|
Since its founding in 1995, SETMA has worked toward the effective use of a team approach to healthcare. In the intervening eighteen plus years, SETMA has developed numerous electronic tools since adopting EMR in 1998. These tools are the result of a May, 1999 decision not to simply pursue electronic medical records but to pursue electronic patient management.
It was in that month that SETMA defined the principles which would guide the development of the EMR. Those principles provided the foundation of our transformation of the delivery of healthcare. There were two aspects of that transformation. The first was structural; the second was dynamic. The structural change, being based on electronic patient records and electronic patient management of patients, was essential and in some ways it was easier than the required dynamic change.
Ten years before SETMA knew about medical home, we defined both the structure and the dynamic of patient-centered medical home. We just did not know it. In May, 1999, SETMA defined the principles which guided our development and which set us on the course to forming, becoming and practice medical home. Those principles guided the structural changes which would prepare us to become a medical home, and they defined much of the dynamic changes which would make us a true medical home. Those principles were:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
Remember, these principles were defined over thirteen years ago. If reiterated today, these principles would be slightly changed but it is useful to see them as they were stated early in our development. It is helpful for us and others to see that even before we knew the name “medical home,” we intuitively began developing the pieces of this new, but old, dynamic of healthcare delivery.
When SETMA set on the conscious course in February, 2009 of formally becoming a medical home, and when SETMA achieved its first recognition by NCQA of a Tier III Patient-Centered Medical Home in June, 2010 and its first accreditation by AAAHC of Ambulatory Care and Medical Home in August, 2010, less than 0.1% of primary care practices were medical homes. Today, “roughly fifteen percent of all U.S. primary care practices are now recognized by the National Committee for Quality Assurance as ‘medical homes.’ (“Building a Health Care Workforce for the Future: More Physicians Professional Reforms, and Technological Advances,” Health Affairs, November, 2013, Volume 32 no. 11, 1922-1927) (December 10-20, 2013, SETMA has a survey by URAC for Medical Home and in the first quarter of 2014, we will submit an application to the Joint Commission for Medical Home accreditation.)
Displaying SETMA’s Patient-Centric Tools
In this context, and because of the number of transformative and patient-centric tools SETMA has developed, we wanted to display these tools in relationship to medical-home functions so that visitors to our website and new colleagues with SETMA could understand how all of the tools fit together and how they address critical elements of medical home.
SETMA’s Academic Teaching Pursuits
As can be seen below on the screen shot from SETMA’s website (www.jameslhollymd.com), at the top of the middle column, we have deployed the Syllabus for PC-MH Externship for senor medical students and for primary care residents in academic graduate medical education programs. Most of SETMA’s healthcare leadership holds academic appointments at Texas Schools of Medicine and all of SETMA’s healthcare providers, physicians and nurse practitioners, participate in training nurse practitioner students, senior medical students and post-graduate primary care residents. The content of the 1,100 page syllabus by sections can be seen below.
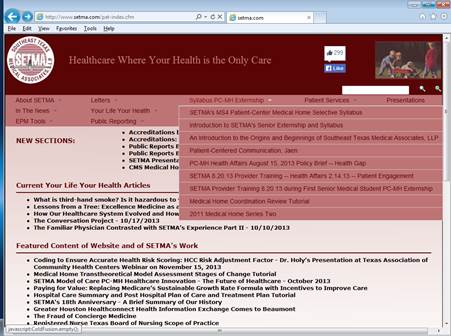
A two-volume printed version of this Syllabus is presented to each participant in SETMA’s Medical Home Externship. (Everything on SETMA’s website is in the public domain and is free for use by anyone without cost.)
In addition, for the benefit of third-year residents in Graduate Medical Education another syllabus is being prepared on practice management, patient-centered medical home cash management, continuous quality improvement, personnel management and other subjects critical to successfully operating a patient-centered medical home.
Medical Home and Medical Neighborhood
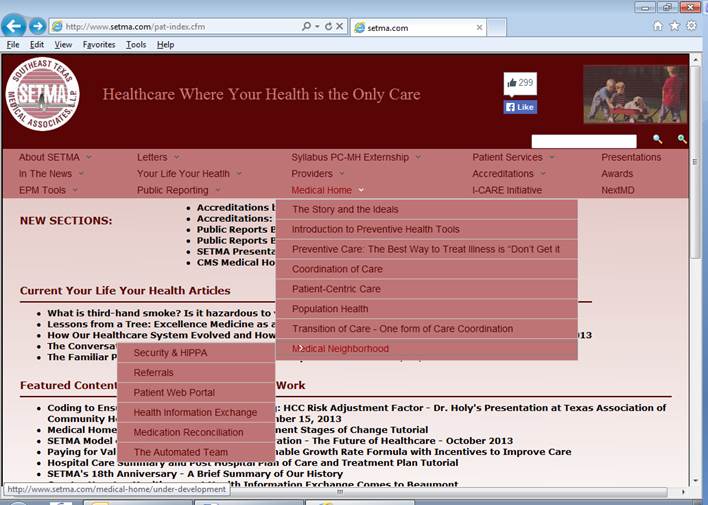
Beneath the Syllabus content is another website section entitled Medical Home. If you click on the main section entitled Medical Home, the complete document with indices can be seen. Beneath the Medical Home heading there are seven sections on the drop down menu which display each section of this part of the website. The eighth drop down menu is entitled Medical Neighborhood beneath which there are displayed six sections of the Medical Neighborhood. Here the tools necessary for enabling multiple medical homes to relate and to communicate with one another are discussed.
By clicking on Medical Home, the entire discussion of the elements of SETMA’s medical home can be seen: http://jameslhollymd.com/medical-home. And yet, this is not all of SETMA’s information and tools about Medical Home. At the following links other Medical Home materials are displayed:
Index to Medical Home: The Story and the Ideals
The following is the index to the Medical Home: the Story and the Ideals. This index is made up of hyperlinks, which allow the reader to easily access the element of SETMA’s medical home he/she wish to review. Going forward, this display will be broadened, and additional materials will be added.
Medical Home
SETMA, LLP
The Story and the Ideals
The Story and the Ideals
Introduction to Preventive Health Tools
Preventive Care: The Best Way to Treat Illness is “Don’t Get it”
Coordination of Care
Patient-Centric Care
Population Health
Transition of Care - One form of Care Coordination
Public Reporting
http://jameslhollymd.com/public-reporting/public-reports-by-type
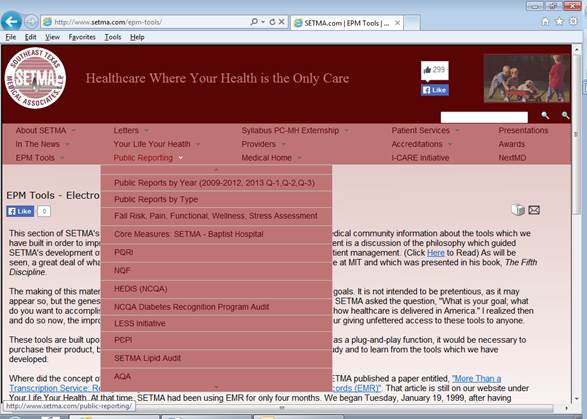
A key element to SETMA’s medical home is transparency with our patients and community particularly by public reporting by provider name. The following screen shot displays SETMA’s Public Reporting by Provider Name of over 300 Quality Metrics. These are displayed by Type of Metric and by Year (2009, 2010, 2011, 2012, 2013). The link above is to the Public Reporting by Type.
Kaizen
Recently, a New York-based physician and healthcare executive said that SETMA has “kaizen” - a Japanese word meaning, “a system of continuous improvement in quality, technology, processes, company culture, productivity, safety and leadership. Kaizen was created in Japan following World War II. The word Kaizen means "continuous improvement". It comes from the Japanese words  ("kai") which means "change" or "to correct" and ("kai") which means "change" or "to correct" and  ("zen") which means "good". Kaizen is a system that involves every employee - from upper management to the cleaning crew. Everyone is encouraged to come up with small improvement suggestions on a regular basis. This is not a once a month or once a year activity. It is continuous. Japanese companies, such as Toyota and Canon, a total of 60 to 70 suggestions per employee per year are written down, shared and implemented. ("zen") which means "good". Kaizen is a system that involves every employee - from upper management to the cleaning crew. Everyone is encouraged to come up with small improvement suggestions on a regular basis. This is not a once a month or once a year activity. It is continuous. Japanese companies, such as Toyota and Canon, a total of 60 to 70 suggestions per employee per year are written down, shared and implemented.
“In most cases these are not ideas for major changes. Kaizen is based on making little changes on a regular basis: always improving productivity, safety and effectiveness while reducing waste. Suggestions are not limited to a specific area such as production or marketing. Kaizen is based on making changes anywhere that improvements can be made. Western philosophy may be summarized as, ‘if it ain't broke, don't fix it.’ The Kaizen philosophy is to ‘do it better, make it better, and improve it even if it isn't broken, because if we don't, we can't compete with those who do.’
“Kaizen in Japan is a system of improvement that includes both home and business life. Kaizen even includes social activities. It is a concept that is applied in every aspect of a person's life. In business Kaizen encompasses many of the components of Japanese businesses that have been seen as a part of their success. Quality circles, automation, suggestion systems, just-in-time delivery, Kanban and 5S are all included within the Kaizen system of running a business.
Kaizen involves setting standards and then continually improving those standards. To support the higher standards Kaizen also involves providing the training, materials and supervision that is needed for employees to achieve the higher standards and maintain their ability to meet those standards on an on-going basis.”
The Future of SETMA’s Patient-Centered Medical Hoe
This is part of SETMA’s medical home story (history). We expect the future to be much more productive and beneficial to our patients, practice and profession than the past. There are many aspects of our medical home and particularly our medical neighborhood which bridge the past and the future. These aspects were begun in the past, they are continuing to be developed in the present but the ultimate value and fruition will be in the future.
No project is more demonstrative of this than is The Automated Team project. It can be read about by clicking Medical Home/Medical Neighborhood/Automated Team or by clicking on this link: http://jameslhollymd.com/EPM-Tools/Automated-Team-Tutorial-for-the-EMR-Automated-Team-Function
We hope as there were only 0.1% of primary medical practices pursuing medical home when we began our pilgrimage, and as there are presently approximately 15% of practice that are medical home in the United States, that in five years more than 50% of practices will be medical homes and in ten years more than 80% will be transforming themselves into medical homes. If our experience and if our telling of our story help in this process, the effort and cost of this website will have been worth it.
A Celebratory Spirit
We will pursue that future in the future, with the same enthusiasm and with the same celebratory spirit with which we pursued the future in the past. Besides defining our medical home future, in May 1999, we experienced another event which taught us to have a celebratory spirit about the development, progress and improvement in our electronic patient management. In that month, my co-founding partner lamented our level of use of the EHR, when he said, "We aren't even crawling yet." We started using the HER January. 26, 1999. On the 29th, we used the EHR for every patient encounter, and we have done so since. Yet, even with that success, it did seem that we were not moving very fast.
As I listened to my friend and partner, I said, "When your son turned over in bed for the first time, did you call for your wife and say, 'this dimwitted kid can't even walk, all he can do is turn over in bed?'" He smiled and I continued, "You celebrated his achievement. If a year later, all he was doing was turning over in bed, you would have reason to lament, but for the moment enjoy the progress." I concluded, "If in a year, we are doing no more than we are now, I will join you in your lamentation. But for now, I am going to celebrate what we have achieved even if all we have done is to start our pilgrimage to electronic patient management."
Through the years, our vision has grown as to what electronic patient management is, and we have celebrated each advance from having the lab interface up and running, to using the EHR in the hospital for history and physical examinations, to creating discharge summaries in the EHR, and to using the EHR for daily progress notes. We have celebrated the automation of formulas for calculating the stage of renal disease, Framingham Risk Factors, Cardiometabolic Risk Factors, stages of hypertension, Fredrickson's Classifications of Dyslipidemia, Homeostasis Model Assessment (HOMA) of Insulin Resistance, and the list goes on and on and on.
We continue to dream ,and some would say hallucinate, and we continue to celebrate. As the old adage says, "We ain't what we was, and we ain't what we gonna be, but we're moving forward." As it has been, it shall be, and in being, we shall continue to become a vision of the future driven by our passion for the present.
|