|
Index
- Introduction - Meaning of “moderately” and “high” complexity
- SETMA’s Tools for using TCM Code
- General Concepts about Transitions of Care Management Codes
- Revenue Summary
- TCM Code Requirement; SETMA’s 14-Year Preparation
- Analysis of Requirements for TCM Code
- Face-to-Face by MSW or RN in home fulfills contact obligation
- Medical Reconciliation Done Prior to or at Provider Face-to-Face
- Have a Face-to-Face within 7 or 14 days
- Face-to-face must include
- Post-discharge would include when indicated
In January, 2013, CMS published two new Evaluation and Management Codes (E&M Codes) which were adopted in order to recognize the value of the processes of transitioning patients from multiple inpatient sites to multiple outpatient venues of care. The value of this work is now being recognized by enhanced reimbursement. CMS has also published three codes for Complex Chronic Care Coordination, which is considered bundled payments in 2013 but in 2014 are scheduled for additional payment to primary care providers. Those will be discussed later.
SETMA has been tracking and auditing the Physician Performance for Performance Improvement Transitions of Care Quality Metrics since they were published in 2009. By provider name, those metrics are published at www.jameslhollymd.com under Public Reporting for 2009, 2010, 2011, 2012. In the past 36 months, SETMA has discharged over 14, 000 patients from the hospital. 98.7% of the time patients have received their Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan (previously called “Discharge Summary “when they left the hospital. Since 2010, SETMA’s Care Coordination Department has also been involved in the transitions process.
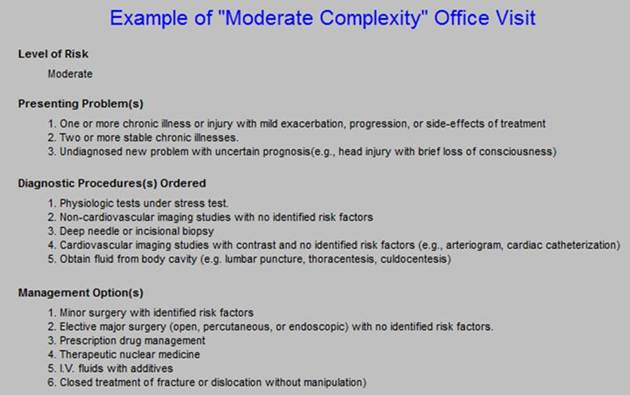
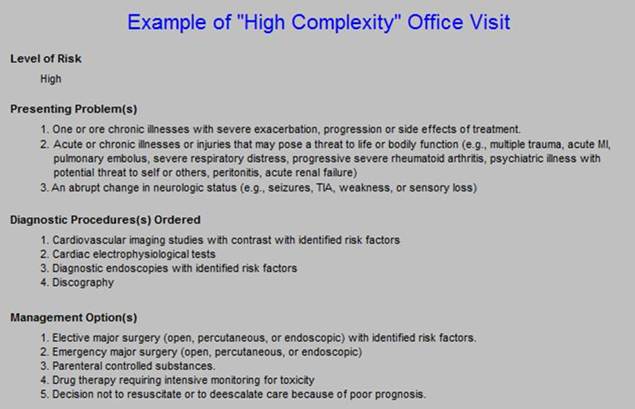
It is only logical that SETMA would be prepared to utilize the new Transitions of Care Codes. At this time, there is only one unresolved issue related to using these codes. Neither CMS nor the Medicare State Contractors are willing to clarify that issue. In order to determine which of the Transitions of Care Management Codes to use, the healthcare provider must distinguish between a Moderately Complexity visit and a High Complexity visit. This tutorial assumes that the complexity discriminator refers to the E&M codes for 99214 and 99215, in which case it would generally be possible for a provider only to use the lower of the TCM codes, i.e., 99495.
Others argue that the terms “moderate” and “high” complexity are not defined by the E&M code descriptions and if they are, the correct reference would be 99213 and 99214. That seems unreasonable as in that case, the higher TCM Code, i.e., 99496 would be the most commonly used TCM Code.
Until this is officially clarified, SETMA is going to assume that the terminology refers to 99214 and 99215. This will cause us to use a lower code than may be valid, but at least it will not result in fraud and abuse charges.
When a patient is seen at SETMA who has been discharged from the hospital or another in-patient setting, a note automatically appears on the AAA Home Template, indicating that the patient is eligible for a Transitions of Care Management evaluation. If the patient is not eligible, then that space will be blank. This alert is illustrated below outlined in green.

The two new Transitions of Care Management Codes (TMC Codes) have been added to SETMA’s E&M Template (see below outlined in green)
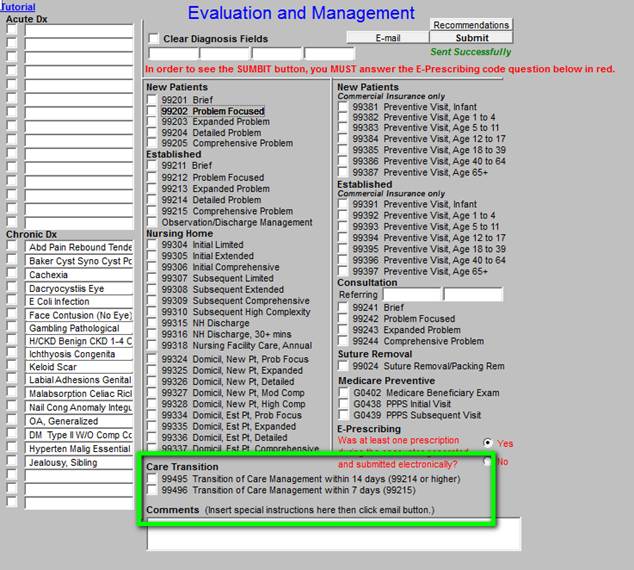
Surrounded in green are the TMC Codes: 99495 and 99496. Because the E&M Code 99215 will rarely be used in the ambulatory setting, and in that a 99215 E&M is required to bill for the 99496 TCM Code, most hospital follow-ups are going to be 99495 TCM Codes. As seen in the template below, SETMA has added a button entitled “Eligibility.”
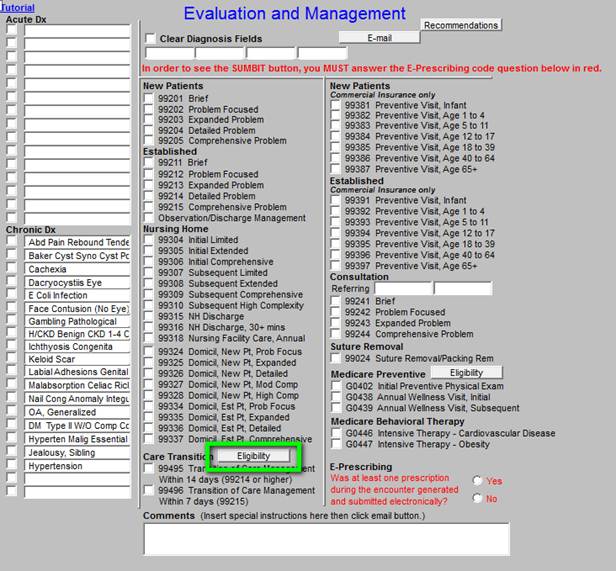
When this button (outlined in green above) is deployed, it will display the following template.
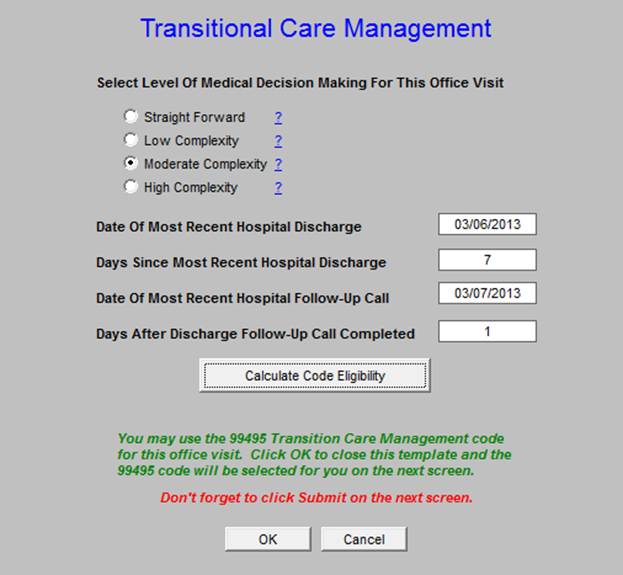
This template aggregates the information required for determining if you have qualified for one of the TCM Codes and if you have, which one. The functionality in the background of the template will search to see if the following requirements have been met:
- The patient is being seen in 7 or 14 days from discharge.
- The patient’s visit qualifies for a 99214 or a 99215
- The patient had a contact within two days of being discharged.
- Medication reconciliation was done after the hospital discharge.
- Plan of Care and Treatment Plan was given to the patient and/or care giver
When you click “Eligibility,” you will need to establish the complexity of the visit by clicking in the radial button next to the Complexity of the visit, i.e., moderate or high. If you have already selected the Complexity of Decision making level on the E&M template, you simply click on the “Calculate Code Eligibility” button and the appropriate TCM code will be selected.
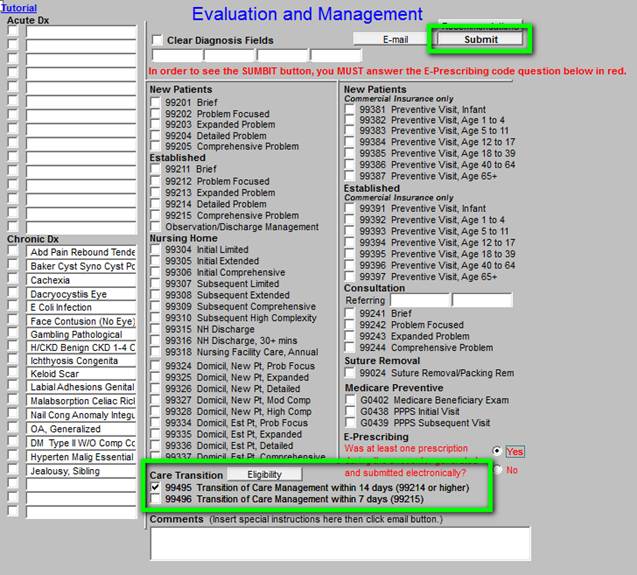
With SETMA’s patient population, there will be more than an average number of 99214 codes but there will be less than the average 99215 codes. Once you determine the medical complexity, the rest is straight forward. When you complete the steps above don’t forget to click the “Submit” button. See below in Green.
Two factors distinguish the codes 99214 and 99215
- The complexity of decision making - ask discussed above, it is unclear what this means at present.
- Whether the patient was seen within 7 days or within 14 days after discharge from the hospital
How to Determine 99214 or 99215 E&M Code Level
For 2013, CMS estimates two-thirds of all discharges will be eligible for TCM, representing approximately 6,667,000 claims. CMS’ assumption is that 75% of those claims will be submitted under 99495, which means that the 2013 TCM price tag will be approximately $1.34 billion (again, based on the 2012 conversion factor). With beneficiaries responsible for the 20% co-payment, CMS expects to pay $1.1 billion for TCM.
In order to bill for a TCM Service, the following must occur:
- The provider must have contact with the patient within two days of the patient leaving the hospital. SETMA’s hospital follow-up Care Coaching call qualifies for this contact. Note: If the patient is discharged from the hospital on Friday and no call is made until Monday, those patients do not qualify for the enhanced payment. The only adjustment to SETMA’s processes is that we must make sure that patients discharged on Friday receive a call by Sunday and that those discharged on Saturday, receive a call by Monday.
- Communicating (via direct contact, telephone, electronic) with the beneficiary and/or caregiver, including education of patient and/or caregiver within 2 business days of discharge based on a review of the discharge summary and other available information such as diagnostic test results, including each of the following tasks:
- An assessment of the patient’s or caregiver’s understanding of the medication regimen as well as education to reconcile the medication regimen differences between the pre and post-hospital, CMHC, or SNF stay.
- Education of the patient or caregiver regarding the on-going care plan and the potential complications that should be anticipated and how they should be addressed if they arise.
- Assessment of the need for and assistance in establishing or re-establishing necessary home and community based resources.
- Addressing the patient’s medical and psychosocial issues, and medication reconciliation and management.
- In lieu of a call, in cases of patients who are very high risk of re-admission, a face-to-face visit in the home by an MSW or an RN would qualify for the contact within 48 hours.
- Have Medication Reconciliation done prior to or at the time of the provider face-to-face visit.
- Have a follow-up call which is a 99214 (there will be very many of these) or 99215 (there will be very few of these). This requirement is not specific to the provider face-to-face encounter but is designated as “Medical decision making of at least moderate complexity during the service period.” The entire coding system for TCM is “for the service period,” which is for thirty days post discharge.
- Have a follow-up face-to-face with the provider (this must be done by a Nurse Practitioner or by a Physician) within 7 days for a 99496 or within 14 days for a 99495.
- At the face-to-face, this service would include:
- Assuming responsibility for the beneficiary’s care without a gap.
- Obtaining and reviewing the discharge summary.
- Reviewing diagnostic tests and treatments.
- Updating of the patient’s medical record based on a discharge summary to incorporate changes in health conditions and on-going treatments related to the hospital or nursing home stay within 14 business days of the discharge.
- Establishing or adjusting a plan of care to reflect required and indicated elements, particularly in light of the services furnished during the stay at the specified facility, and to reflect the result of communication with beneficiary.
- An assessment of the patient’s health status, medical needs, functional status, pain control, and psychosocial needs following the discharge. (This summary is from the American College of Physicians)
- When indicated for a specific patient, the post-discharge transitional care service would also include:
- Communication with other health care professionals who will (re)assume care of the beneficiary, education of patient, family, guardian, and/or caregiver.
- Assessment of the need for and assistance in coordinating follow up visits with health care providers and other necessary services in the community.
- Establishment or reestablishment of needed community resources.
- Assistance in scheduling any required follow-up with community providers and services.
The following is a published summary of the requirements of TCM coding:
Who is eligible to receive TCM services? |
Beneficiaries discharged from inpatient acute care hospitals (inpatient, observation, and outpatient partial hospitalization); skilled nursing facilities; and community mental health center partial hospitalization programs. |
What is the time period for TCM services? |
30-day period beginning on discharge date. |
Who is eligible to bill for TCM services? |
Physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified nurse midwives (referred to as “qualified professionals”). Rural health clinics and federally qualified health centers cannot bill for TCM. |
Must the beneficiary be an established patient of the qualified professional ? |
Previously established relationship is not required. |
What are the required elements for TCM services? |
(1) Communication with patient or caregiver within two business days of discharge (or two separate, unsuccessful attempts at communication).
(2) Face-to-face visit within fourteen days (99495) or seven days (99496)(cannot be performed on day of discharge; not separately billable; may be performed at any appropriate location; elements of visit not specified).
(3) Medication reconciliation and management performed no later than date of face-to-face visit.
(4) Non-face-to-face care management services (see next section for further explanation).
(5) Medical decision making of moderate complexity (99495) or high complexity (99496) (using E/M code definitions). |
What non-face-to-face care management services are required? |
The following services must be provided unless the qualified professional determines a particular service is not medically indicated or needed:
Performed by a qualified professional: obtain and review discharge information; review need for, or follow-up on, pending diagnostic tests and treatments; interact with other providers involved in patient’s care; educate patient, family, guardian, and/or caregiver; arrange for needed community resources.
Performed by clinical staff or case manager under direction of qualified professional: communicate with home health agencies and other community services utilized by patient; educate patient and/or family/caretaker regarding self-management, independent living, and activities of daily living; assess and support treatment regimen adherence and medication management; identify available community and health resources; facilitate access to necessary care and services. |
When can claims for TCM services be submitted? |
No sooner than 30 days following discharge. |
Can multiple TCM claims be submitted for the same patient? |
CMS will pay for only one TCM claim for the 30-day period following discharge. . The first claim to be filed will be paid. CMS will not pay a second TCM claim in connection with a discharge that occurs within 30 days of the original discharge (i.e., if the patient is readmitted and discharged within the 30-day period. |
Currently, reimbursement of clinic follow-up of patients discharged from the hospital is based on the standard E&M codes 99212-99215. There is no recognition of the increased time and enhanced services being provided primary care providers, and the reimbursement heretofore has been the same as for any patient encounter in the clinic. The standard, primary care payments for clinic visits are:
- 99212: $41.06
- 99213: $68.73
- 99214: $101.12
- 99215: $135.63
The new reimbursement for Transition of Care Management (TCM) Services will be:
- 99495: $154.53
- 99496: $218.27
To qualify for either of these codes, the underlying complexity of the follow-up visit must qualify for either a 99214 or a 99215 E&M Code. Because, a clinic visit, even a post-hospital follow-up, rarely qualifies for a 99215 E&M Code, the most common TCM code which will be used will be 99495.
To estimate the value of the TCM Codes, it is necessary to look at the change in reimbursement. If a hospital follow-up visit in the clinic previously qualified for a 99214 E&M Code, the provider was reimbursed $101.12. Now, if the elements of the TCM code 99495 are fulfilled, the reimbursement will be $154.53. Only one E&M Code can be used for each visit, therefore the net value of the new TCM Code at the 99495 level is $154.53 (reimbursement for 99495) minus $101.12 (reimbursement for a 99214 visit) is $53.42 per discharged patient seen in the clinic. In the rare exception when the requirements for a 99215 visit are met, the net value to the practice of a single visit would be $218.27 minus $135.63 or $82.64.
If SETMA discharges 5,000 patients a year and if 66% of them are eligible for a TCM code (as estimated by CMS), we would expect an increase in revenue of $176,286 per year. We have to reduce this expectation by the capitated Medicare Advantage patients and by the commercially insured patients we care for; this means that this number would be reduced by more than half.
This is not a great deal of money in a multi-specialty clinic but it is a significant step forward in recognizing the enhanced services clinics are offering today The following is a review of the requirements for using the new Transition of Care Management Codes (TCM) with a review of the process development which SETMA has done to make it possible for SETMA providers to respond to this opportunity for enhanced reimbursement with accuracy and validity.
Over the past fifteen years, SETMA has developed the use of electronic, systems-wide solutions which often were not reimbursed. We have always believed that the day would come when we would be compensated for the quality of our work. The TCM codes, along with the Physician Quality Reporting System, Meaningful Use and Bridges to Excellence are the most recent example of why our hard work is now “paying off,” both for our patients and our practice.
Below, we review each of the requirements for billing for TCM and then we discuss SETMA’s information technology and organization structural development for performing each of the tasks required.
Note: This section of this tutorial gives the element of the requirement for using the TCM Codes and following that a description of SETMA’s electronic medical record summary which makes it possible for us to use these codes. That explanation is introduced by the word “Preparation” which is displayed in red.
- The provider must have contact with the patient within two days of the patient leaving the hospital.
Preparation -- In August, 2010, SETMA began care coaching calls the day following a patient’s discharge from the hospital. We are now adding an MSW and an RN for home visits following hospitalization and for fragile patients who are at an increased risk of re-hospitalization.
- Communicating (via direct contact, telephone, electronic) with the beneficiary and/or caregiver, including education of patient and/or caregiver within 2 business days of discharge based on a review of the discharge summary and other available information such as diagnostic test results, including each of the following tasks:
Preparation - In 2001, SETMA began completing hospital discharge summaries in our EMR making them instantly available in the clinic, in the Nursing Home and in all other venues where patients are treated post hospital discharge. In 2005, SETMA reorganized the hospital care team such that now, 98.7% of the time the discharge summary is completed at the time the patient leaves the hospital. In >June 2009, the Physician Consortium for Performance Improvement published a Transitions of Care Measurement Set. SETMA immediately deployed that quality measure set and has audited our hospital charts since as to our performance on these measures. At www.jameslhollymd.com under Public Reporting, we publicly report by provider name these measures for 2009, 2010, 2011 and 2012. (See http://jameslhollymd.com/public-reporting/public-reports-by-type) Going forward this audit is published quarterly.
In August 2010, SETMA’s Care Coordination Department began making care-coaching calls to all discharged patients the day after discharge. In September, 2010, SETMA renamed the “discharge summary.” The new name is “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.” This plan includes a reconciled medication list, an assessment for potential of readmission, and all follow-up information.
- An assessment of the patient’s or caregiver’s understanding of the medication regimen as well as education to reconcile the medication regimen differences between the pre and post-hospital, Community Mental Health Centers, or Skilled Nursing Facility stays.
- Education of the patient or caregiver regarding the on-going care plan and the potential complications that should be anticipated and how they should be addressed if they arise.
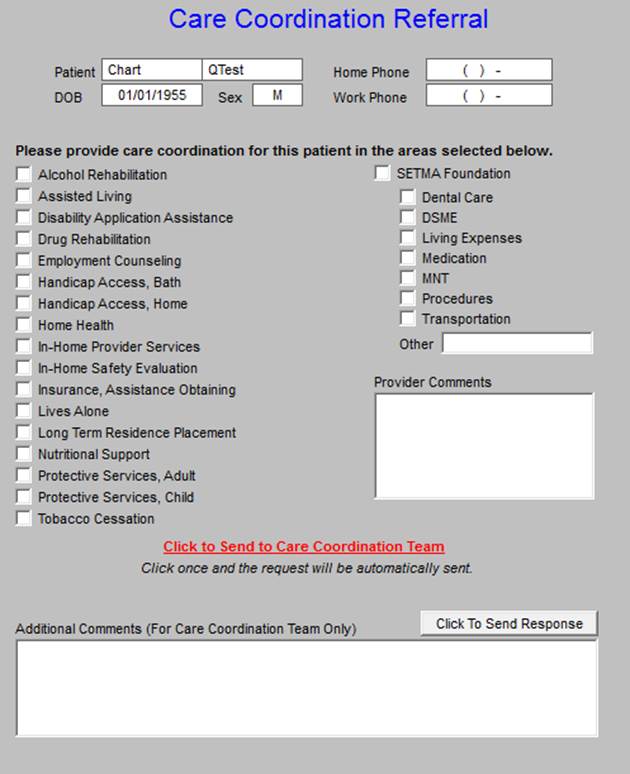
- Assessment of the need for and assistance in establishing or re-establishing necessary home and community based resources.
Preparation - A simplified solution to this is a referral template to the Care Coordination Department which requires less than five seconds of the provider’s time in obtaining home health, physical therapy, in-home provider support, Meals on Wheels, medications, financial support, DME, education, etc. This referral includes the ability to request patient support from The SETMA Foundation. Each year the partners of SETMA give $500,000 to the Foundation which money is used to help patients obtain care they cannot afford. None of that money can benefit SETMA.
- Addressing the patient’s medical and psychosocial issues, and medication reconciliation and management.
Preparation - At the time of discharge from the hospital and at the post-hospital visit, the SETMA healthcare team assesses Fall Risk, Pain, Function, Wellness and Stress. The tools which SETMA has deployed for these functions can be reviewed at http://jameslhollymd.com/epm-tools/Patient-Centered-Medical-Home-Annual-Questionaires. These tools allow SETMA providers and staff to uncover unspoken needs in the patient’s care.
- In lieu of a call, in cases of patients who are very high risk of re-admission, a face-to-face visit in the home by an MSW or an RN would qualify for the contact within 48 hours.
Preparation - SETMA completes a “readmission risk assessment” at the time a patient is admitted to the hospital. This is given to the patient in a document entitled, “Hospital Care Plan.” This document tells the patient why they were admitted, what they can expect as far as treatment and length of stay, gives them a reconciled medication list and gives them the admission estimate of their risk of readmission. The risk assessment is repeated upon discharge and is reported to the patient, or care giver in the Hospital Care Summary and Post Hospital Plan of Care, which they are given at discharge. The security and confidence the MSW and RN give to the patient that their healthcare needs are and will be met is significant. It begins correcting the idea that the emergency department is the patient’s only healthcare safety net.
- Have Medication Reconciliation done prior to or at the time of the provider face-to-face visit.
Preparation - a medication reconciliation is done at admission, at discharge, at the time of the care-coaching call the day after discharge and at the hospital follow-up visit which takes place in two days for patients at high risk of readmission and within five days for all others.
- Have a follow-up visit which is a 99214 (there will be very many of these) or a 99215 (there will be very few of these). This requirement is not specific to the provider face-to-face encounter but is designated as “Medical decision making of at least moderate complexity during the service period.” The entire coding system for TCM is “for the service period,” which is thirty-days post discharge. It is this idea which may allow for coding more 99496 TCM codes than we presently think.
Preparation - SETMA has the ability to correctly assess the complexity of medical decision making based on published CMS guidelines. This allows SETMA to assess the correct Evaluation and Management code in order to correctly determine that the Transition of Care Management codes are appropriately used.
- Have a follow-up face-to-face with the provider (this must be done by a Nurse Practitioner or by a Physician) within 7 days for a 99496 or within 14 days for a 99495.
Preparation - SETMA has launched functionality in the EMR to make these management codes available. (See Above) This functionality includes automation of the determination of whether the:
- Level of E&M is achieved which is required for the TCM,
- Contact within two days post discharge was done,
- Patient is seen within seven or fourteen days post discharge,
- Medication reconciliation has taken place,
- Plan of care and treatment plan has been given to the patient or caregiver.
Ongoing training will take place with SETMA’s providers to make certain that these codes are used properly. Ongoing auditing of provider compliance with CMS requirements will be done.
- At the face-to-face, this service would include:
- Assuming responsibility for the beneficiary’s care without a gap.
Preparation - The SETMA care is seamless between the inpatient and the ambulatory care setting. The same EMR is used in both. All care is documented in the same data base. The four medication reconciliations for each admission are all performed on the same medication list. The hospital admission plan of care, the hospital care summary and post hospital plan of care and treatment plan, the care- coaching call and the follow-up face-to-face visit are all competed in the same data base. While there is continuity of personalities helping with the patient’s care, the ultimate continuity-of-care is data driven by the EMR being used at ALL points of care.
- Obtaining and reviewing the discharge summary.
Preparation - The discharge summary, which for SETMA is a much more robust and dynamic document is instantly available in the ambulatory setting whether that is the clinic, the emergency department, the nursing home, the SNF, the home health, the hospice, or any other venue of care. A SETMA provider, performing a TCM face-to-face visit, has the entire hospital documentation immediately available at the time of discharge. In addition, fulfilling HIPPA security regulations and only giving designated healthcare professions of long-term care facilities access to the information for patients in their facilities, SETMA makes the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan immediately available.
- Reviewing diagnostic tests and treatments.
Preparation - The Hospital Care Summary includes all diagnostic tests, consultations, treatments and assessments. Once again the continuity of care is seamless because the records are simultaneously and instantly available everywhere. As an aside, SETMA’s confidentiality and security of patient information is state-of-the art with two-factor identification and random, eight digits, numerical codes which change ever sixty seconds and which codes are uniquely tied to each provider so that every provider gets a different code which changes every sixty seconds.
- Updating of the patient’s medical record based on a discharge summary to incorporate changes in health conditions and on-going treatments related to the hospital or nursing home stay within 14 business days of the discharge.
Preparation - The diagnoses, assessments, medications, laboratory results are not only instantly available but they are dynamically interactive with the rest of the record. For instance, a hemoglobin A1C which is done in the hospital is documented in SETMA’s records and will display on Disease-specific Management tools. So, if you are accessing the most recent HbA1C after a hospitalization or an LDL the last one displayed will be the one from the hospital and not one from the clinic four weeks before. As described in 6b above, using two-factor authentication including an 8 digit, random number which changes every sixty seconds and which is unique to the specific personnel, appropriate professional team members are given access to the patient’s laboratory data.
- Establishing or adjusting a plan of care to reflect required and indicated elements, particularly in light of the services furnished during the stay at the specified facility, and to reflect result of communication with beneficiary.
Preparation - Because the plan of care and treatment plan established at discharge is a part of the patient’s permanent record, it is automatically incorporated into the ongoing plan of the patient based on diagnoses, medications, treatment plans and treatment goals.
- An assessment of the patient’s health status, medical needs functional status, pain control, and psychosocial needs following the discharge. (This summary is from the American College of Physicians)
Preparation - As addressed above, at the time of discharge from the hospital and at the post-hospital visit, the SETMA healthcare team assesses Fall Risk, Pain, Function, Wellness and Stress. The tools which SETMA has deployed for these functions can be reviewed at http://jameslhollymd.com/epm-tools/Patient-Centered-Medical-Home-Annual-Questionaires These tools allow SETMA providers and staff to uncover unspoken needs in the patient’s care.
- When indicated for a specific patient, the post-discharge transitional care service would also include:
- Communication with other health care professionals who will (re)assume care of the beneficiary, education of patient, family, guardian, and/or caregiver.
Preparation - SETMA’s Care Coordination department is electronically linked with all other SETMA providers. Internal referrals to specialists, education or testing are seamless. Referrals and transmittal of information to those providers external to SETMA are completed easily with documentation of “sent” and “received.”
- Assessment of the need for and assistance in coordinating follow-up visits with health care providers and other necessary services in the community.
Preparation - The interface between SETMA’s Care Coordination Department and providers is simple and seamless. Regardless of the patient need, it takes only seconds for a provider to make a referral to the Department from a pre-established list of options.
|