|
This template can be accessed from:
AAA Home
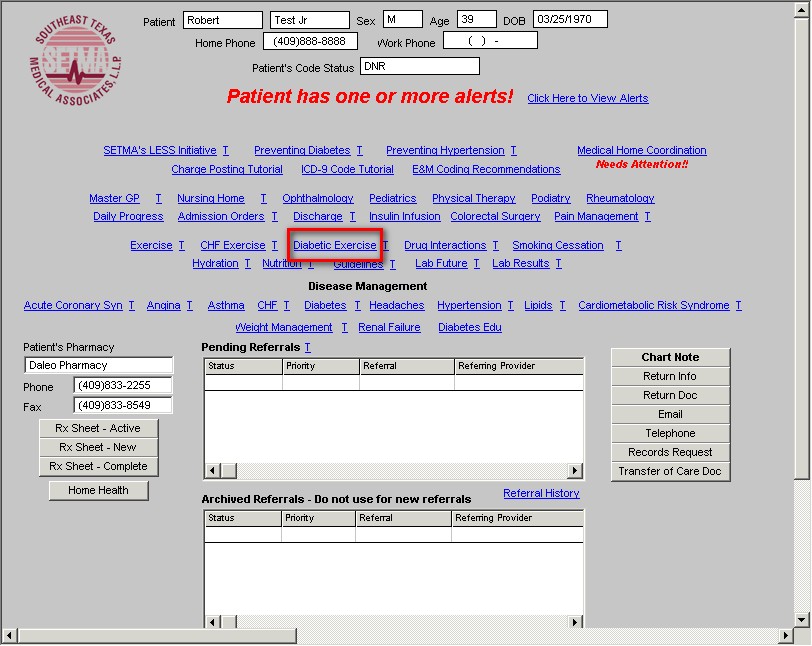
LESS Initiative
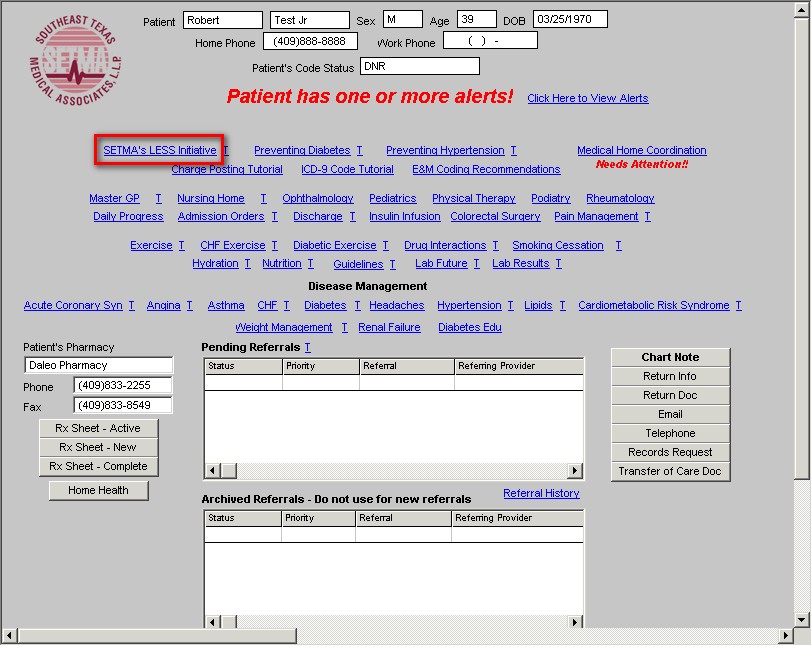
Main Tool Bar
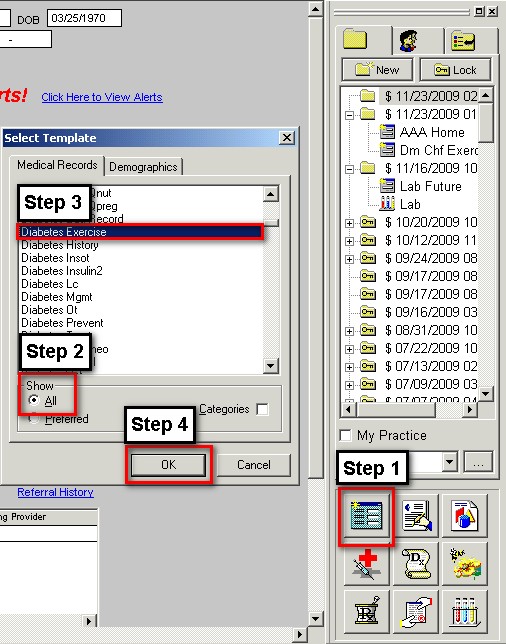
- When the Template button is clicked you will be presented with the preference list.
- If the Diabetes Exercise Template is listed as one of your preferences, select it.
- If it is not one of your preferences, select the All radio button and scroll down until you find it in the list. Then you may select the template by either double-clicking on the name or single click on the name (so that it is highlighted in blue) and then click the OK button.
NOTE: For more on how to set up your preferences, Click Here
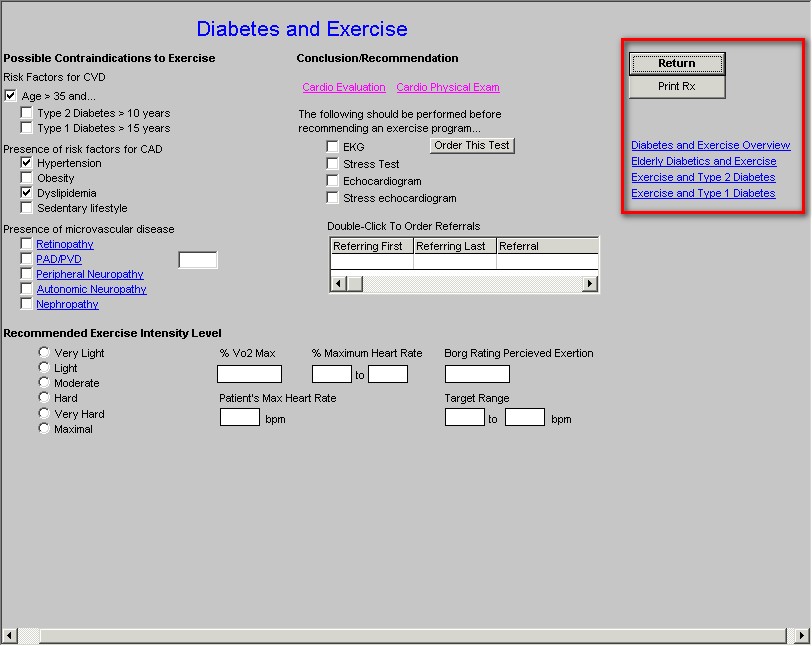
The Diabetes Exercise Prescription template is organized into three columns.
Column 1 -
Possible Contraindications to exercise
There are three groups of cautions for exercise with patients who have diabetes. None of these are absolute contraindications but represent cautionary guides to help patients with diabetes improve their glycemic levels with safe physical training or activities. The cautions are indicated by:
- Type 2 Diabetes >10 years
- Type 1 Diabetes >15 years
Patients with longstanding diabetes are at higher risk for cardiovascular disease, as the very presence of diabetes is a cardiovascular risk equivalent, which means that a patient with diabetes is at the same risk for a future cardiac event as a person who has already had a heart attack or other cardiac event. Therefore, exercise programs in patients with diabetes ought to be started but they ought to be started with caution.
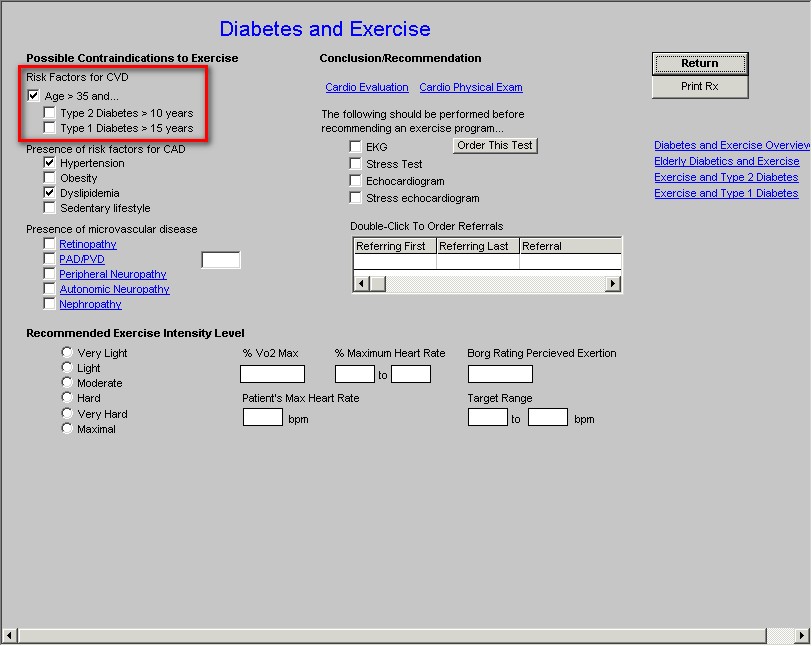
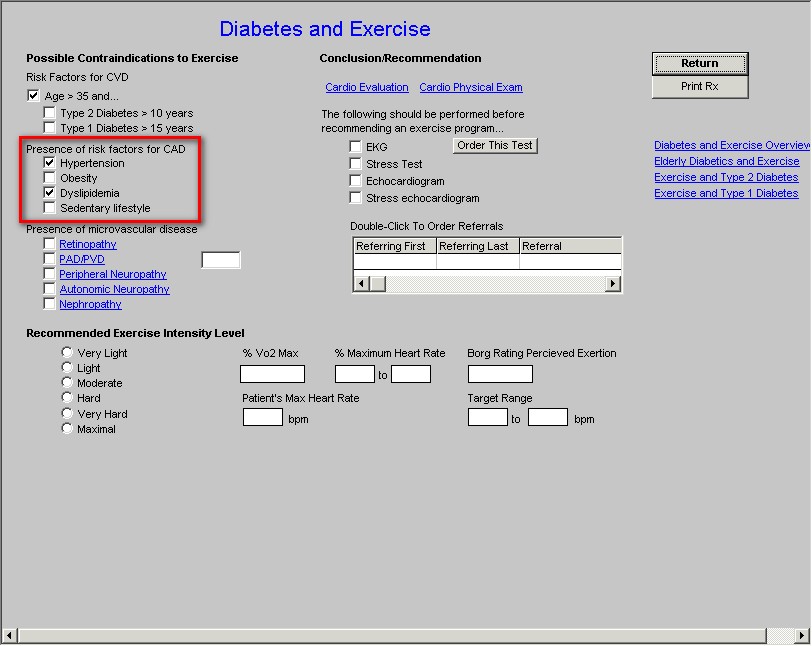
- Presence of Risk Factors for CAD
- Hypertension
- Obesity
- Dyslipidemia
- Sedentary Lifestyle
The presence of other risk factors for cardiovascular disease makes it more likely that the patient with diabetes may need cardiac evaluation before beginning a new exercise program, particularly if they are interested in a strenuous program. In column 2, this template offers the opportunity to order cardiovascular testing for screening patients with diabetes before beginning such an program.
- Presence of Microvascular Disease
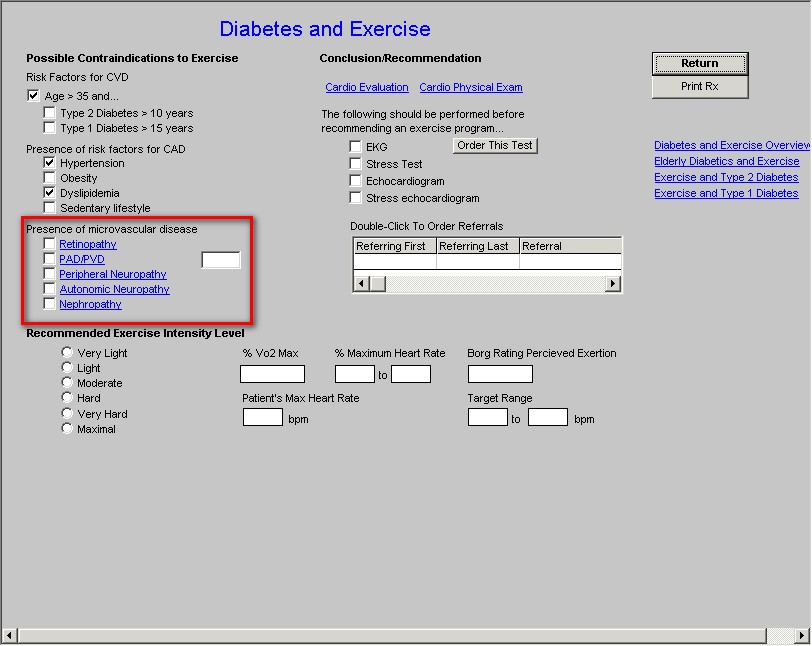
- Retinopathy
- PAD/PVD
- Peripheral Neuropathy
- Autonomic Neuropathy
- Nephropathy
Any of the five categories of microvascular disease have implications for exercise. These will be examined in detail below.
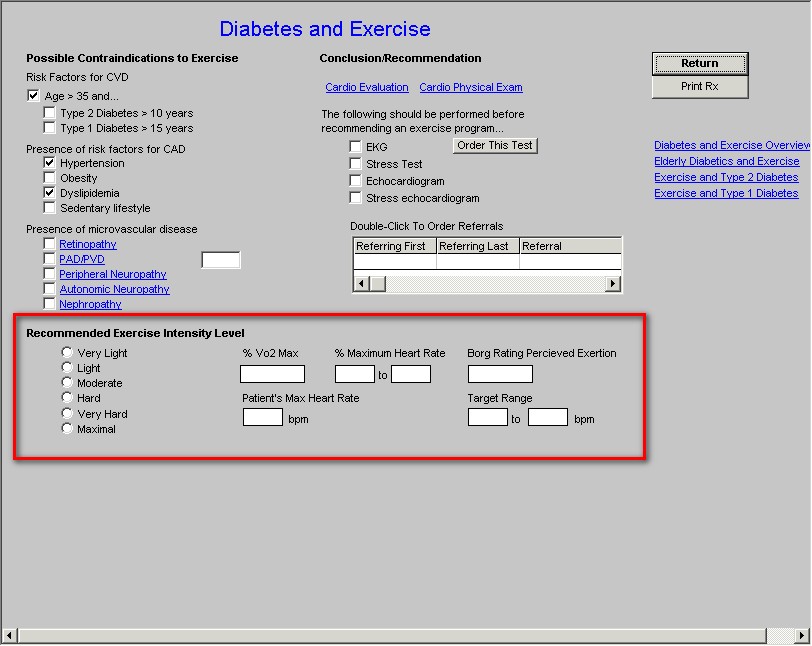
Recommended Exercise Intensity Level
Based on the evaluation above, an exercise intensity level can be selected among the following options:
- Very Light
- Light
- Moderate
- Hard
- Very Hard
- Maximal
When selected, the following data is displayed on the template and subsequently added to the patients Diabetes Exercise Prescription. That data includes:
- %Vo2Max
- % Maximum Heart Rate
- Borg Rating Perceived Exertion
- Patient's Max heart Rate
- Target Range
Column 2 -
Conclusion/Recommendation
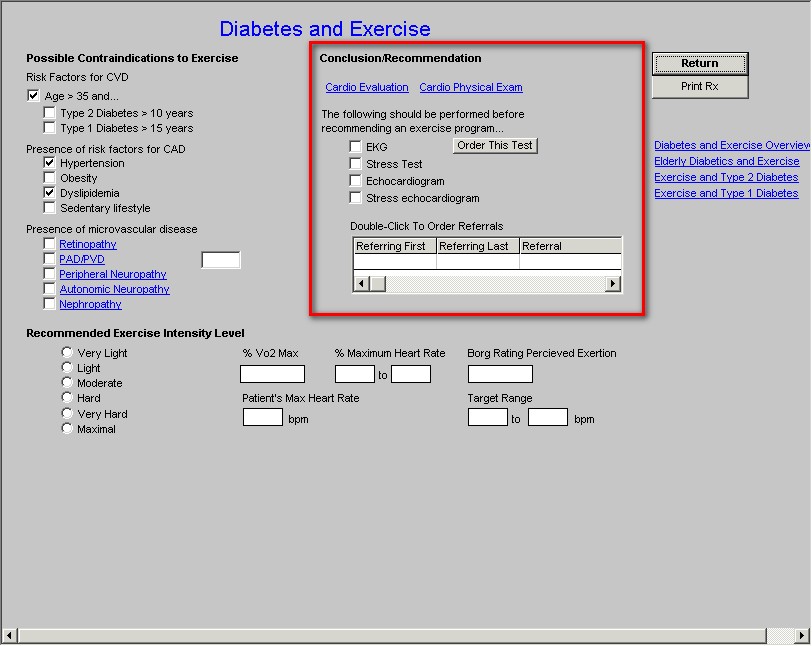
First there are two buttons with the following titles:
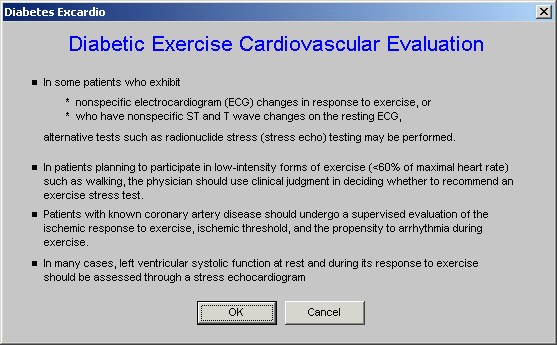
Cardio Evaluation - when clicked this launches a pop-up with the following information:
In some patients who exhibit
- Nonspecific electrocardiogram (ECG) changes in response to exercise, or
- Who have nonspecific S and T wave changes on the resting ECG,
Alternative tests such as radionuclide stress (stress echo) testing may be performed.
- In patients planning to participate in low-intensity forms of exercise (<60% of maximal heart rate) such as walking, the physician should use clinical judgment in deciding whether to recommend an exercise stress test.>
- Patients with known coronary artery disease should undergo a supervised evaluation of the ischemic response to exercise, ischemic threshold and the propensity to arrhythmia during exercise.
- In many cases, left ventricular systolic function at rest and during its response to exercise should be assessed through a stress echocardiogram.
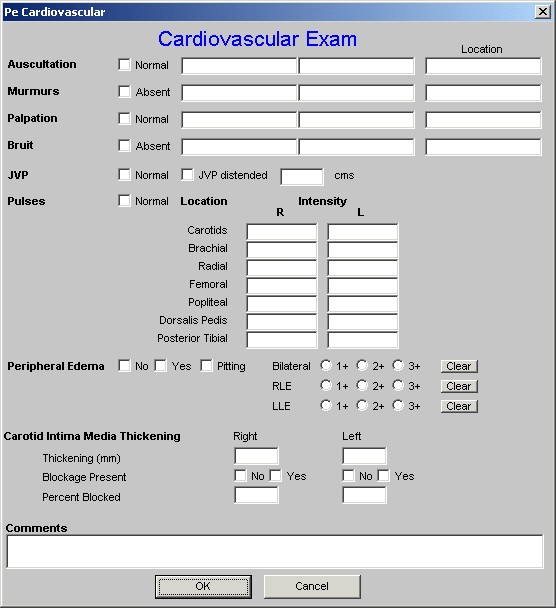
Cardio Physical Exam
This launches the cardiovascular template from the Master GP template which allows you to document any pertinent changes to the patient's cardiovascular system which might give you data with which to decide what type of testing may or may not be needed.
Beneath these two buttons is a charge posting function for
- EKG
- Stress Test
- Echocardiogram
- Stress Echocardiogram
There is also a button entitled "Order This Test" which will charge post when the test is selected and the button is depressed.
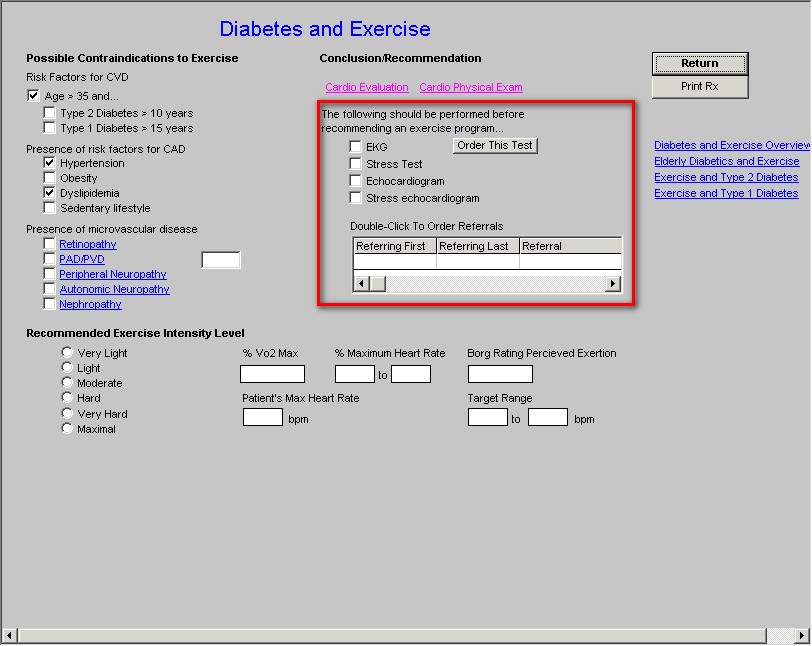
Beneath this function there is a link to the Referral template for the Stress Test, Echocardiogram and Stress Echocardiogram.
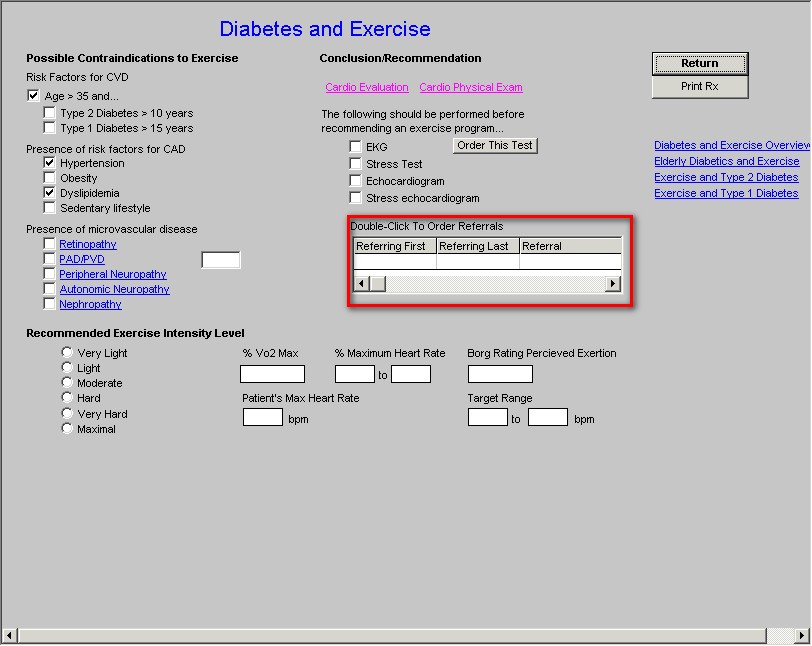
Column 3 -
- There is a Return button which takes you back to the LESS Initiative Main template
- There is a Print Rx button which prints the Diabetes Exercise Prescription which is discussed below.
Finally in the third column, the following documents can be printed:
- Diabetes and Exercise Overview
- Elderly Diabetics and Exercise
- Exercise and Type 2 Diabetes
- Exercise and Type 1 Diabetes
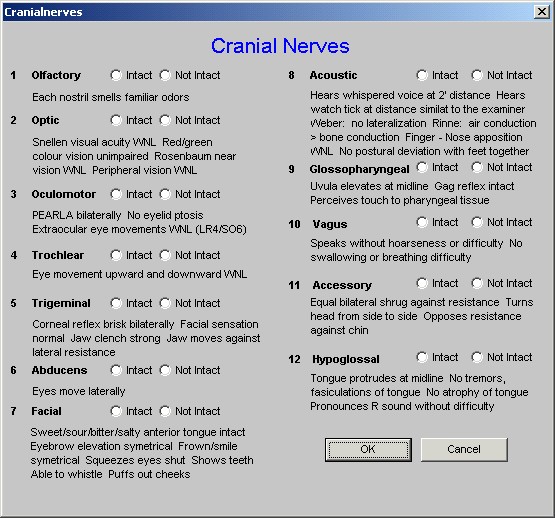
More detail on the five categories of microvascular complications of diabetes and their implications for exercise prescriptions for patients with diabetes.
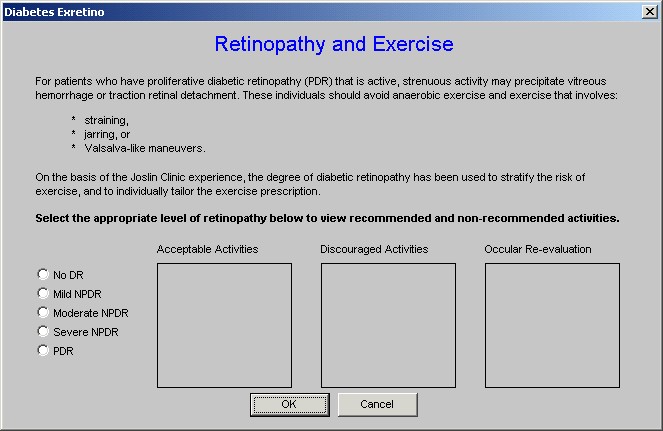
- Retinopathy - this is the first category of microvascular complications. If the patient has retinopathy, you should check the check box next to the name and then click the hyperlink entitled "Retinopathy." This displays the following:
For patients who have proliferative diabetic retinopathy (PDR) that is active, strenuous activity may precipitate vitreous hemorrhage or traction retinal detachment. These individuals should avoid anaerobic exercise and exercise that involves strain, jarring, or valslava-like maneuvers.
On the basis of the Joslin Clinic experience, the degree of diabetic retinopathy has been used to stratify the risk of exercise, and to individually tailor the exercise prescription.
Instructions are then given on the template to "Select the appropriate level of retinopathy below to view recommended and non-recommended activities.
The options are:
- No DR (No Retinopathy)
- Mild NPDR (Non-proliferative Diabetic Retinopathy)
- Moderate NPDR (Non-proliferative Diabetic Retinopathy)
- Severe NPDR (Non-proliferative Diabetic Retinopathy)
- PDR (Proliferative Diabetic Retinopathy)
When the radial button next to these options is selected, boxes entitled
- Acceptable Activities.
- Discouraged Activities and
- Ocular re-evaluation
are populated. From these instructions, a decision about the level of intensity of exercise can be made.
The next microvascular complication is:
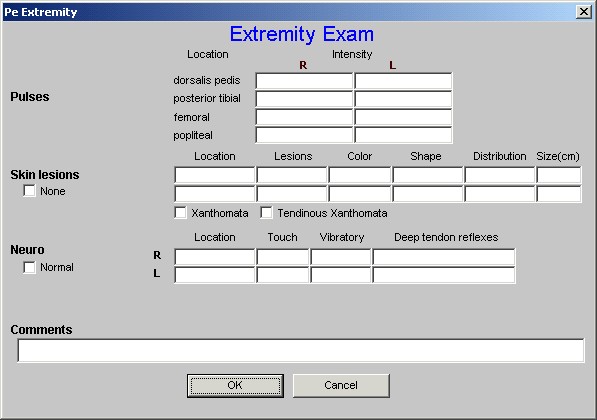
- PAD/PVD - when the check box next to this option is selected, the hyperlink entitled PAD/PVD (Peripheral Artery Disease/Peripheral Vascular Disease) should be clicked. This will launch the following information on a pop-up.
Evaluation of peripheral arterial disease (PAD) is based on signs and symptoms including.
- Intermittent Claudication
- Coldness of the extremity
- Decreased or absent pulses
- Atrophy of subcutaneous tissues
- Hair Loss on extremity
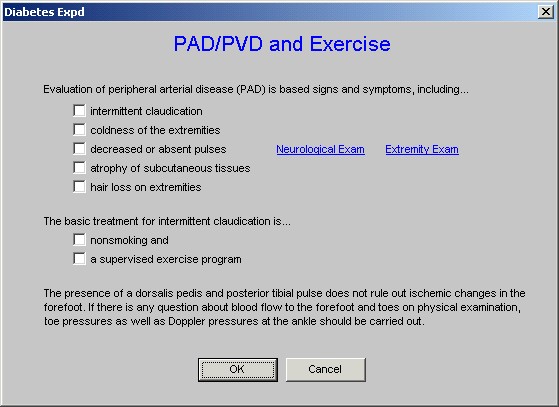
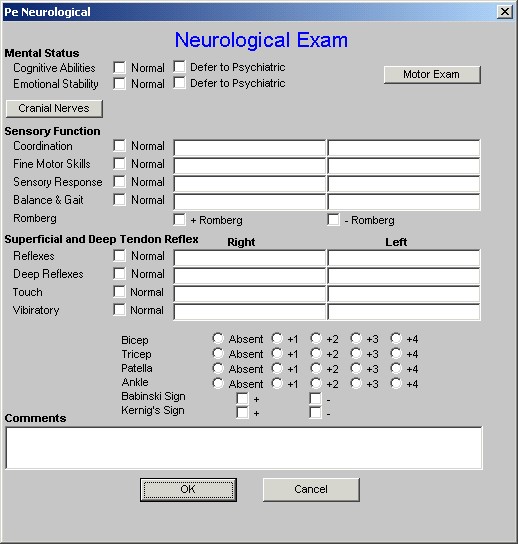
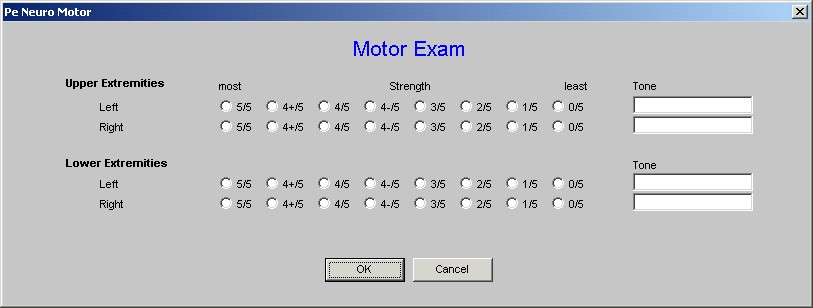
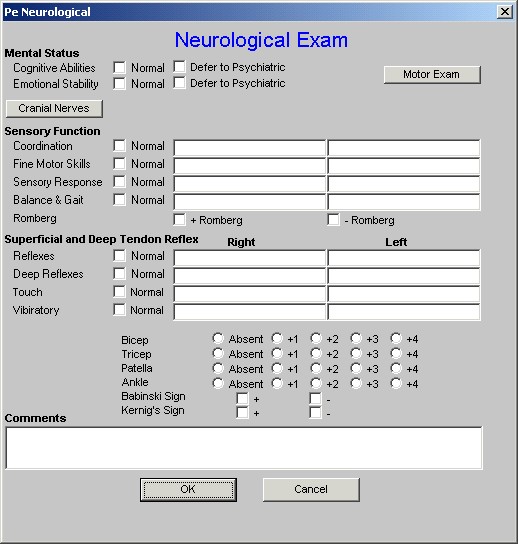
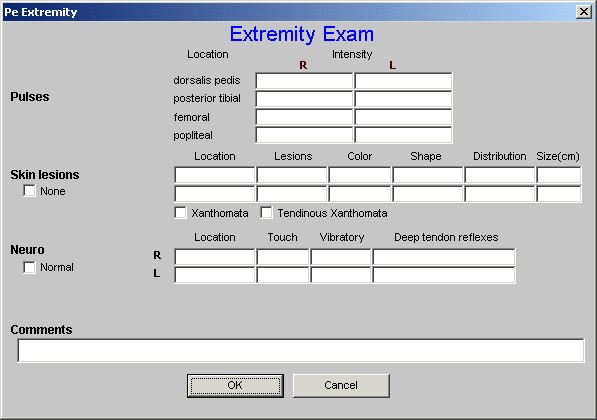
Next to these five options are links to the Master GP Neurological Exam and Extremity Exam. They enable the elements of PAD to be properly assessed and documented.
The basic treatment for intermittent claudication is;
- Nonsmoking and
- A supervised exercise program
The presence of a dorsalis pedis and posterior tibial pulse does not rule out ischemic changes in the forefoot. If there is any question about blood flow to the forefoot and toes on physical examination, toe pressures as well as Doppler pressures at the ankle should be carried out.
The next category of micovascular disease is
- Peripheral Neuropathy - when the check box next to this option is checked, the hyperlink named Peripheral Neuropathy should be clicked which will launch a pop-up with the following displayed:
Peripheral Neuropathy and Exercise
Peripheral neuropathy (PN) may result in loss of protective sensation in the feet. Significant PN is an indication to limit weight-bearing exercise.
- Repetitive exercise on insensitive feet can ultimately lead to ulceration and fractures.
- Evaluation of PN can be made by checking the
- Deep Tendon reflexes
- Vibratory Sense
- Position sense
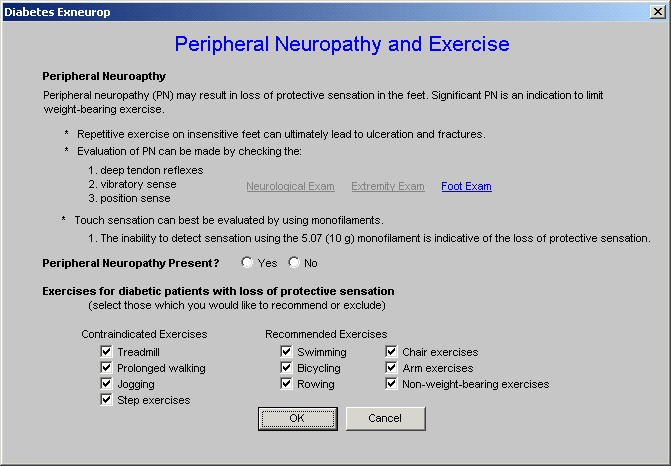
- Note: Next to these options are links to the Master GP Neurological Exam, Extremity Exam and Foot Exam.
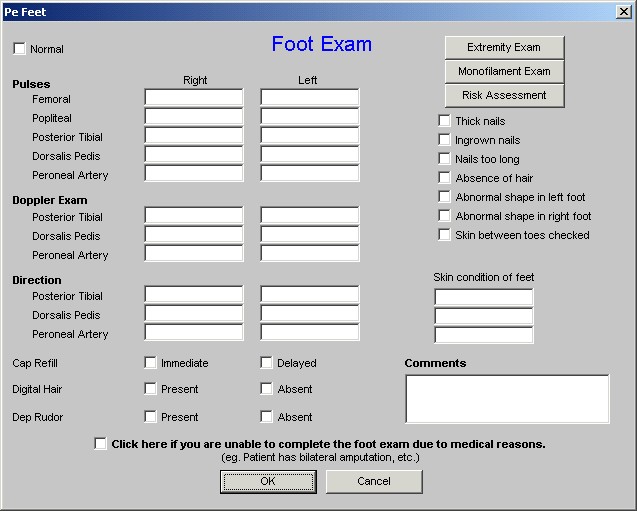
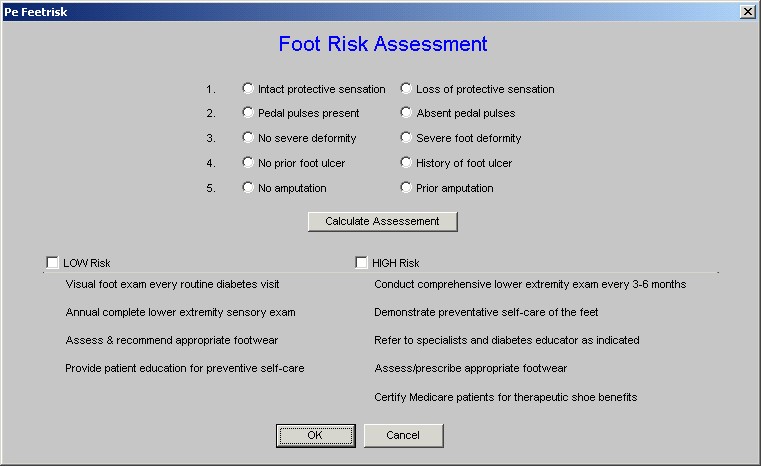
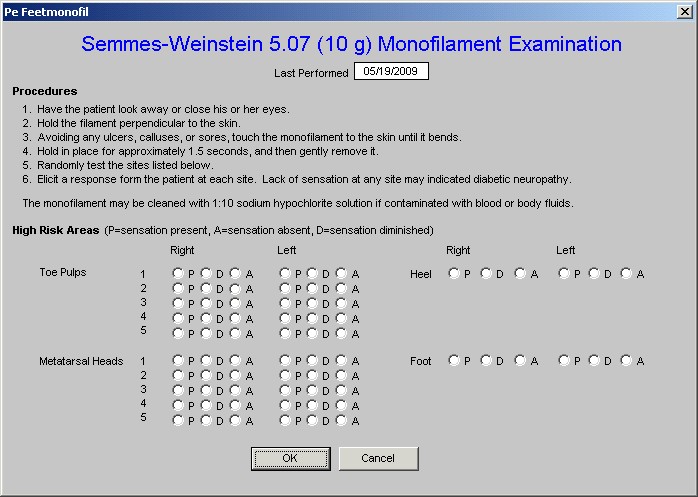
Touch sensation can best be evaluated by using monofilaments. The inability to detect sensation using the 5.07 (do gram) monofilament is indicative of the loss of protective sensation.
Peripheral Neuropathy Present Yes No
Exercise for diabetic patients with loss of protective sensation
(Select those which you would like to recommend or exclude)
Contraindicated Exercises
- Treadmill
- Prolonged walking
- Jogging
- Step exercises
Recommended Exercise
- Swimming
- Bicycling
- Rowing
- Chair Exercises
- Arm Exercises
- Non-weight-bearing exercise.
The next category of micovascular complications which can impact exercise in the patient with diabetes is Autonomic Neuropathy.
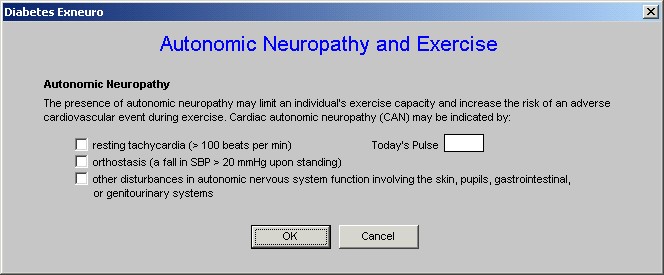
- Autonomic Neuropathy - if the check box is checked or if this is a concern, the Autonomic Neuropathy hyperlink should be clicked. This launches a pop-up which states:
The presence of autonomic neuropathy may limit an individual's exercise capacity and increase the risk of an adverse cardiovascular event during exercise. Cardiac autonomic neuropathy (CAN) may be indicated by
- Resting tachycardia (>100 beats per minute)
- Orthostasis (a fall in SBP > 20 mmHg upon standing)
- Other disturbances in autonomic nervous system function involving the skin, pupils, gastrointestinal, or genitourinary systems.
The patient's pulse is automatically populated to this template in a box entitled Today's Pulse.
The fifth and final category of microvascular complications in the patient with diabetes which can impact the exercise prescription is Nephropathy.
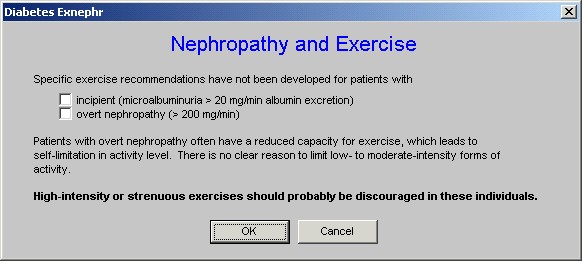
- Nephropathy -if the patient has nephropathy, the hyperlink should be clicked which launches a pop-up which states:
Specific exercise recommendations have not been developed for patients with
- Incipient (microabluminuia >20 mg/min albumin excretion)
- Overt nephropathy (> 200 mg/min)
Patients with overt nephropathy often have a reduced capacity for exercise, which lead to self-limitation in activity level. There is no clear reason to limit to low- to moderate-intensity forms of activity.
High-intensity or strenuous exercises should probably be discouraged in these individuals.
All of the information on the microvascular complications will print on your Diabetic Exercise Prescription.
The following is an analysis of the Diabetic Exercise Prescription
Diabetic Exercise Prescription
Part 1 -
This gives general principles about the amount of exercise a patient with diabetes should have.
General Principles
The recent Surgeon Generals Report on Physical Activity and Health underscores the pivotal role physical activity plays in health promotion and disease prevention.
- It recommends that individuals accumulate 30 min of moderate physical activity on most days of the week.
- In the context of diabetes, it is becoming increasingly clear that the epidemic of type 2 diabetes sweeping the globe is associated with decreasing levels of activity and an increasing prevalence of obesity.
- Thus, the importance of promoting exercise as a vital component of the prevention as well as management of type 2 diabetes must be viewed as a high priority.
- It must also be recognized that the benefit of exercise in improving the metabolic abnormalities of type 2 diabetes is probably greatest when it is used early in its progression from insulin resistance to impaired glucose tolerance to overt hyperglycemia requiring treatment with oral glucose-lowering agents and finally to insulin.
For people with type 1 diabetes, the emphasis must be on adjusting the therapeutic regimen to allow safe participation in all forms of physical activity consistent with an individuals desires and goals. Ultimately, all patients with diabetes should have the opportunity to benefit from the many valuable effects of exercise.
Part 2 -
This begins to give details about exercise by a patient with diabetes, the warm up and cool down phrase are particularly important in a diabetic.
Warm Up/Cool Down
A standard recommendation for diabetic patients, as for nondiabetic individuals, is that exercise includes a proper warm-up and cool-down period.
- A warm-up should consist of 5-10 min of aerobic activity (walking, cycling, etc.) at a low-intensity level.
- The warm-up session is to prepare the skeletal muscles, heart, and lungs for a progressive increase in exercise intensity.
- After a short warm-up, muscles should be gently stretched for another 5-10 min.
- Primarily, the muscles used during the active exercise session should be stretched, but warming up all muscle groups is optimal.
- The active warm-up can either take place before or after stretching.
- After the activity session, a cool-down should be structured similarly to the warm-up.
- The cool-down should last about 5-10 min and gradually bring the heart rate down to its pre-exercise level.
Part 3 -
This addresses the importance of foot care in patients with diabetes who are exercising.
Foot Care, Equipment, and Identification
There are several considerations that are particularly important and specific for the individual with diabetes.
- Aerobic exercise should be recommended, but taking precautionary measures for exercise involving the feet is essential for many patients with diabetes.
- The use of silica gel or air midsoles as well as polyester or blend (cotton-polyester) socks to prevent blisters and keep the feet dry is important for minimizing trauma to the feet.
- Proper footwear is essential and must be emphasized for individuals with PN.
- Individuals must be taught to monitor closely for blisters and other potential damage to their feet, both before and after exercise.
- A diabetes identification bracelet or shoe tag should be clearly visible when exercising.
Part 4 -
This addresses the critical issue of hydration in patients with diabetes who are exercising.
Hydration During Exercise for Diabetics
Proper hydration is also essential, as dehydration can effect blood glucose levels and heart function adversely.
- Exercise in heat requires special attention to maintaining hydration. Adequate hydration prior to exercise is recommended (e.g., 17 ounces of fluid consumed 2 h before exercise).
- During exercise, fluid should be taken early and frequently in an amount sufficient to compensate for losses in sweat reflected in body weight loss, or the maximal amount of fluid tolerated.
- Precautions should be taken when exercising in extremely hot or cold environments.
- High-resistance exercise using weights may be acceptable for young individuals with diabetes, but not for older individuals or those with long-standing diabetes.
- Moderate weight training programs that utilize light weights and high repetitions can be used for maintaining or enhancing upper body strength in nearly all patients with diabetes.
Part 5 -
This draws material from the Diabetic Exercise Template which is specific for this patient and displays it for the patient's benefit.
Possible Diabetic Contraindications to Exercise
Risk Factors for CAD
- Hypertension
- Dyslipidemia
Retinopathy
Level of Retinopathy - Mild NPDR
As a result of your retinopathy status, the activities listed below are ACCEPTABLE forms of exercise.
Dictated by medical status
As a result of your retinopathy status, the activities listed below are DISCOURAGED forms of exercise.
Dictated by medical status
Peripheral Neuropathy
Peripheral Neuropathy - Present
As a result of your peripheral neuropathy status, the activities listed below are ACCEPTABLE forms of exercise.
- Swimming
- Bicycling
- Rowing
- Chair exercises
- Arm exercises
- Non-weight-bearing exercises
As a result of your peripheral neuropathy status, the activities listed below are DISCOURAGED forms of exercise.
- Treadmill
- Prolonged walking
- Jogging
- Step exercises
Nephropathy
As a result of your nephropathy status, you should AVOID high-intensity or strenous levels of exercise.
Part 6 -
This displays the recommended exercise on the basis of your choice made according to the algorithm above.
Recommended Exercise
Intensity Level - Moderate
Your maximum heart rate is 147.0 beats per minute. Based on the recommended intensity level, your target heart rate during exercise is between 80 and 101 beats per minute.
Part 7 -
This gives the Borg Rating of Perceived Exertion for the patient to report to their subjective judgment of their exercise program.
You should exercise at a Borg Rating Perceived Exertion of 12-13. See the key below.
Borg's Ratings of Perceived Exertion (RPE)
6 |
No exertion at all |
7-8 |
Extremely light (very, very light) |
9-10 |
Very light (warm-up/recovery) |
11 |
Light |
12-13 |
Moderate |
14-15 |
Hard |
16-17 |
Very hard |
18-19 |
Extremely hard |
20 |
Maximum all-out effort with absolutely nothing being held in reserve |
Exercise is critical for the patient with diabetes; it is equally critical that it be done safely. You can help patients by prescribing proper exercise for them.
|