|
“The better the primary care, the greater the cost savings, the better the health outcomes, and the greater the reduction in health and health care disparities”
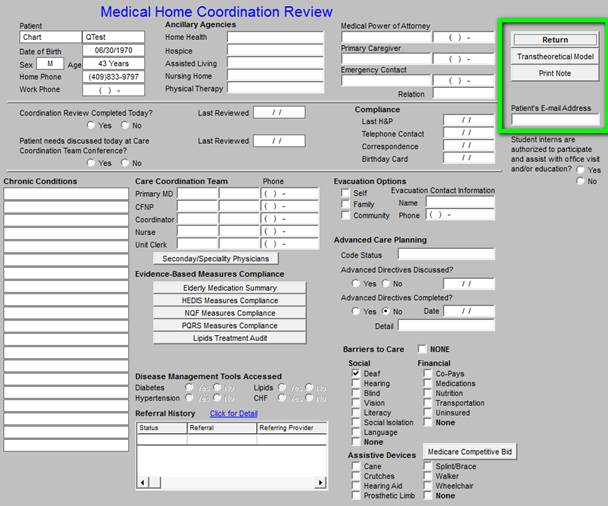
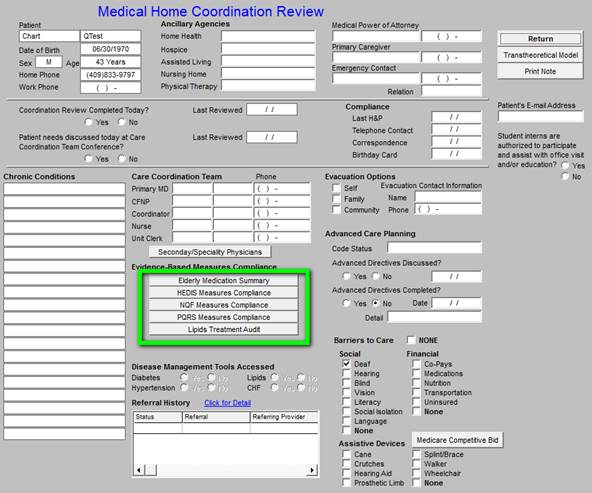
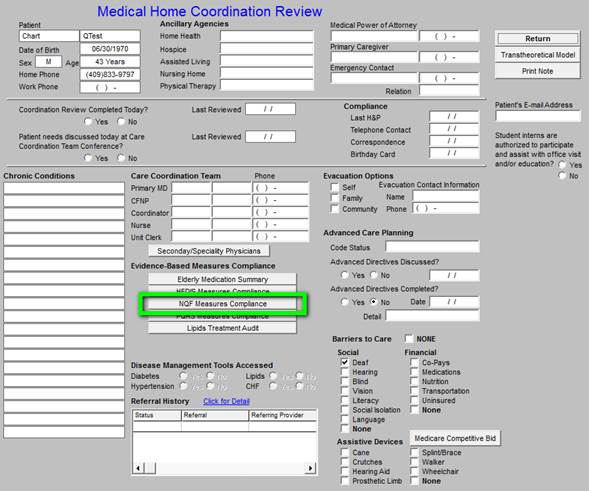
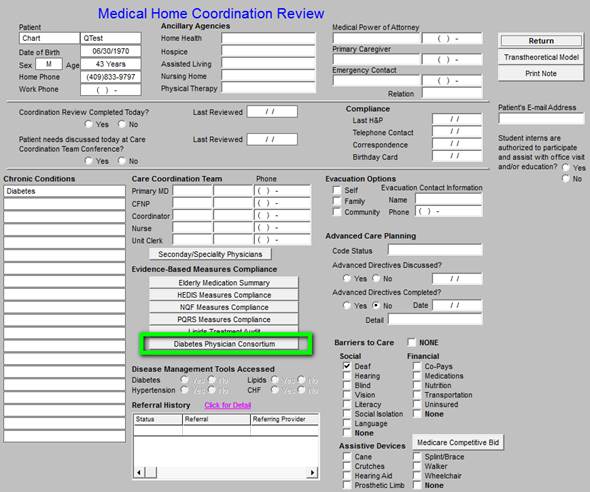
Because care coordination is the heart of the ideal of Medical Home, the hub of SETMA’s Medical Home will be the Medical Home Coordination Review template. When the patient’s care encounter is completed, the patient will be given a document which will summarize all of the Care Coordination issues which will be reviewed in this tutorial. The patient will be charged with the responsibility of directing their own care by requesting the points of care which the quality measures indicate they have not received and which are noted in this Care Coordination review document.
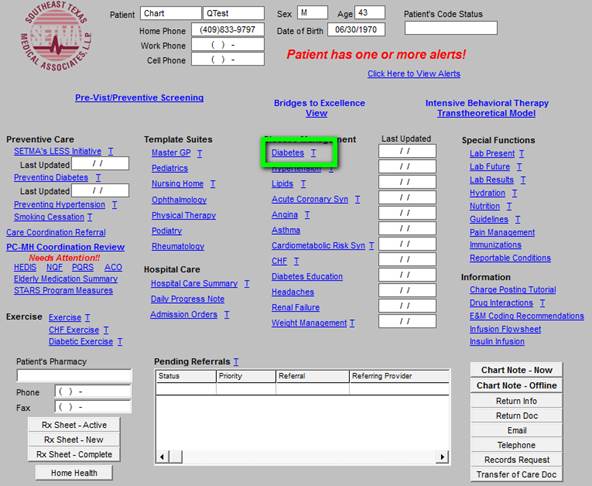
Accessing the Medical Home Coordination Review from AAA Home
There will be two possible alerts on the AAA Home, which address functions of the Medical home Coordination Review; they appear in red and are entitled:
- Patient Has One or More Alerts - appears at the top of the AAA template. This alert refers to barriers to care such as hearing, seeing, reading, etc., which will impact the ability of the patient to receive and to direct their own care.
- Needs Attention-- appears under the Medical Home Coordination Review at the top right of the AAA template. This alert lets the provider know that an element of one or more of the six evidenced-based classes of quality measures which appear on the Medical Home Coordination of Care Review needs attention.
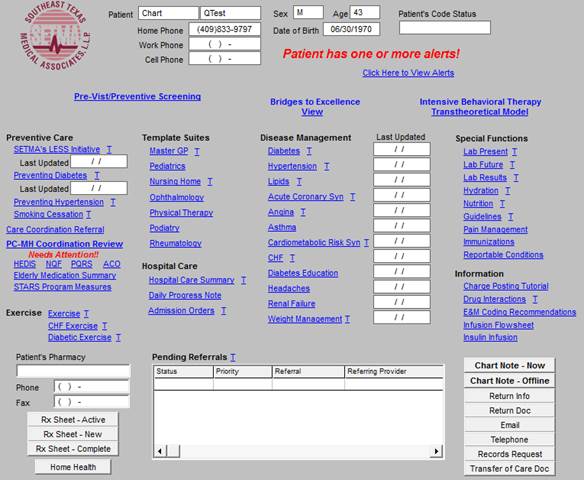
The first alert addresses special patient needs which are documented on the Patient Alert popup which normal launches from the GP Master Template. To the right of this notation, there is a button entitled “click here to view alerts.” When this button is activated, the Patient Alert pop-up is launched.
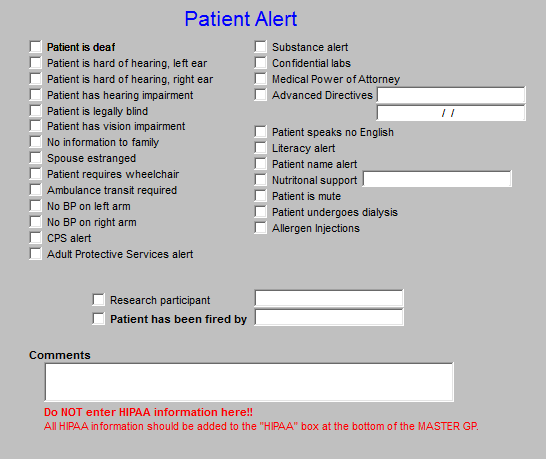
The following are the communication issues which must be displayed:
- Identify and display in the record the language preference of the patient and family
- Assess both hearing and vision barriers to communication
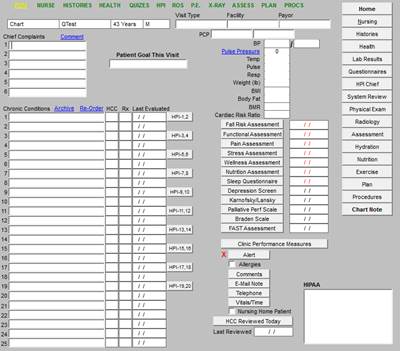
These and other issues related to the patient’s access to care are documented on SETMA’s Patient Alert pop-up which can also be accessed from the GP Master template by clicking on the button entitled Alert which is found in the second column of the GP Master template. See the following screen shot:
The second alert is found on the AAA Home template underneath the Medical Home Coordinationbutton and is entitled “Needs Attention.”
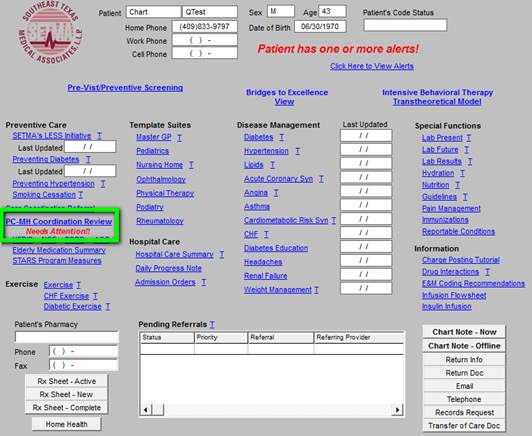
This alerts the provider that there is a deficiency in one or more of the following:
- The Elderly Medication Summary (NCQA)
- The HEDIS Measures (NCQA)
- The NQF Measures (National Quality Forum
)
- The PQRS Measures (Centers for Medicare and Medicaid Services)
- The PCPI Diabetes*
- The PCPI Hypertension*
Each of these functions displays the evidence-based, quality measures published by the identified organization. The compliance of the patient’s care with these measures is automatically displayed for quick and easy review by the provider. These functions will be described below.
Note: While there are six categories of evidenced-based measures which are tracked by SEMTA, numbers 5 and 6 appear only when a patient has diabetes and/or hypertension. If one or both of these buttons do not appear on the Medical Home Coordination Review template,, it is because the patient does not have that condition.
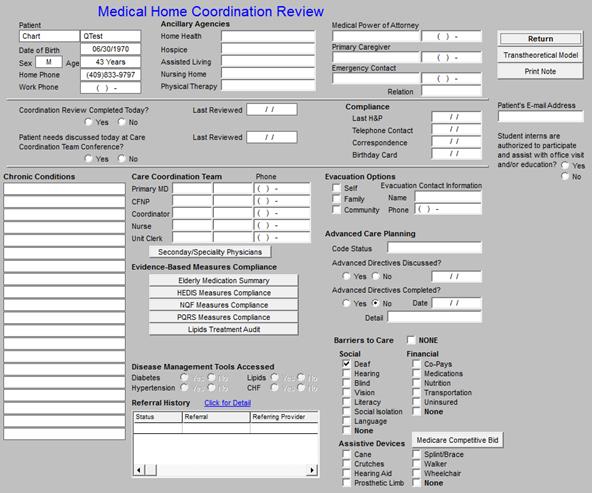
The Medical Home Coordination Review template is organized into three sections from top to bottom and into four columns left to right.
The first section from top to bottom has five lines in four columns and principally addresses demographic information about the patient. Each of the data points interact with all other elements of the EMR and are automatically filled when that information appears elsewhere in the EMR.
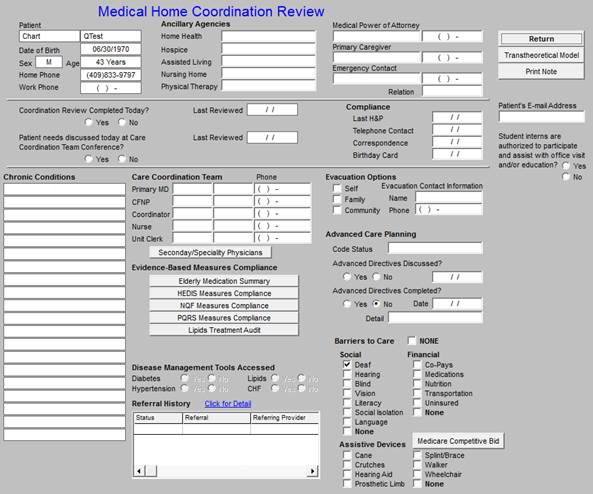
The first column addresses the patient’s personal information, which is automatically pulled from the EMR’s enterprise practice management system:
- Name
- Date of Birth
- Sex and Age
- Home phone
- Work phone
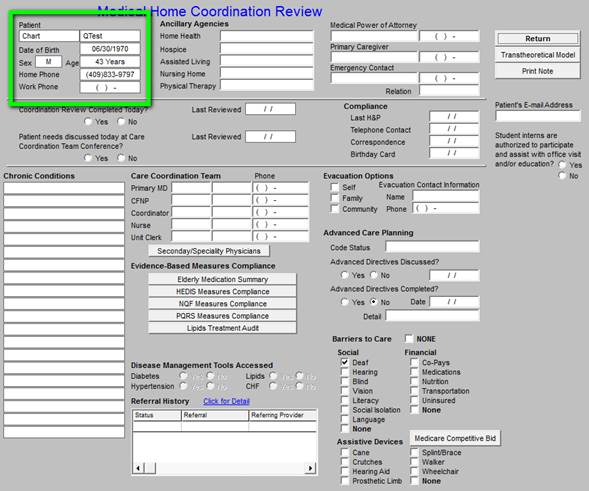
The second column is entitled Ancillary Agencies from which and/or through which the patient is receiving services. The second and third column information will be principally gathered by a form given to each patient for completion and then will be entered by our staff. Once the data is entered on our current patients - this task should take six to twelve months, we will easily maintain the collection of that information on new patients.
- Home Health
- Hospice
- Assisted Living
- Nursing Home
- Physical Therapy
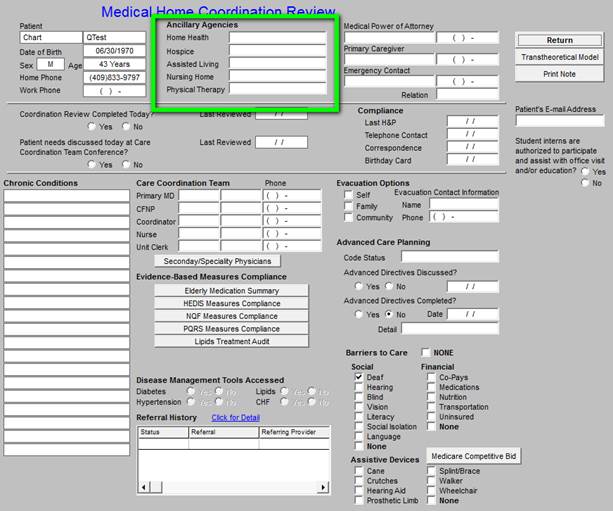
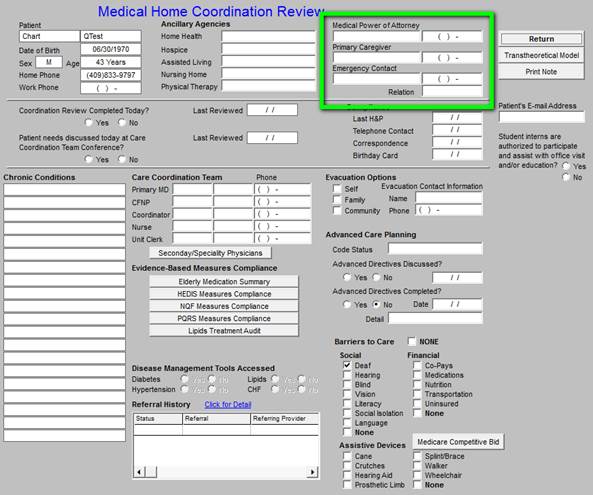
The Third column addresses:
- Medical Power of attorney and telephone number
- Primary Care Giver and telephone number
- Emergency Contact and telephone number
The fourth column contains three navigation buttons:
- The first is entitled RETURN takes you back to AAA Home
- The second launches he Transtheoretical Model Assessment template
- The Third is entitled Print note and it prints the Medical home Coordination
Review document which is to be given to the patient.
Clicking the Transtheoretical Model button launches the following pop-up.
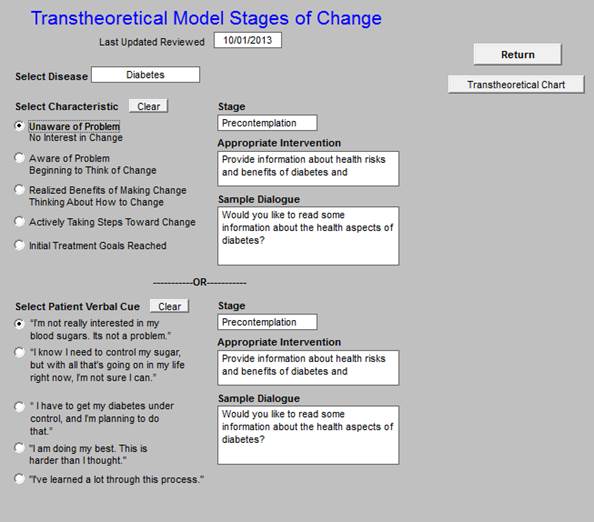
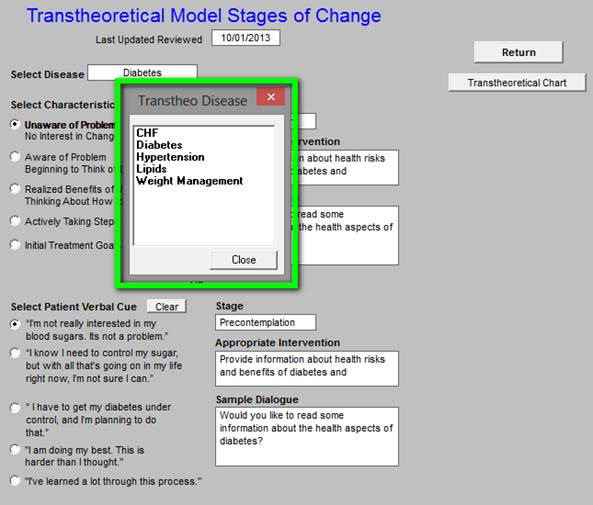
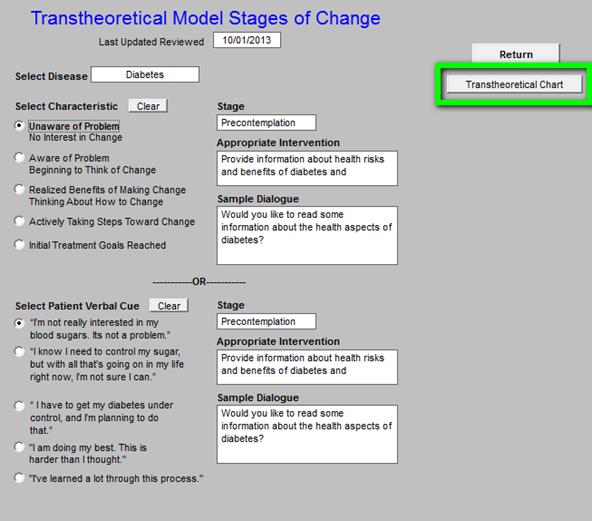
This tool allows you to assess and document, the patient’s current state of readiness to change their behavior. There are five, disease-specific options. Each option provides precise language for discussing with a patient their “readiness to change their behavior” of reach of the following conditions:
- CHF
- Diabetes
- Hypertension
- Lipids
- Weight Management
You access these disease-specific options by selecting them from the disease field.
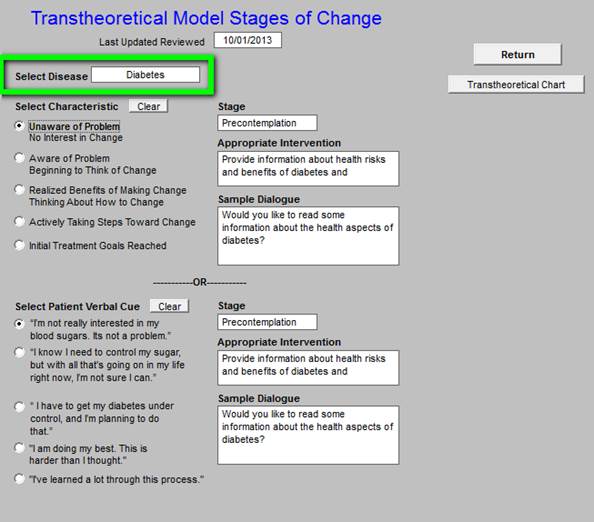
When you click in this field you will get a pop-up with the following options.
In that one of the goals of Medical Home is patient self-improvement and self-management, it is important to be aware whether the patient is ready to make a change in his/her health and to have a recommendation as to how to address the patient’s current state of readiness.
If a patient has not reached his/her goal in one of these conditions, or if the patient is not improving toward reaching that goal, the Transtheoretical-Model Assessment should be completed in order to assess where the patient is and what steps are required to encourage them to improve their health.
The results of this assessment will appear on the printed note which will be given to the patient and which will summarize the review of the Medical Home Coordination of Care. If more than one condition is assessed with this tool both will appear on the chart note.
Here is what the template would look like for a patient who has uncontrolled diabetes and who is not well motivated to change.
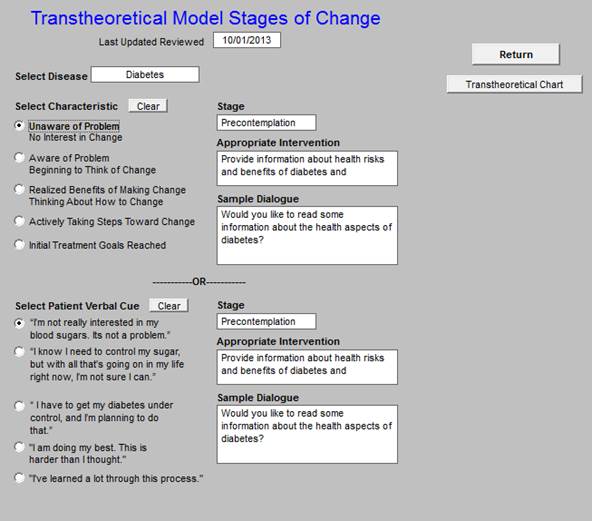
Under the heading “Select Characteristic”, there are five choices which will display the patient’s Stage of Change for the response they give. Depending upon which response a patient gives, one of the following stages will be displayed:
- Pre-contemplation
- Contemplation
- Preparation
- Action
- Maintenance
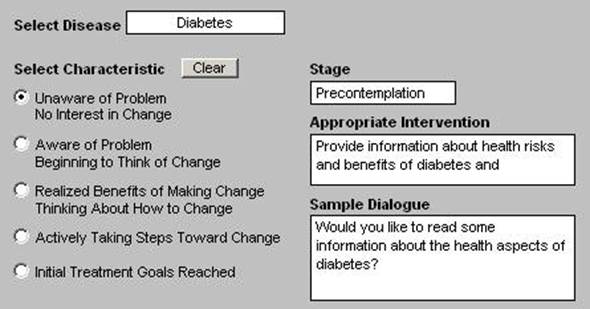
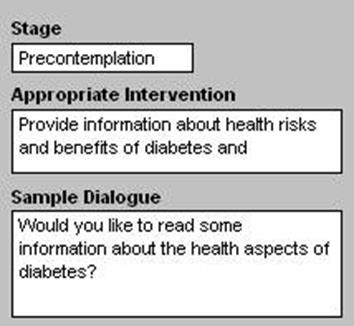
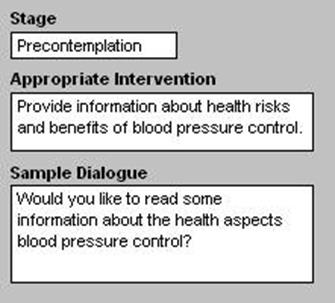
When a Stage of Change is selected, the following will be displayed:
- Stage of change
- Appropriate Intervention
- Sample dialogue
Under the heading “Select Patient Verbal cue” there are five choices which are linked to the patients Stage of Change. Once the Stage of Change is selected, the patient’s Verbal Cue should be noted.
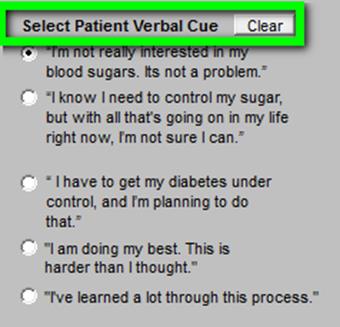
Depending upon the Patient’s “Verbal Cue” the following will appear:
- Stage of Change
- Appropriate Intervention
- Sample Dialogue
To the right of these boxes, there is a button entitled Transtheoretical Chart.
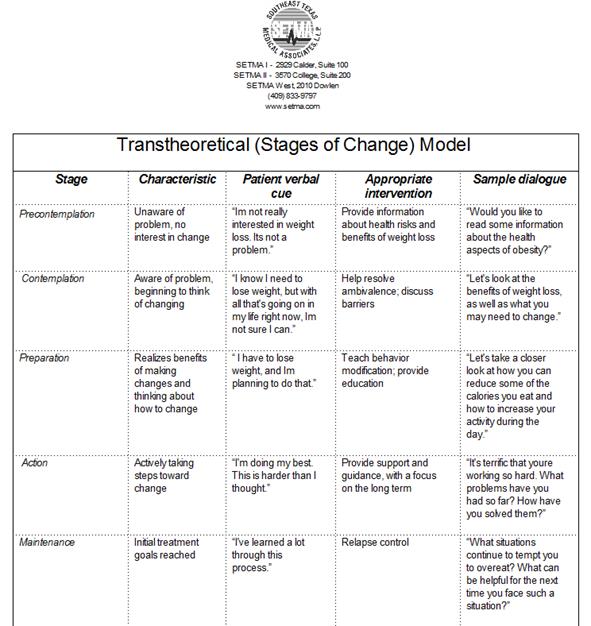
When activated the entire chart for the condition chosen will appear. For instance if you had chosen “weight management,” the following would appear.
If you wish to use this tool to assess more than one condition in a visit, simply select as many of the options you wish and ALL of them will appear on your Medical Home Coordination Review document.
When you are through with this tool, click, Return and it will take you back to the Medical Home Coordination Review template.
The button under the Transtheoretical Model Assessment is Print Note. Once the entire Medical Home Coordination Review has been completed, this button is launched in order to prepare a document which is given to the patient with the following instruction:
“This is a working tool. It is imperative that you review it for completeness, accuracy and usefulness to you. You should schedule a visit if any of your preventive health issues have not been completed and/or if there are issues raise with your review which require and explanation. You may choose to call your Nurse or Care Coordinator rather than scheduling a visit. The choice is yours.”
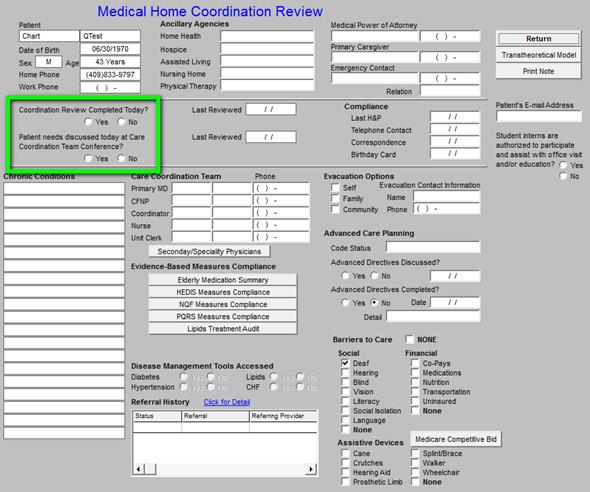
The second section of the Medical Home Coordination Review only has four columns.
The first column tracks two events:
- Whether or not the coordination of care review was completed today -- if you reviewed this function on the current visit, you should click box next to this function.
- Whether or not the patient’s care coordination needs were discussed at the team conference and if so what date and then the last time the team review was done is listed.
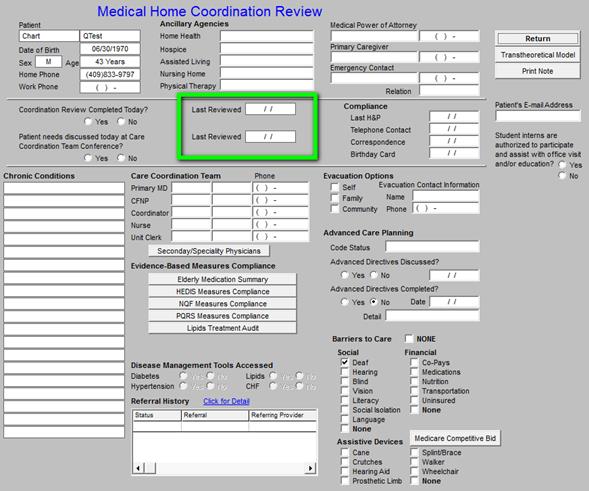
In the second column of the second section, the following is captured. This will automatically be noted by the system and requires no action on your part.
- The last date the coordination of care review was completed
- The last date that the patient’s coordination of care was discussed at team conference
The third column documents four events which are related to the Medical Home and is entitled Compliance. This compliance relates to specific functions of the Medical Home. These are care-coordination issues and relate to the standards SETMA has established for communications with the Medical-Home patient beyond the contact time in the office. The one exception is the Last H&P which is a clinic-contact issue.
- Last H&P - this will be captured automatically when you use the ICD-9 code V700 for Exam Well Adult, or V7231 for Exam GYN Gynecological Routine. It is important to use one of these codes as this is one HEDIS measure which requires that it be reported by the health plan through encounter data and not through a chart review or a report by the provider that they have done the examination.
- Telephone contact -- two times per year, the practice will contact the patient about their healthcare needs and/or about preventive care needs.
- Correspondence - two times a year, the practice will contact the patient with education materials and/or with needed preventive care needs.
- Birthday Card - each year, the practice will contact the patient via correspondence on his/her birth date both to acknowledge their birthday and to encourage them with needed preventive care measures.
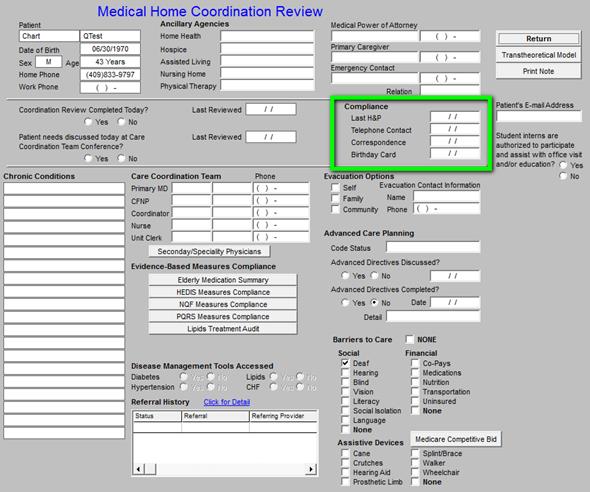
It is the intent of SETMA’s Medical Home to contact the patient four times a year, other than at times the patient has an appointment, or comes to clinic. The contracts will be twice by correspondence and twice more by telephone calls. One of written correspondences will be a Medical-Home-birthday card which will acknowledge the patient’s special day and include preventive health reminders to the patient and to their personal physician.
The fourth column has the patient’s e-mail address
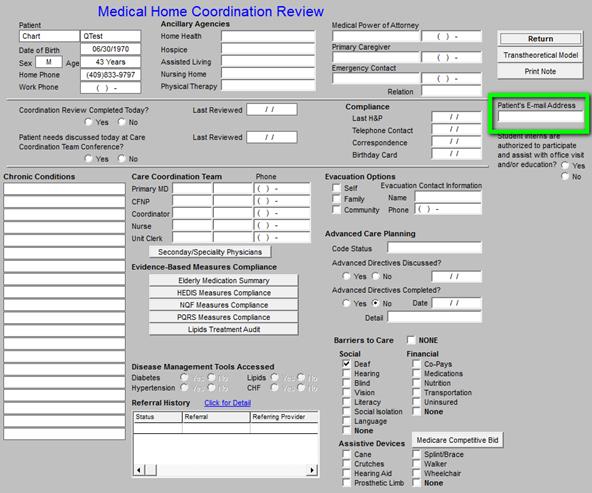
This is neither a secure nor an encrypted contact and cannot be used for communications with a patient of a confidential nature. For that capability, see the section on NextGen’s web portal entitled NextMD.
The third section of the Medical Home Coordination Review has three columns.
The first column is a list of the patient’s chronic conditions. This is essentially a Patient Problem List. While it is not displayed on the Medical Home Coordination Review, the patient’s active medication list and medication allergies will appear on the Medical Home Coordination Review documentwhich will be given to the patient each time it is reviewed.
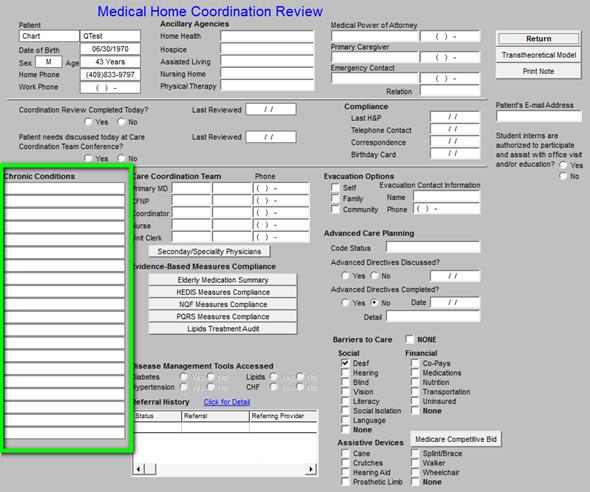
This provides the reviewer and/or physician a reminder of a patient’s special and specific needs which should be considered in the Coordination of Care review.
The second column in the third section includes six elements
- Care Coordination Team
- Physician
- CFNP
- Care Coordinator
- Nurse
- Unit Clerk
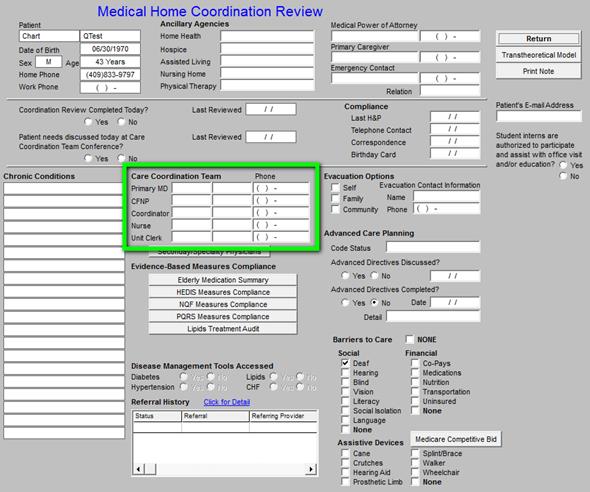
The next element is a button entitled Secondary/Specialist Physicians.
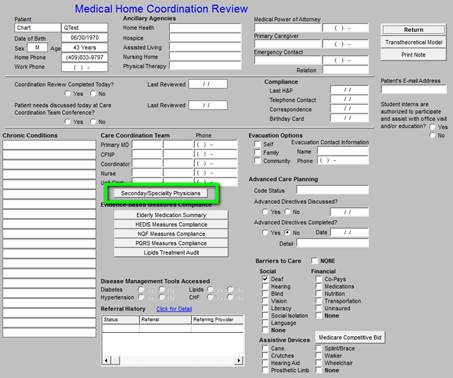
This button will launch the following template.
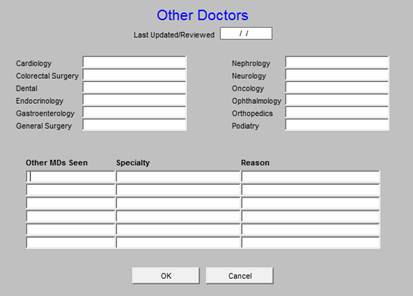
Because Medical-Home implies a Medical Home Neighborhood, it is important to know who other care gives are who participate in the care of this patient. As SETMA deploys NextGen’s Community Health Solutions (interface engine, repository, physician portal), there will be a more seamless connectivity with the larger neighborhood. It will be the intent of SETMA’s Medical Home to include each of the patient’s specialist-care givers in the Community Health Solutions.
The next section is entitled Evidenced-based Measures Compliance and has six buttons**
- The Elderly Medication Summary
- The HEDIS Measures
- The NQF Measures
- The PQRS Measures
- The PCPPI Diabetes*
- The PCPPI Hypertension*
*(Physician Consortium for Physician Performance Improvement Data Sets) for:
**Remember, as previously noted, buttons 5 and 6 will ONLY appear in the records of patients with those diagnoses. If the patient has neither diabetes nor hypertension only four buttons will appear.
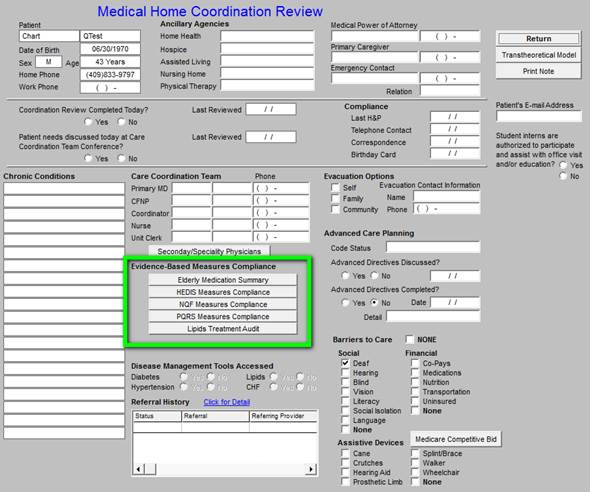
These functions will be discussed below.
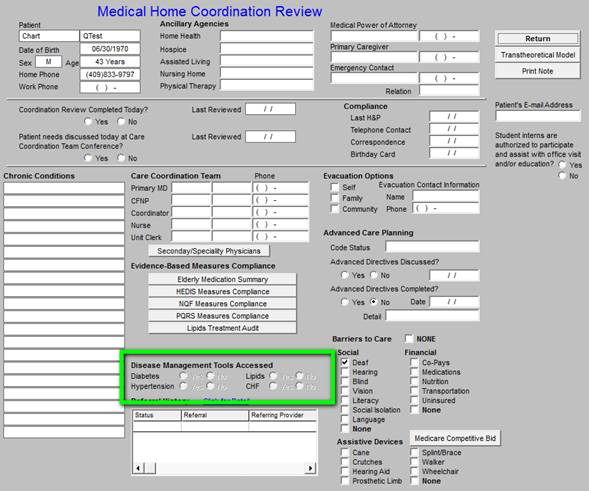
The next element is Disease management Tools Accessed.
- Diabetes
- Hypertension
- Lipids
- CHF

From AAA Home, when a specific disease-management tool is:
- accessed and completed on any of these four conditions, and
- when the follow-up document is printed and given to the patient,
the radial button next to that condition will be highlighted on the Medical Home Coordination Review template.
Note: Because these radial buttons cannot be changed from the template and because they are in demographic fields which means they come forward at each visit, the highlighting is faded.
The last element in this column is the Referral History. The most recent referrals are displayed in this window.
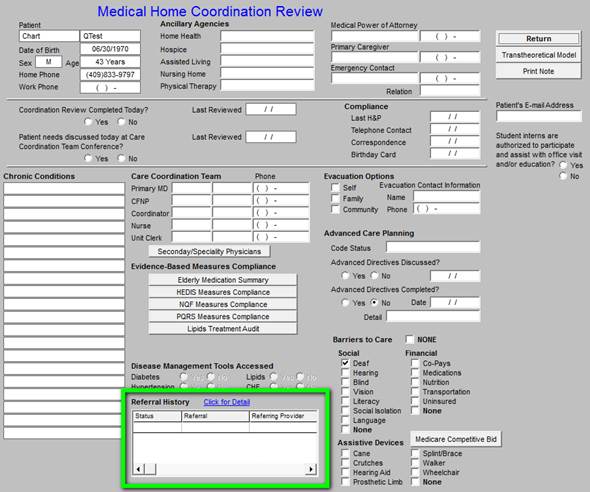
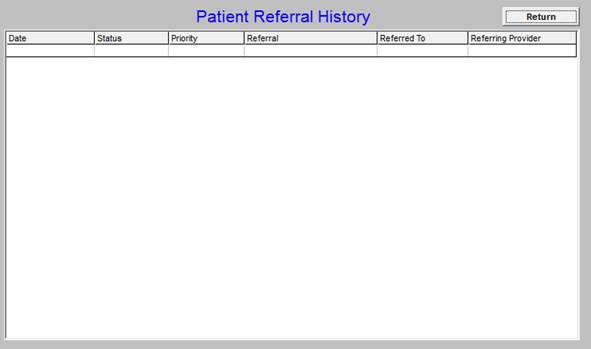
There is a button entitled Click for Detail beside the title Referral History which launches the following:
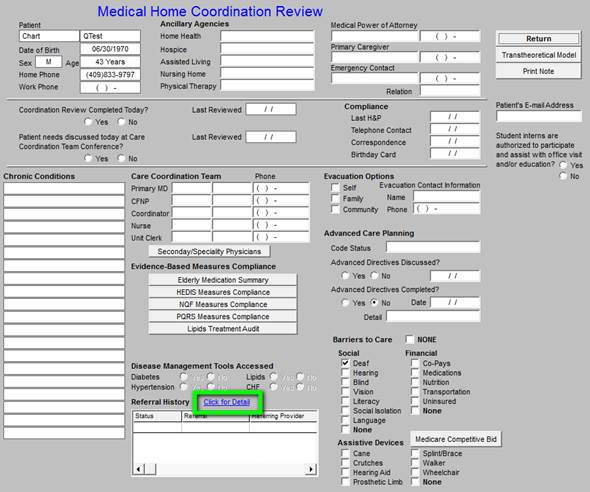
This will launch a list of all of the referrals which this patient has ever been given and will show their status. To make certain that no referral is not completed and/or no patient does not follow through, IT will run a query and will let SETMA operations know of patients whose referrals have either not been completed by our department or where we do not have a report from the referral source.
The third column in this third section of the Medical Home Coordination Review template has the following elements:
- Evacuation Options
- Advanced Care Planning
- Barriers to Care
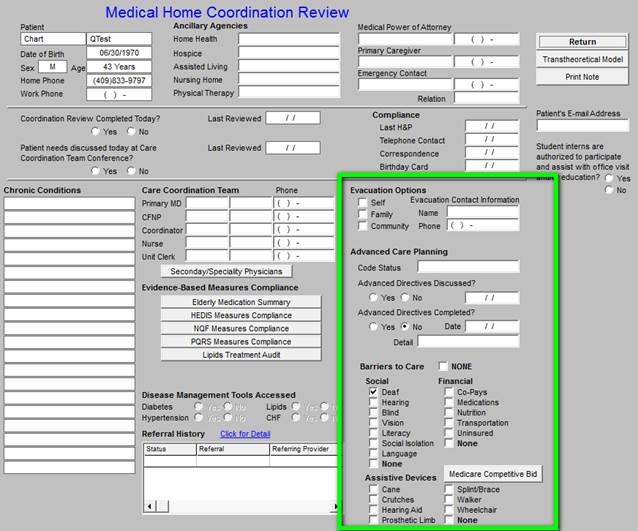
Each of the specific issues documented here are linked to other data points in the EMR where the same information is captured. This avoids redundancy in data entry and leverages the power of the EMR.
Evacuation Options allows the Medical Home to know who needs special help in the case of a mandatory evacuation being called by the local authorities. This function identifies who will be responsible for the patient’s evacuation:
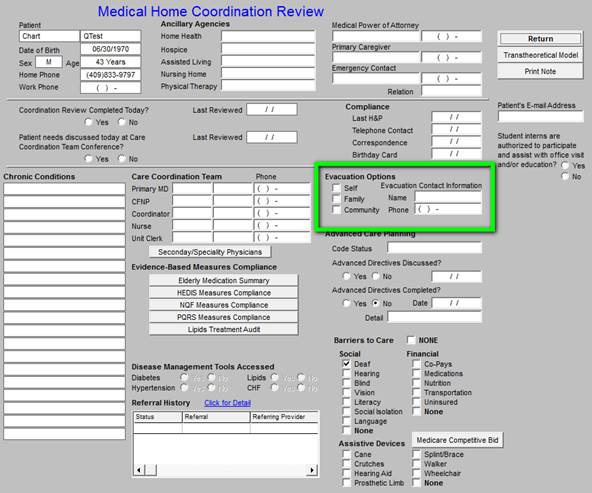
This function also provides a place to document the name and phone number of the family member or community agency which should be contacted to provide evacuation for this patient.
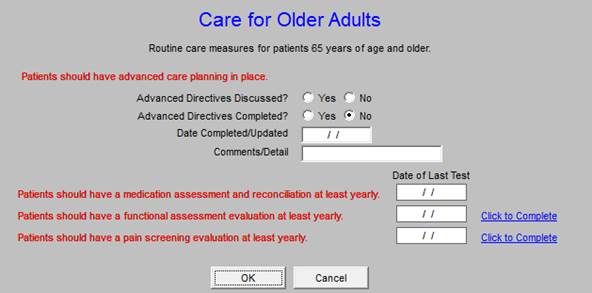
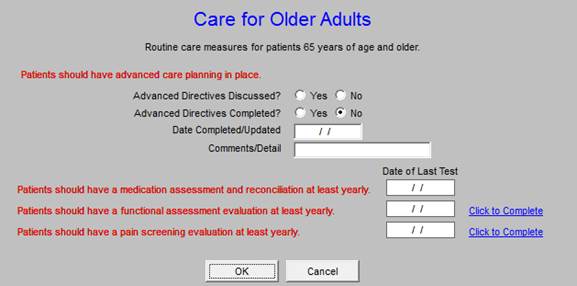
Advanced Care Planning is a HEDIS and a Medical Home requirement for older adults and it is a requirement of Medical Home. This function allows for the documentation of the patient’s:
- Code status
- Whether Advanced Directive was discussed at the present encounter*
- Whether the patient has an Advanced Directive
- Advanced Care Directive - details
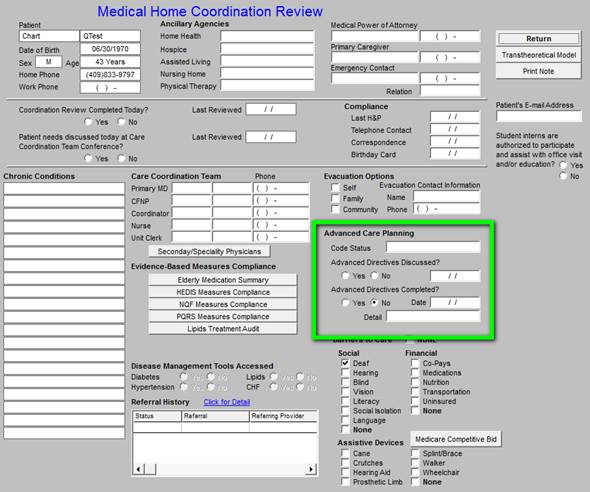
Whether Advanced Directive was discussed- one of the HEDIS measures for “care for older adults” requires that the advanced directive be on file, or that it be discussed at the current encounter. When you click the check box next to this function on the Medical Home Coordination Review template, it will automatically result in your receiving credit for this function.
If you check the box next to “Advanced Directive was discussed” or that “Whether the patient has an Advanced Directive”, the following HEDIS Measure (see below) will be credited for this patient’s Care for Older Adults record.
The Barriers to Care section of the Medical Home Coordination Review template allows for the aggregation of data which is collected elsewhere. Three categories of barriers are reviewed:
- Social
- Financial
- Assistive Devices
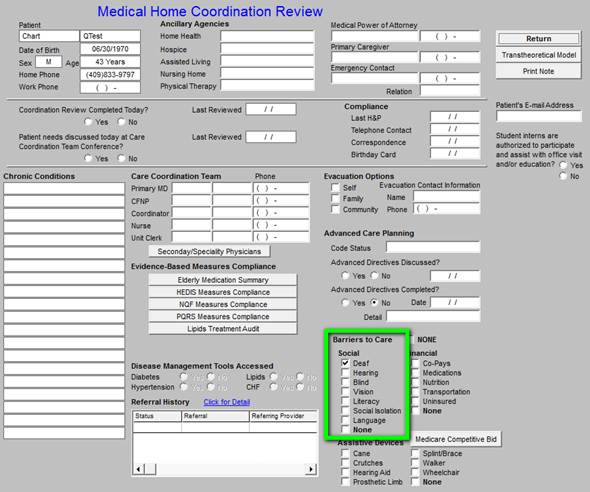
The Social Barriers of special interest to the Medical-Home-Coordination team are:
- Hearing
- Vision
- Literacy
- Social Isolation
- Language Preferred Language
Each of these data points is already collected in the EMR under Patient Alerts.
Financial Barriers identifies issues in the patient’s care which prevents them from obtaining care due to financial limitations including their inability to pay for:
- Co-pays
- Medications
- Nutrition
- Transportation
- Uninsured
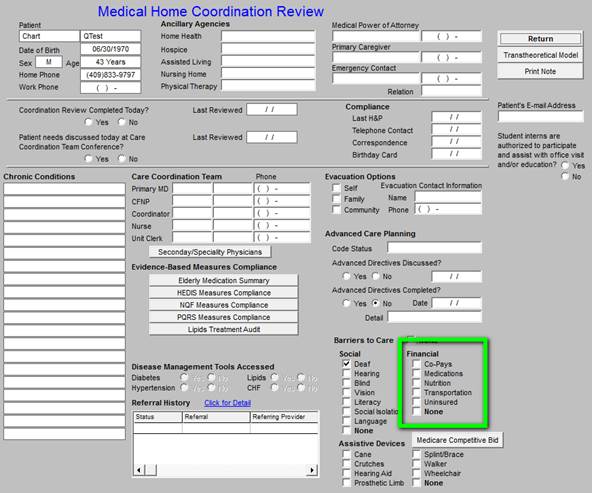
While SETMA’s resources are limited, The SETMA Foundation has been established to assist in the obtaining of care by our patients who need financial help in obtaining care.
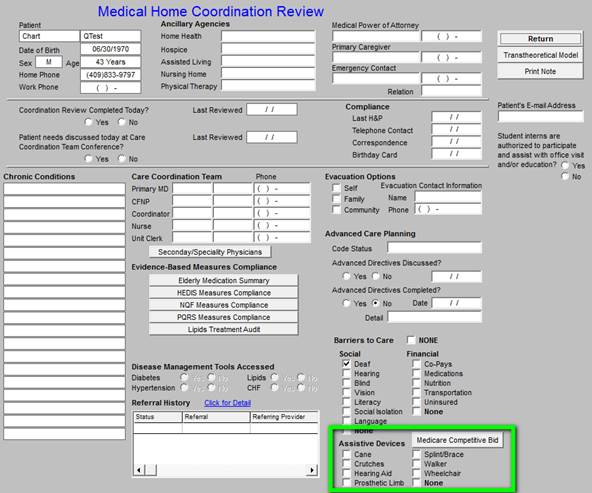
The final Barriers-to-Care is Assistive Devices. This is a list of devices which may be used by our patients, including:
- Cane
- Crutches
- Hearing Aid
- Prosthetic Limbs
- Spine/Brace
- Walker
- Wheelchair
The Medical Home Coordination Review will identify the use of these devices as they will affect the patients assess to care and often will limit the kinds of care which can be prescribed for the patient in regard to therapy and exercise.
Evidenced-Based Measures for Quality of Care
The Following is the full detail of using the six categories which appear under the heading Evidenced-based Measures Compliance, in the second column of the Medical Home Coordination Review where there are 6 buttons:
- The Elderly Medication Summary
- The HEDIS Measures
- The NQF Measures
- The PQRS Measures
- The PCPI Diabetes Data Set*
- The PCPI Hypertension Data Set*
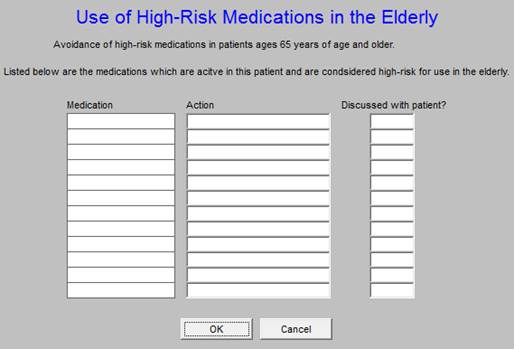
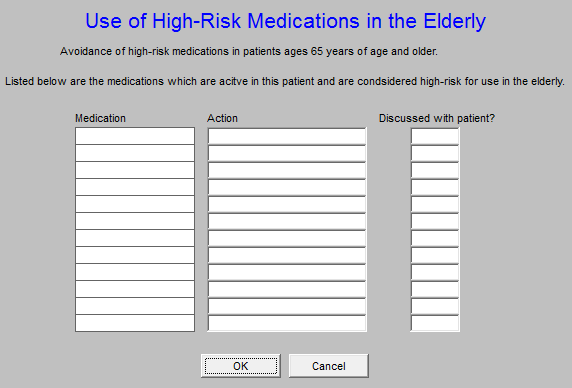
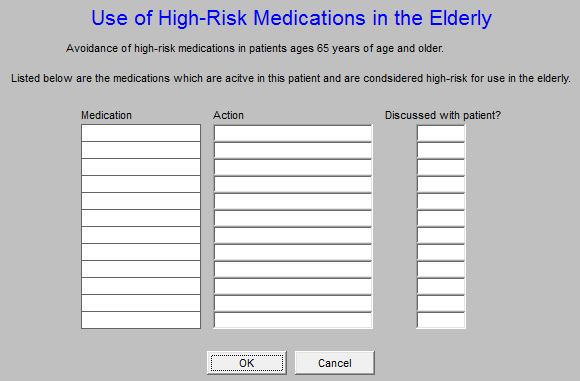
The First button is the Elderly Medication Summary
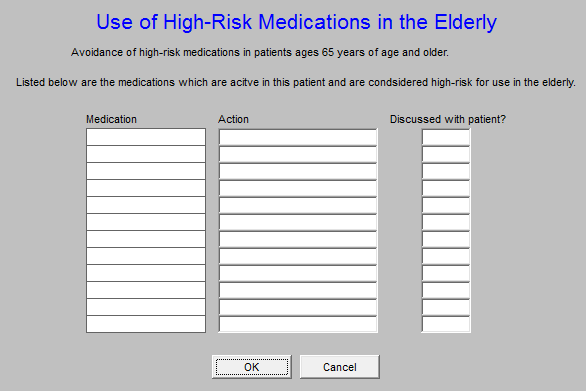
This aggregates the material which is gathered automatically on the HEDIS Measures templates where there are six categories of medications which are potentially hazardous in older adults:
- High Risk Medications
- Medications which are contraindicated in the following conditions in older adults
- Arthritis
- COPD
- Dementia
- Depression
- Insomnia
When a medication is found which falls into these categories the name of that medication will appear in the appropriate list. The Alert under the Medical Home Coordination button on AAA entitled “ needs attention,” alerts that provider that this needs attention.
In the two columns beside the medication listed, the provider can document the action taken. When the provider clicks in the space entitled “action,” the options on the pop-up are:
- Medication changed
- Medication stopped
- Reviewed, must be continued
When this is done, in the space entitled, “Discussed with patient?,” the provider can designate whether this action was discussed with the patient with a “yes” or “no.”
The second button is HEDIS Measures Compliance
What is HEDIS? -- Healthcare Effectiveness Data and Information Set published by he National Committee on Quality Assurance (NCQA) HEDIS measures are used by more than 90% of United States health plans to measure the effectiveness of care provided through their plans. HEDIS measures effectiveness of preventive care, acute care and chronic care based on the results of evident-based studies.
When this button I launched it displays the HEDIS Measures Compliance template which is entitled, “2009 HEDIS Technical Specifications for Physician Measurement.”
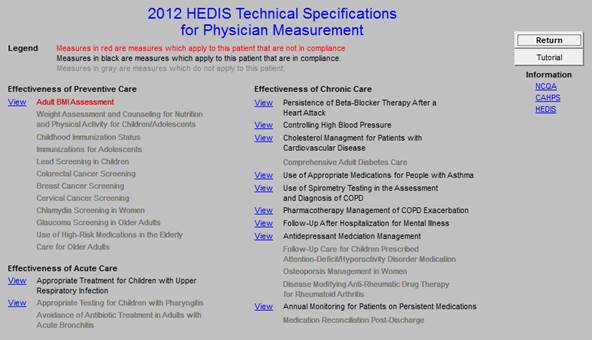
This template lists all of the HEDIS measures for which providers are responsible. All of the activity and fulfillment of the HEDIS measures on this template are captured automatically.
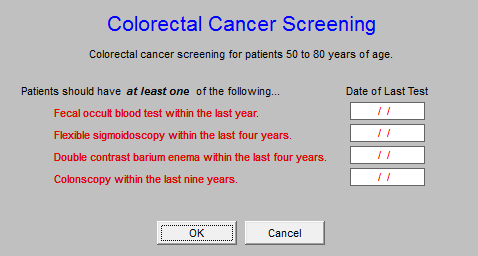
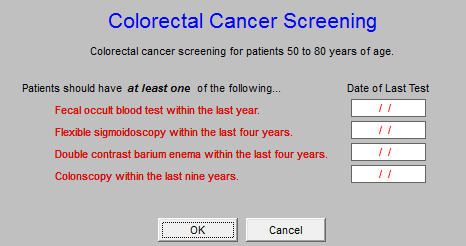
In the course of the patient encounter, the provider will access this and other evidenced-based quality measures. Those which appear in red will be reviewed and the action required to fulfill that measure will be taken, i.e., if the colorectal screening shows up in red, the provider will order a stool for occult blood, a colonoscopy, a double contrast barium enema or a flexible sigmoidoscopy. When the results of the study, or procedure is returned, the measure will be marked as met.
To the right of the HEDIS measures are the following buttons:
- Return - this takes you back to the AAA Home screen
- Tutorial - this makes it possible for you to review the content of all of the HEDIS measures whether or not they apply to the current patient or not. To revert back to the display of only those HEDIS measures which apply to the current patient, simply exit the template and then return.
- There are three Help buttons which display:
- NCQA - this gives information about the National Committee on Quality Assurance.
- CAHPS - this gives information about the Consumer Assessment of Healthcare Providers and Systems (CAHPS) program.
- HEDIS - this gives information about the Healthcare Effectiveness Data and Information Set.
At the top of the template is a section entitled, “LEGEND,” which explains that:
*The measures which apply to the current patient and are not fulfilled appear in RED. The measures which apply to the current patient and are fulfilled appear in BLACK. The measures which do not apply to the current patient are grayed out.
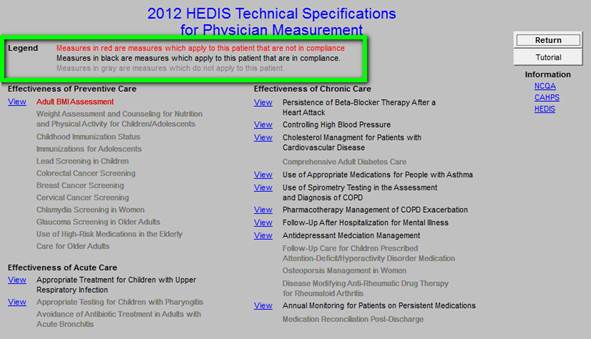
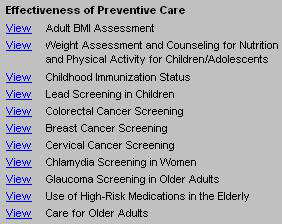
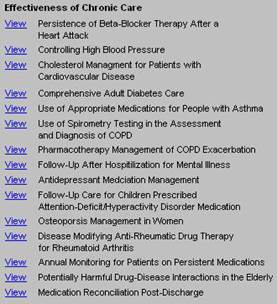
Below this explanation is listed the three categories of HEDIS measures
- Effectiveness of Preventive Care where there are 10 measures
- Effectiveness Acute Care where there are 5 measures

- Effectiveness of Chronic Care where there are 13 measures
Screen shots of each of these 28 measures will now be displayed with:
- The name of the measure listed first
- Followed by a screen shot of the pop-up which defines the content of the measure launched. The content will typically define:
- The age ranges to which the measure applies
- The metric which the measure addresses, i.e., the blood pressure, LDL, etc.
*Remember, for any particular patient ONLY those HEDIS measures which apply to a particular patient will be in redor black according to the LEGEND above.
1. Effectiveness of Preventive Care
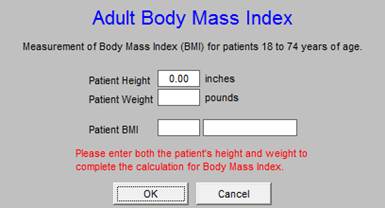
Adult BMI Assessment
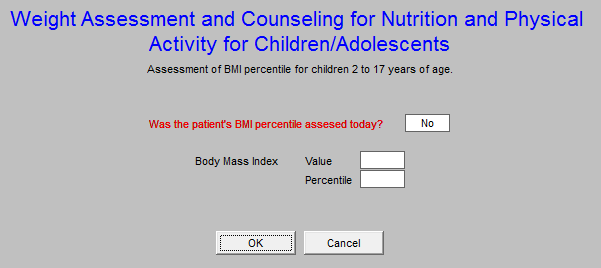
Weight Assessment and Counseling for Nutrition and Physical Activity for Children / Adolescents
Childhood Immunization Status
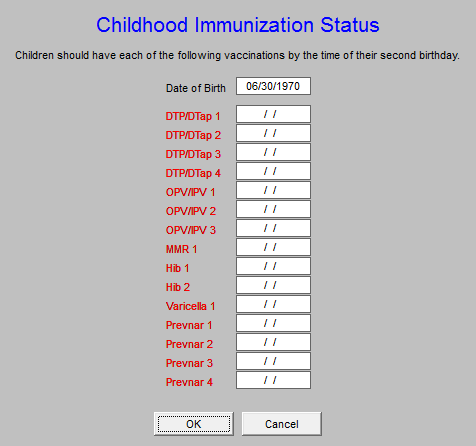
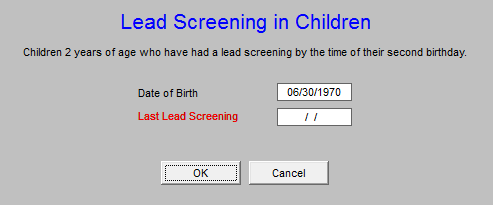
Lead Screening in Children
Colorectal Cancer Screening
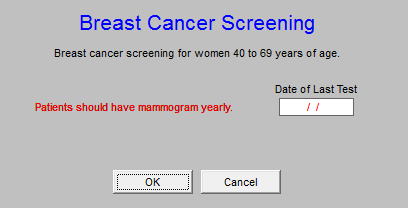
Breast Cancer Screening
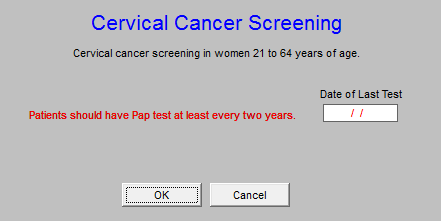
Cervical Cancer Screening
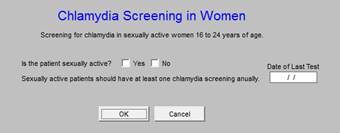
Chlamydia Screening in Women
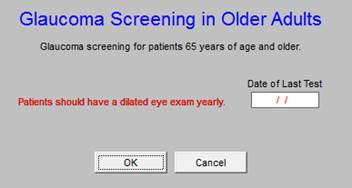
Glaucoma Screening in Older Adults
Use of High-Risk Medications in the Elderly
Care for Older Adults
2. Effectiveness of Acute Care
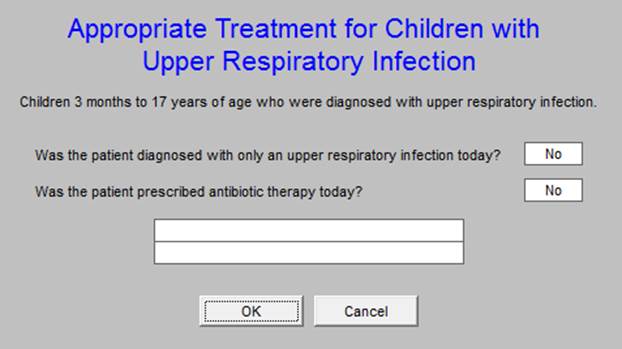
Appropriate Treatment for Children with Upper Respiratory Infection
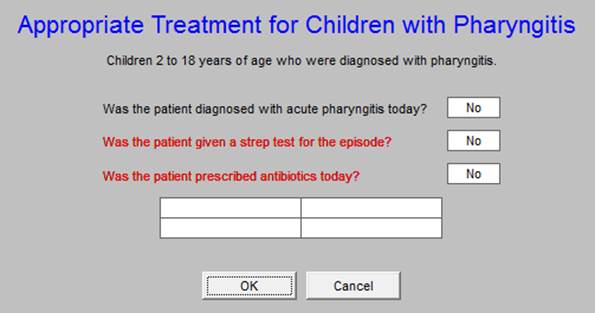
Appropriate Testing for Children with Pharyngitis
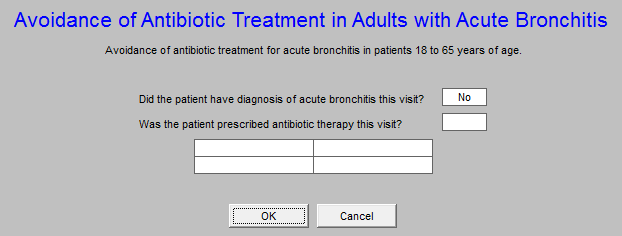
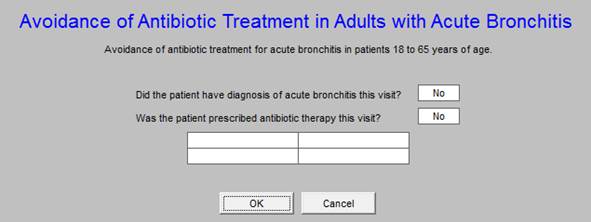
Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis
3. Effectiveness of Chronic Care
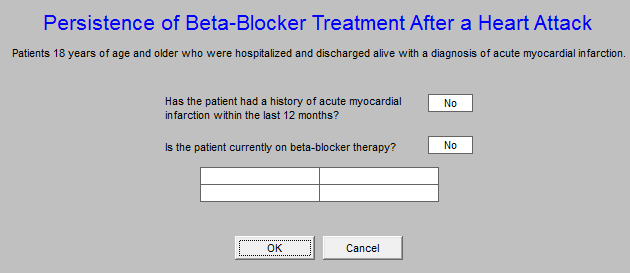
Persistence of Beta-Blocker Treatment After a Heart Attack
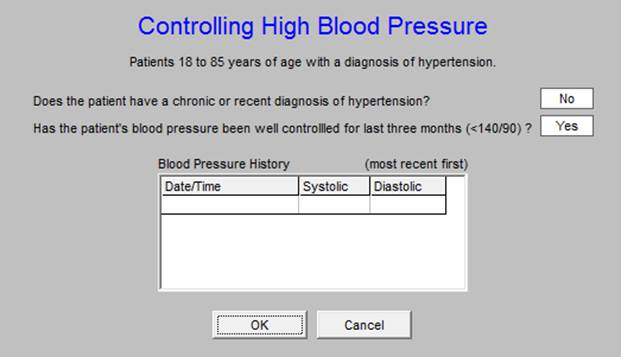
Controlling High Blood Pressure
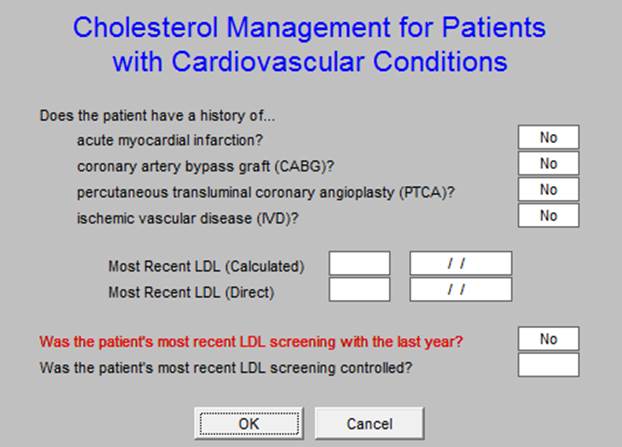
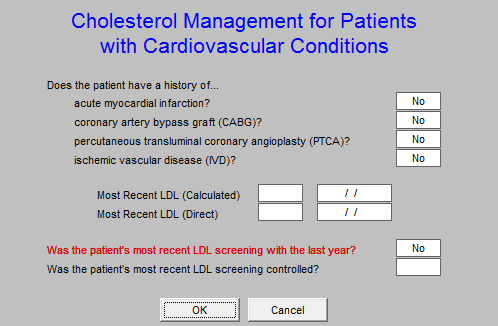
Cholesterol Management for Patients with Cardiovascular Disease
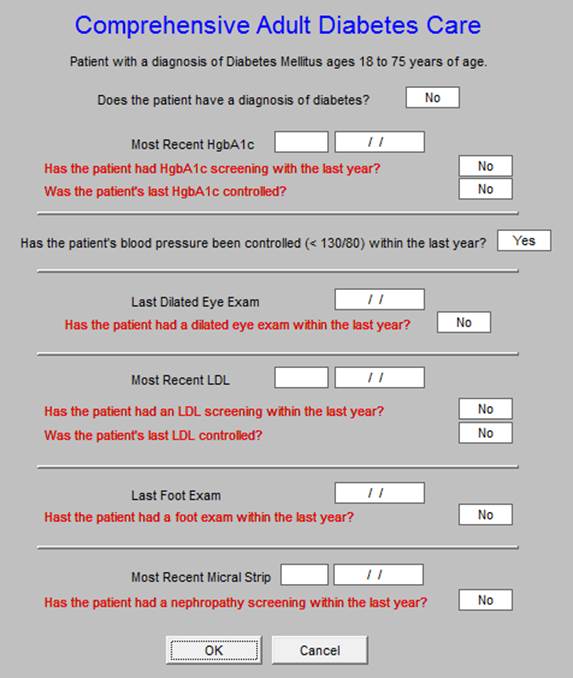
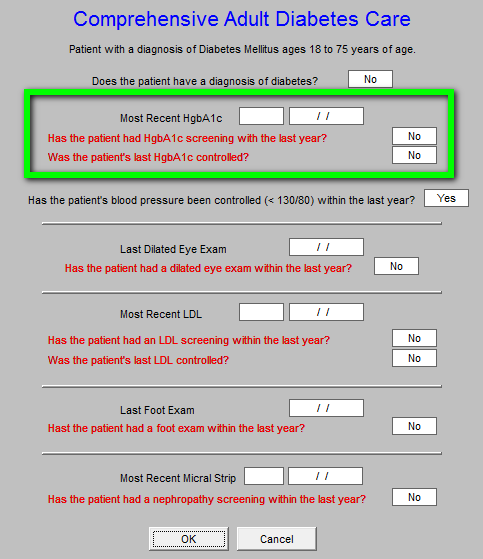
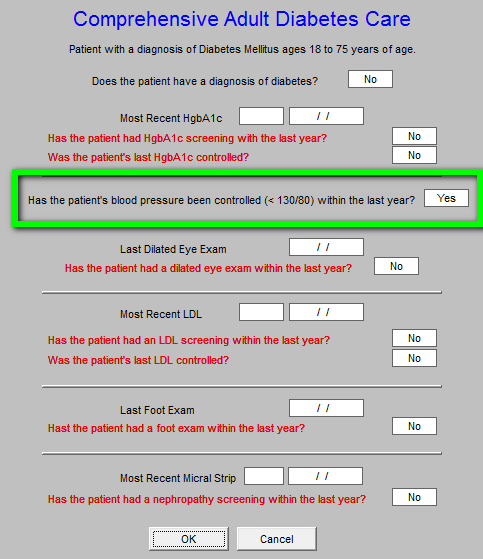
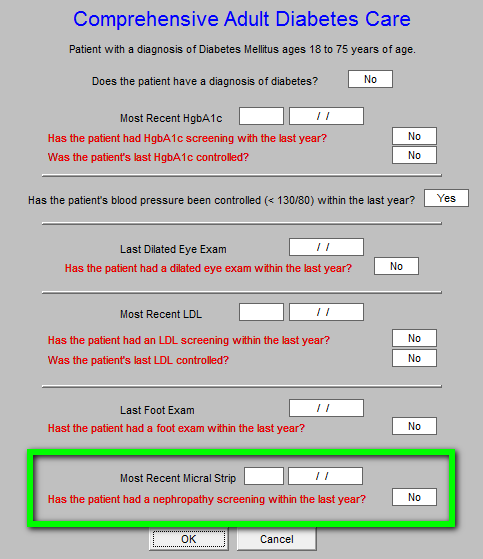
Comprehensive Adult Diabetes Care
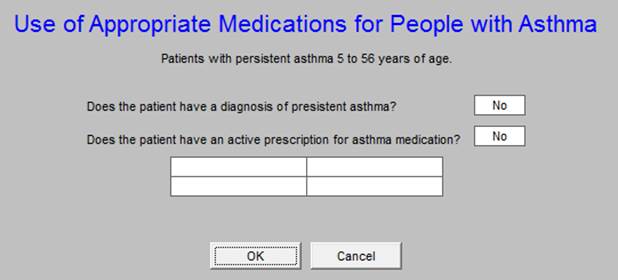
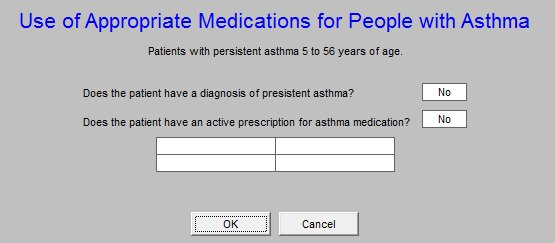
Use of Appropriate Medications for People with Asthma
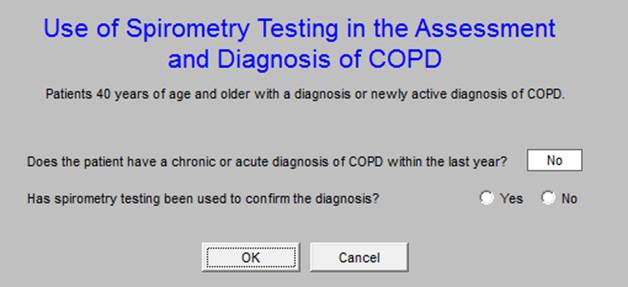
Use of Spirometry Testing in the Assessment and Diagnosis of COPD
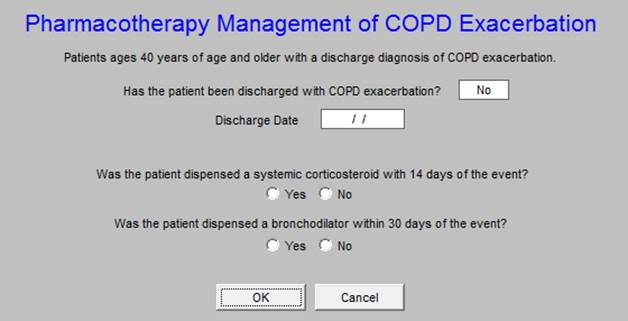
Pharmacotherapy Management of COPD Exacerbation
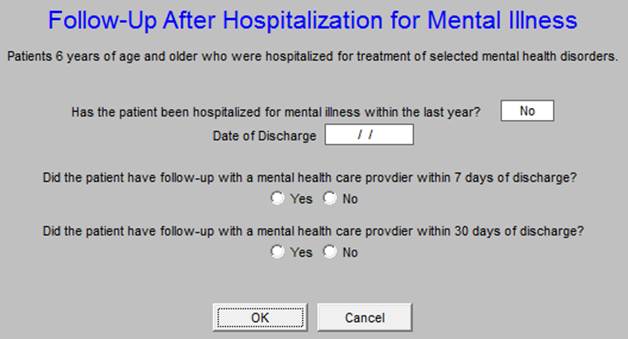
Follow-Up After Hospitalization for Mental Illness
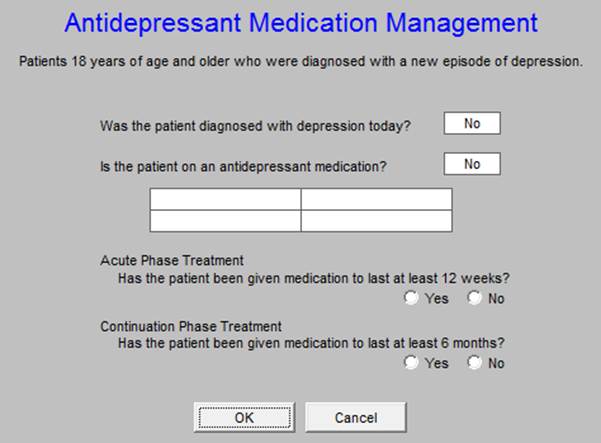
Antidepressant Medication Management
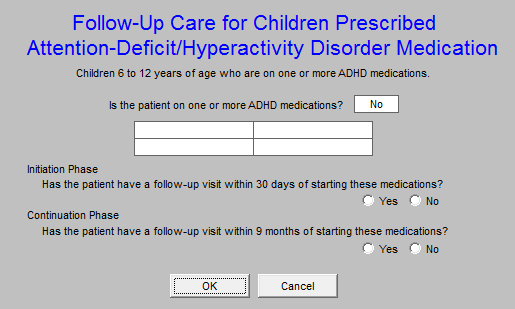
Follow-up Care for Children Prescribed Attention Deficit/Hyperactivity Disorder Medication
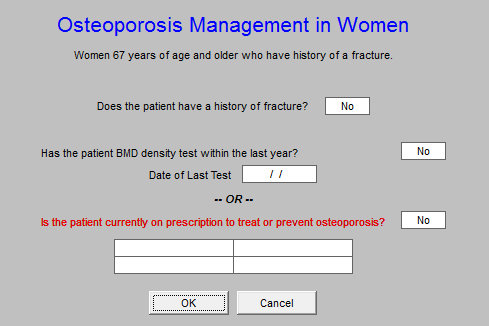
Osteoporosis Management in Women
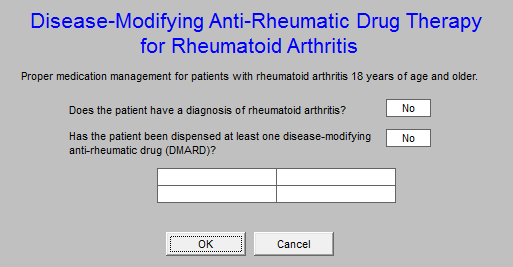
Disease Modifying Anti-Rheumatic Drug Therapy for Rheumatoid Arthritis
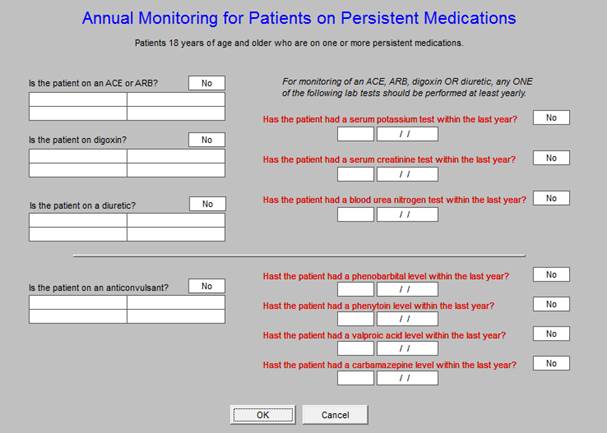
Annual Monitoring for Patients on Persistent Medications
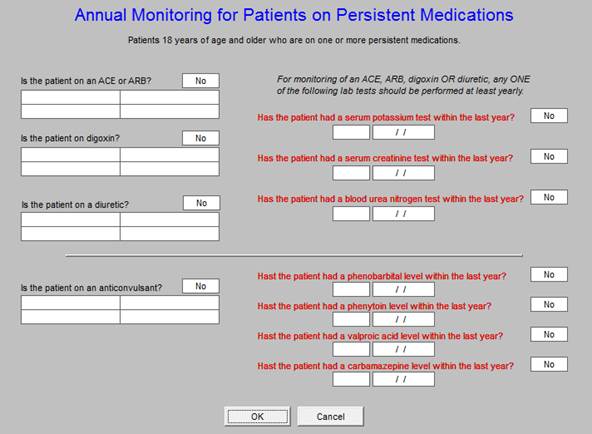
Potentially Harmful Drug-Disease Interactions in the Elderly
The use of this template and its function is explained above. This is the only HEDIS measure which is presented twice - here and as a separate evidenced-based measure on the Medical Home Coordination Review template. See Above
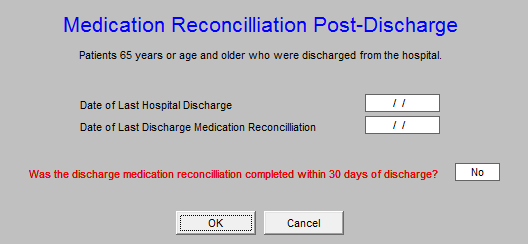
Medication Reconciliation Post-Discharge
National Quality Forum (NQF) The next button is entitled NQF Compliance.
National Quality Forum (NQF) - In 1998, A report of the President's Advisory Commission on Consumer Protection and Quality in the Health Care Industry, proposed the formation of the Forum as a part of a national agenda for improvement in healthcare delivery. Formed in 1999, NQF’s mission statement declared, “The mission of the National Quality Forum is to improve the quality of American healthcare by setting national priorities and goals for performance improvement, endorsing national consensus standards for measuring and publicly reporting on performance, and promoting the attainment of national goals through education and outreach programs.”
NQF’s vision is that “the NQF will be the convener of key public and private sector leaders to establish national priorities and goals to achieve the Institute of Medicine Aims - health care that is safe, effective, patient-centered, timely, efficient and equitable. NQF-endorsed standards will be the primary standards used to measure and report on the quality and efficiency of healthcare in the United States. The NQF will be recognized as a major driving force for and facilitator of continuous quality improvement of American healthcare quality.” To achieve NCQA recognition as a Medical Home, SETMA must report on 10 measures endorsed by NQF. We have chosen to report on 43 for 2009.
This will launch the below template.

There are 7 categories of NQF-endorsed, evidenced-based measures which SETMA has chosen to report on for our NCQA recognition. The measures will be reviewed by category and by each individual measures.
General Health Measures
Body Mass Index Measurement
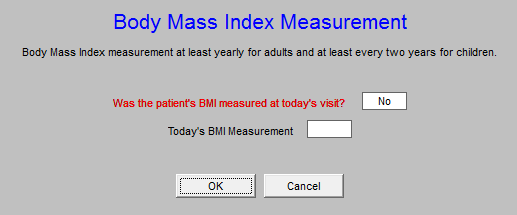
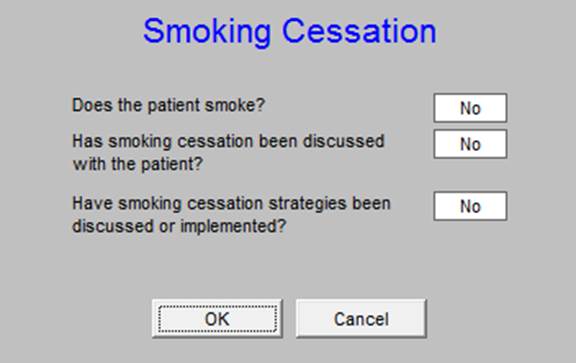
Smoking Cessation
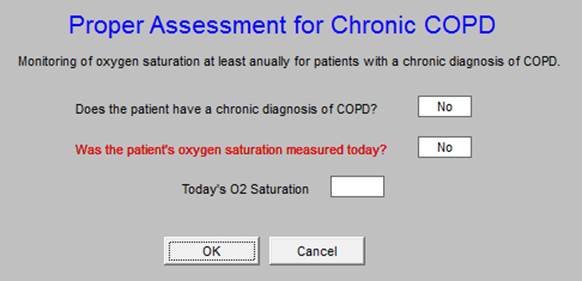
Proper Assessment for Chronic COPD
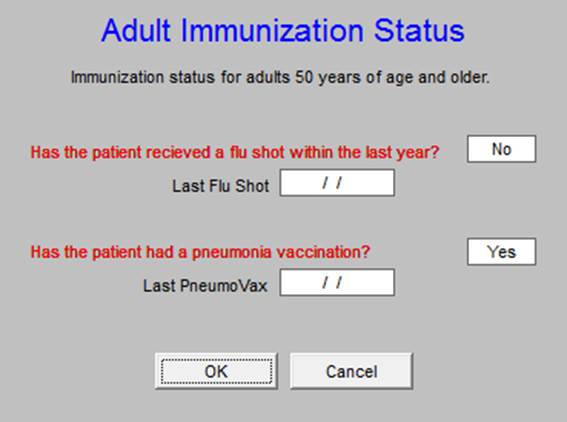
Adult Immunization Status
Blood Pressure Measures
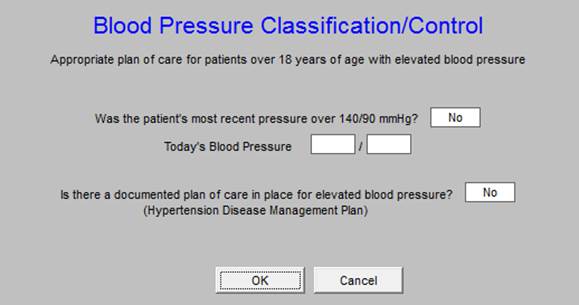
Blood Pressure Measurement
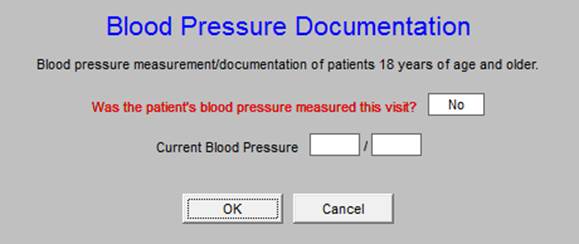
Blood Pressure Classification Control
Medication Measures
Current Medication List
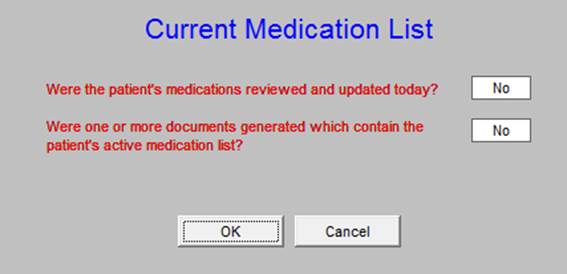
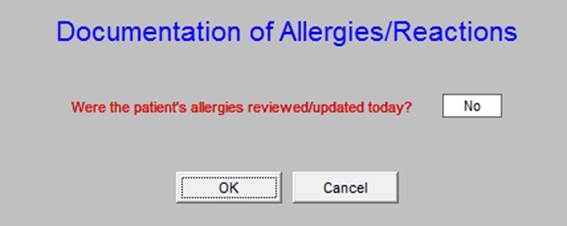
Documentation of Allergies/Reactions
Therapeutic Monitoring of Long Term Medications
Drugs to Avoid in the Elderly
Appropriate Medications for Asthma
Inappropriate Antibiotic Treatment for Adults with Acute Bronchitis
LDL Drug Therapy for Patients with CAD
Care for Older Adults
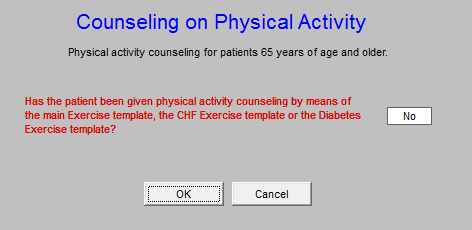
Counseling on Physical Activity
Colorectal Cancer Screening
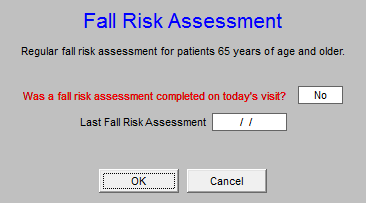
Fall Risk Management
Diabetes Measures
Dilated Eye Exam
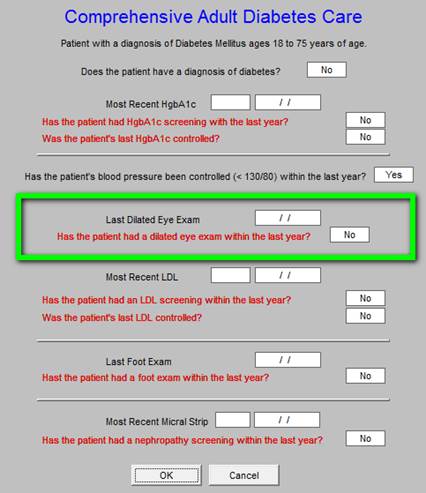
Foot Exam
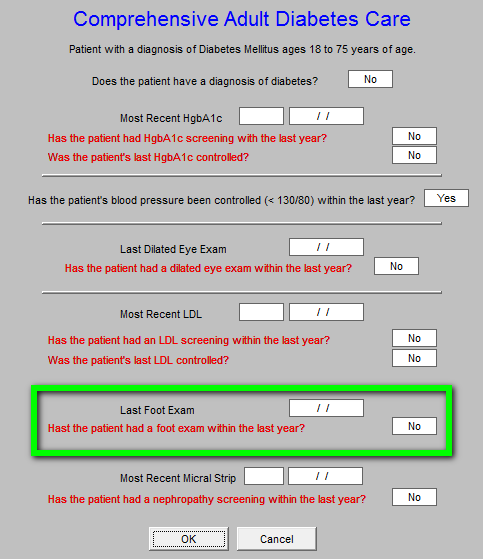
Hemoglobin A1c Testing Control
Blood Pressure
Lipid Screening
Physician Quality Reporting System (PQRS)
The 2006 Tax Relief and Health Care Act required the establishment of a physician quality reporting system, including an incentive payment for eligible professionals (EPs) who satisfactorily report data on quality measures for covered services furnished to Medicare beneficiaries during the second half of 2007 (the 2007 reporting period). CMS named this program the Physician Quality Reporting System (PQRS). The 2009 PQRI Measures Specifications Manual for Claims and Registry Release Notes is a 442-page document which explains this program.
PQRI has identified 134 measures and requires that a practice report to report on at least 3 individual measures, or 1 Measures Group in order to be recognized by CMS. SETMA will report on three Measures Groups (Diabetes, Preventive Care, and Rheumatology, and the measures on Ophthalmology) which contain a total of 28 measures instead of the required 3. The program has been changed to PQRS.
The next button is entitled PQRS Compliance - those elements are described elsewhere.
Physician Consortium for Physician Performance Improvement Data Sets (PCPPI)
The Physician Consortium for Performance Improvement
The Physician Consortium for Physician Performance Improvement (Consortium) is a group of clinical and methodological experts convened by the AMA. The Consortium includes representatives from more than 60 national medical specialty and state medical societies, the Agency for Healthcare Research and Quality, and the Centers for Medicare and Medicaid Services.
The Consortium's vision is to fulfill the responsibility of physicians to patient care, public health, and safety by:
- becoming the leading source organization for evidence-based clinical performance measures and outcomes reporting tools for physicians; and
- ensuring that all components of the medical profession have a leadership role in all national forums seeking to evaluate the quality of patient care.
The Consortium's mission is to improve patient health and safety by:
- Identifying and developing evidence-based clinical performance measures that enhance quality of patient care and that foster accountability;
- Promoting the implementation of effective and relevant clinical performance improvement activities; and
- Advancing the science of clinical performance measurement and improvement.
The Consortium works to develop evidence-based clinical performance measures and clinical outcomes reporting tools to support physicians in quality improvement efforts.
The Consortium has published a number of disease management data sets which established quality of care measures with which physicians and other healthcare providers can measure their own performance.
Physician Consortium for Performance Improvement - this measurement set for various conditions such as hypertension, diabetes, congestive heart failure and others have been developed by the American Medical Association (AMA), the Centers for Medicare and Medicaid Services (CMS), the Institute of Medicine (IOM) and the medical and surgical specialty societies. These data sets are intended as “open-book tests of provider performance, where the questions have been given to the provider.” The hope is that as providers measure their own performance that quality of care will improve. SETMA has embedded some of the Consortium’s data sets into our EMR and we will report on the results of these as well as HEDIS.
The next button on the Medical Home Coordination Review template is entitled PCPPI Diabetes
Note: Remember, this button on shows up if the patient has the diagnosis of diabetes in their Chronic Problem list.
When launched this button automatically links the provider with the Consortium Data Set which is viewed from the Plan Template on the Diabetes Disease Management Tool which is launched from AAA Home
The following are the steps of how to access the Consortium Data Set via AAA Home. Of course, it can be launched as above from the Medical Home Coordination Review template.
The Diabetes Disease Management tool is launched from AAA Home.
Once the Diabetes Disease Management is launched the Consortium Data Set for Diabetes (entitled PCPPI Diabetes on the Medical Home Coordination Review template) is found by clicking on Plan in the list of navigational buttons on the Diabetes Master template

When the Diabetes Plan button is launched the following template appears.
On the Diabetes Plan template there is a button in the right hand upper part of the screen entitled Consortium Data Set
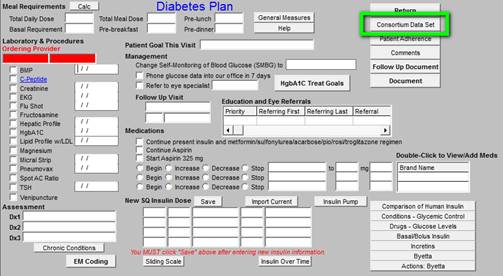
When the Consortium Data Set button is launched the following pop-up appears, which is the same pop-up which appears when the Medical Home Coordination Review PCPPI Diabetes button is launched:
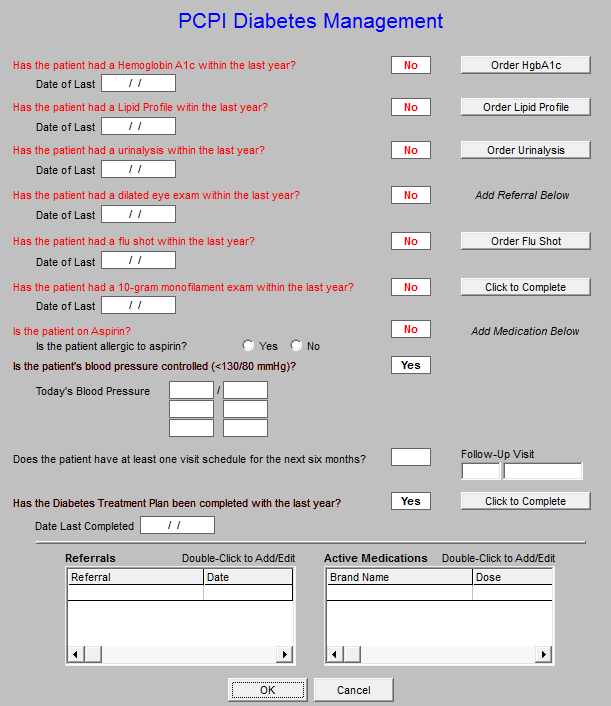
The 9 data points which are automatically captured and documented by SETMA's Diabetes Suite of Templates, and, which are collected and displayed on the Consortium Data Set pop-up on the Diabetes Plan, are the quality measures for diabetes developed by the Consortium.
These 9 data points are the basis along with several other data points of SETMA's Daily Diabetes Care Audit. These data points are:
- Collected automatically
- Provide a quick and easy review for the SETMA healthcare provider to evaluate his/her own Diabetes care.
- Provide a quick and easy way of completing the Diabetes measures required if they were not completed.
- Attention to these data points places in you line for additional reimbursement when CMS
- The Consortium material should be completed by the nursing staff and reviewed by the provider.
The Elements of the Consortium Data Set for Diabetes are listed on the pop-up.
(A complete tutorial for this function can be found in Appendix A below or on the Diabetes Disease Management tutorial)
The functioning of the Hemoglobin A1C element illustrates the above:
Hemoglobin A1C -
- The standard is that the patient has had a Hemoglobin A1C in the past three months or has one at this visit.
- The date of the last Hgb A1C is displayed on this template.
- If this data point is out of date, a button will appear to the right of the date box
- When you depress this button you will automatically order and charge post a Hgb
A1C, making it easier to do it right than not to do it at all.
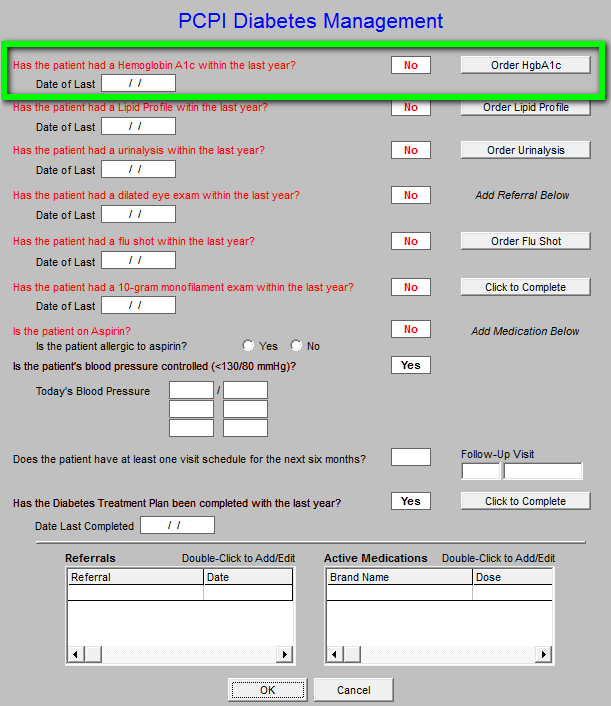
When this Diabetes management tool is accessed from the Medical Home Coordination Review template, any elements which are incomplete will appear in redand the button to the right of that element will appear. Any incomplete element can be quickly completed by clicking on the button in the right hand column.
The next button is entitled PCPPI Hypertension
When launched this button takes the provider to the Hypertension Disease Management tool and to the template entitled Physician Role. This template automatically collects the information from the patient encounter and notes whether each element of the evidenced- based management, identified by the PCPPI has been met. Here are eight elements as they are listed on the pop-up below.
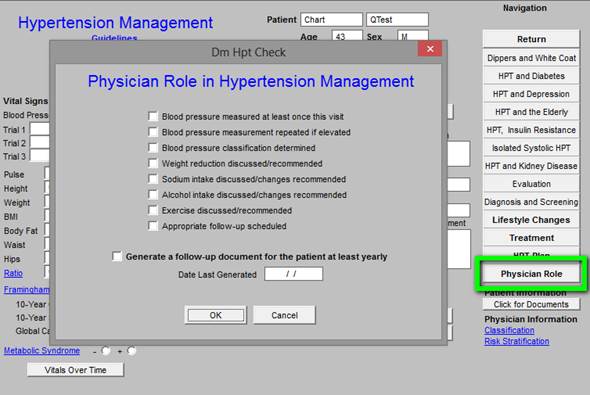
As the provider progresses through SETMA's Hypertension Suite of Templates, this template automatically collects the data points for the Physician Consortium for Performance Improvement Data Set for quality of care in hypertension management. A review of this template will allow a provider to see "how he/she is doing," as measured against a national standard of care in hypertensive management.
The standard of excellence in the management of hypertension is measured on the following 8 data points.
- Blood pressure measured at least once this visit
- Blood pressure measurement repeated if elevated
- Blood pressure classification determined
- Weight reduction discussed/recommended
- Sodium intake discussed/changes recommended
- Alcohol intake discussed/changes recommended
- Exercise discussed/recommended
- Appropriate follow-up scheduled
The elements of evidenced-based measures for hypertension are met in SETMA’s EMR:
- Completed by performing a blood pressure check during the current encounter
- Completed by repeating the blood pressure during the encounter if the initial pressure is above 140/90.
- Completed by using the Hypertension Disease Management templates which automatically calculates the classification, follow-up recommendation, risk group and treatment recommendation when the Calculate Assessment button is depressed on the Hypertension Master template
- Completed by accessing the Life-style changes template which is found on the Hypertension Master template and by completing the LESS Initiative
- Completed by accessing the Life-style changes template which is found on the Hypertension Master template and by giving the patient the Hypertension Follow-up document which includes instructions on low sodium diets.
- Completed by accessing the Life-style changes template which is found on the Hypertension Master template
- Completed by using the LESS Initiative with its Exercise Prescription.
- Completed by accessing the Life-style changes template which is found on the Hypertension Master template and by completing the LESS Imitative.
|