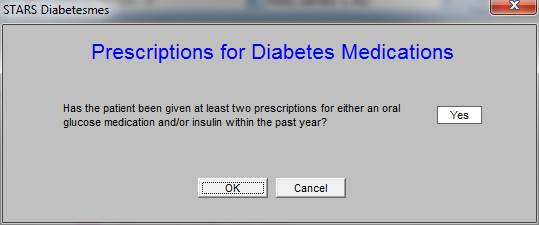
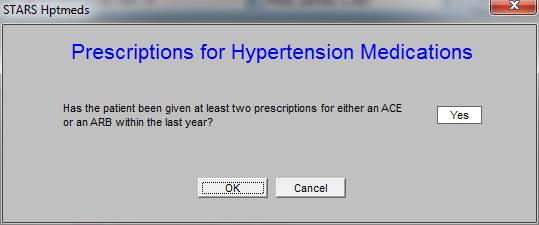
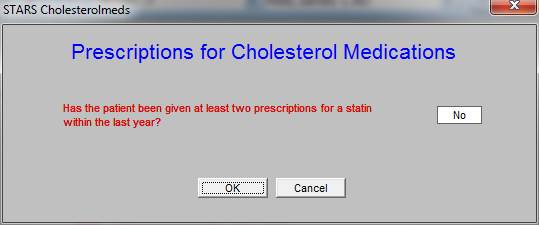
The next three measures are sets of metrics which related to hypertension, cholesterol and diabetes. Later, there are three measures which related to the prescribing of medications for hypertension, cholesterol and diabetes.
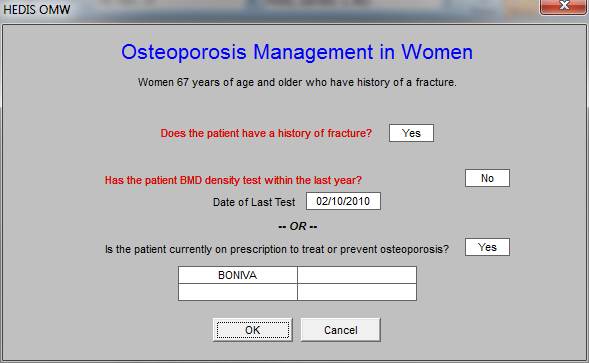
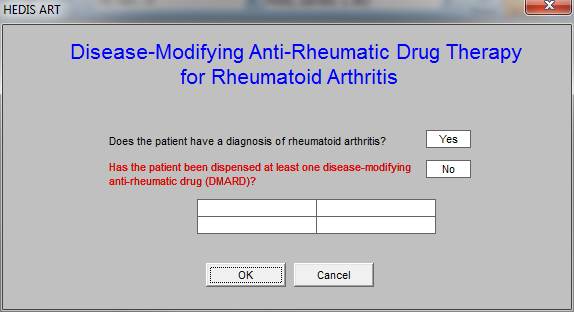
The next two measures have to do with osteoporosis in women who have had a fracture and with the treatment of patients who have rheumatoid arthritis.
These last three measures have to do with prescribing of medications for three conditions: diabetes, hypertension and cholesterol.
This metric calls for all patients to be on an ACE or an ARB. Sometimes that is not appropriate but we live with the metric until we are able to influence its being changed.
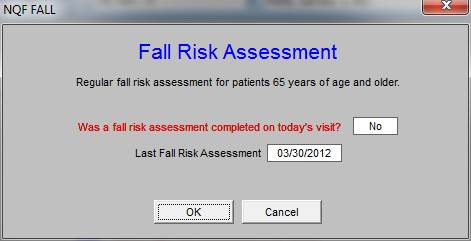
The metric for Fall Risk Assessment for STARs is annually, but it is such an important issue SETMA modified it to the less precise “regular,” to encourage more frequent assessment of this issue.
|