|
In an effort to decrease the inappropriate use of antipsychotic medications in Texas Nursing Homes, The Texas Medical Foundation and the Texas Department of Aging and Disability provided this toolkit. Because SETMA provides care to over 90% of the long-term care residents in Southeast Texas, which comprises a five county area, and because SETMA documents the care of those patients in our electronic patient record (EMR), we have taken this tool kit and created a Clinical Decision Support tool to improve the care of the patients for whom we have responsibility.
The following are the templates and functionalities which are now deployed in our EMR.
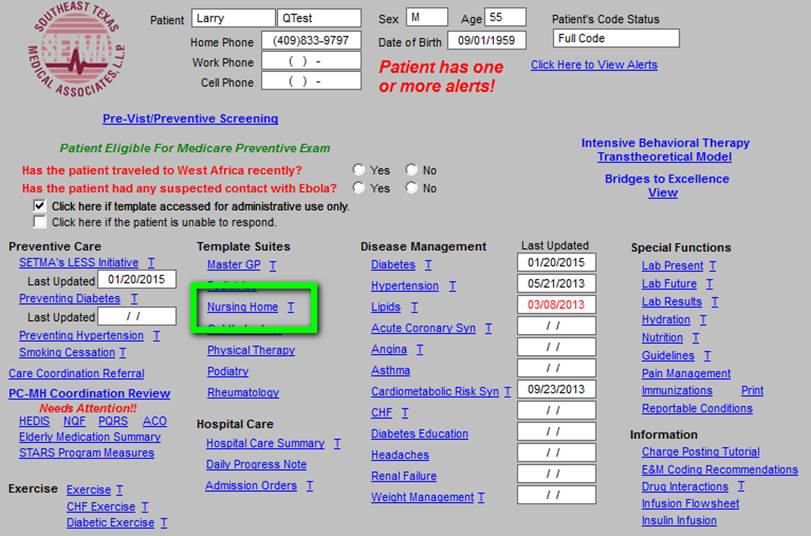
First is the principle template which launches all of our electronic patient care. Outlined in green on this template is the hyperlink which launches the Nursing Home suite of templates.
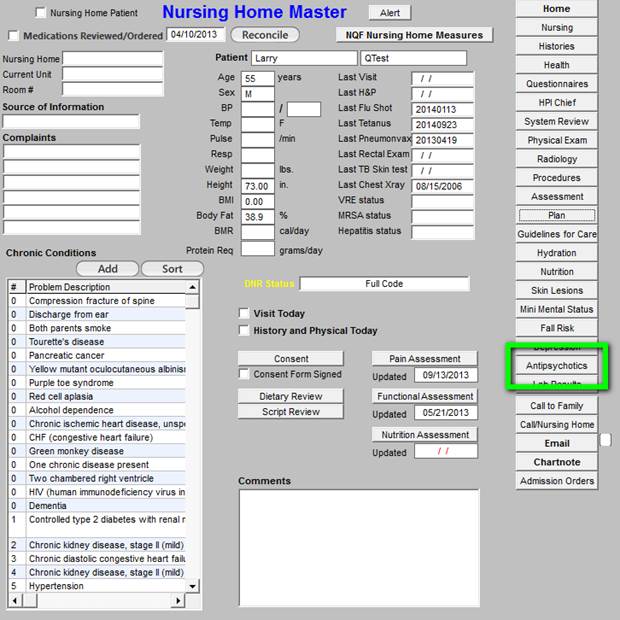
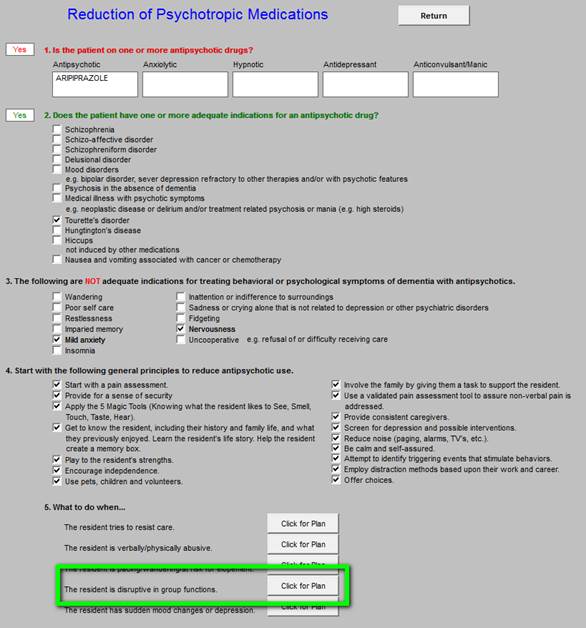
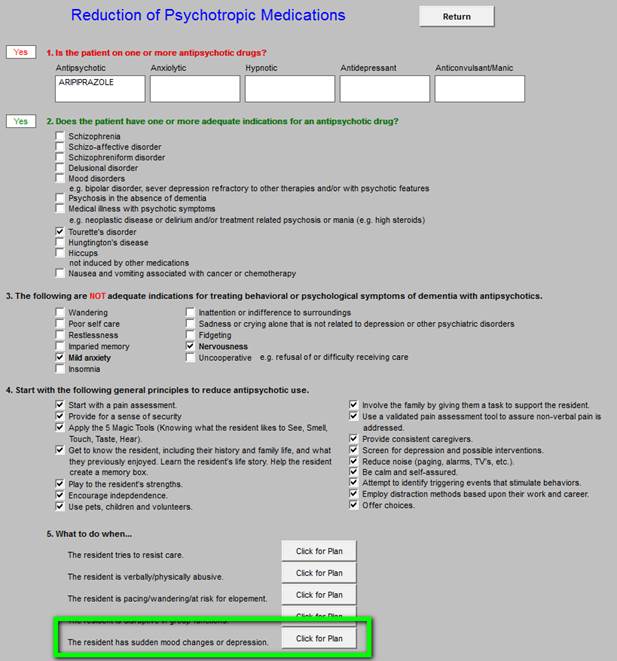
When the Nursing Home hyperlink is deployed the Nursing Home Master template is deployed. Outlined in green is the button which launches the Antipsychotics Toolkit. There are five sections to the tool kit:
- Is the patient on one or more antipsychotic drugs?
- Does the patient have one or more diagnoses for an antipsychotic drug?
- The following are not adequate indications for treating behavioral or psych9ological symptoms of dementia with antipsychotics.
- Start with the following general principles to reduce antipsychotic use.
- What to do when€¦
When this button is deployed, the EMR is searched for Antipsychotic Drugs in these Classifications:
- Antipsychotic
- Anxiolytic
- Hypnotic
- Antidepressant
- Anticonvulsant/Manic
This is a partial list of psychotropic drugs commonly used in the long-term care setting. Some of these drugs are listed under their official classifications, but may be seen with the intended use of the above classifications to alter/change mood or behavior. Any drugs which are found are automatically listed under its category.
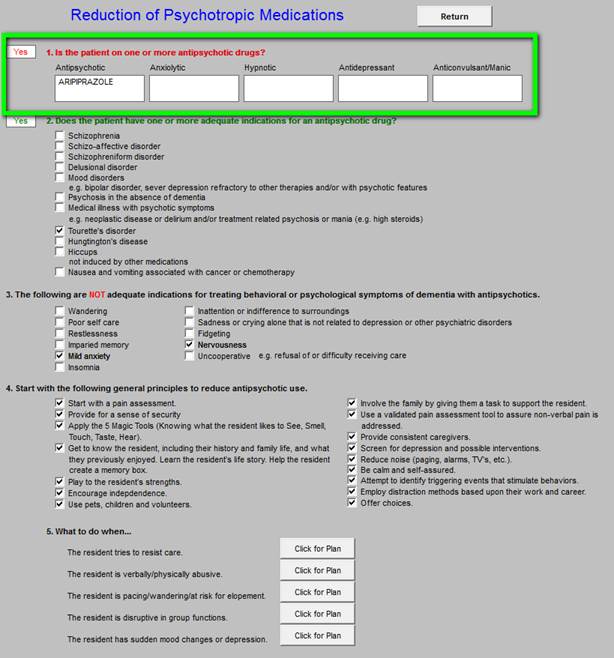
In section 2 of this template, the computer automatically denotes: “Does the patient have one or more adequate indications for an antipsychotic drug?” See below for details.
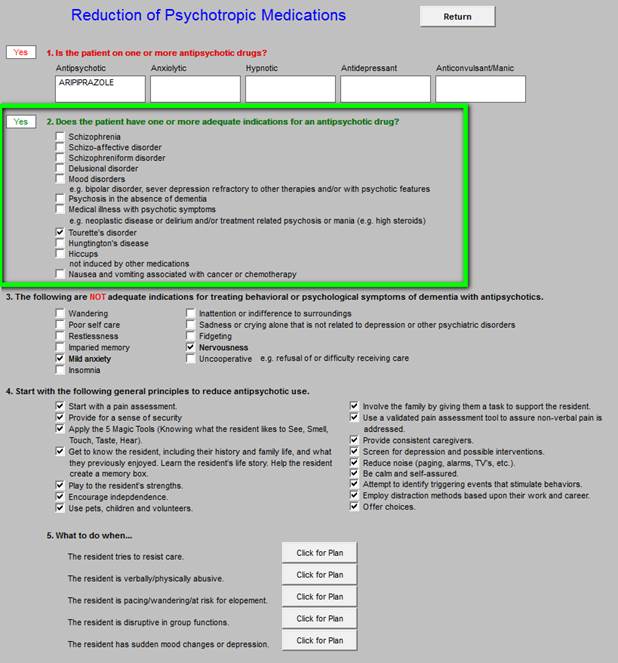
If there is no appropriate diagnosis for the use of an antipsychotic medication, consideration should be given for discontinuing the medication and/or for employing one of more of the therapeutic or environment interventions provided below.
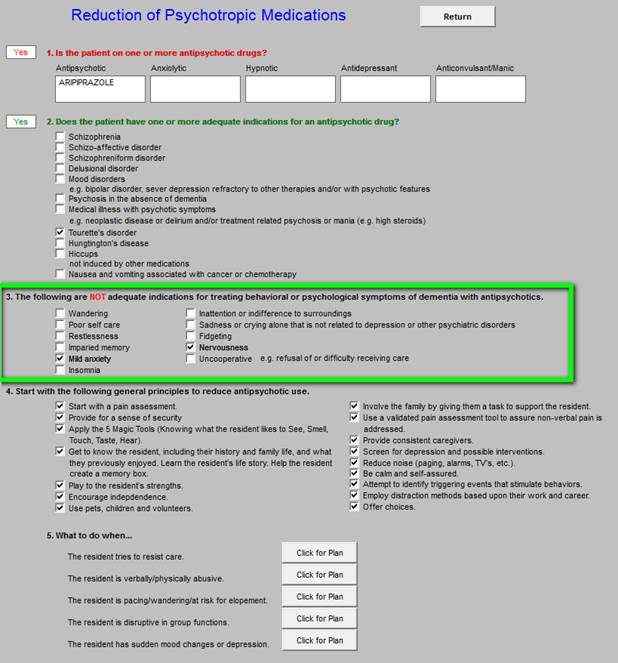
Section 3 of the tool kit lists the indications for which antipsychotics are often used but which are inadequate indications for such use.
Section 4 lists alternatives for antipsychotic medications when there is not an indication for their use. This section lists 16 actions which can be instituted to decrease the use of antipsychotic medications. The example shows all of the actions checked off but generally you would only began a few a time.
Those which you check off will appear on the chart note to be placed on the nursing home chart or on the chart of a patient in the clinic.
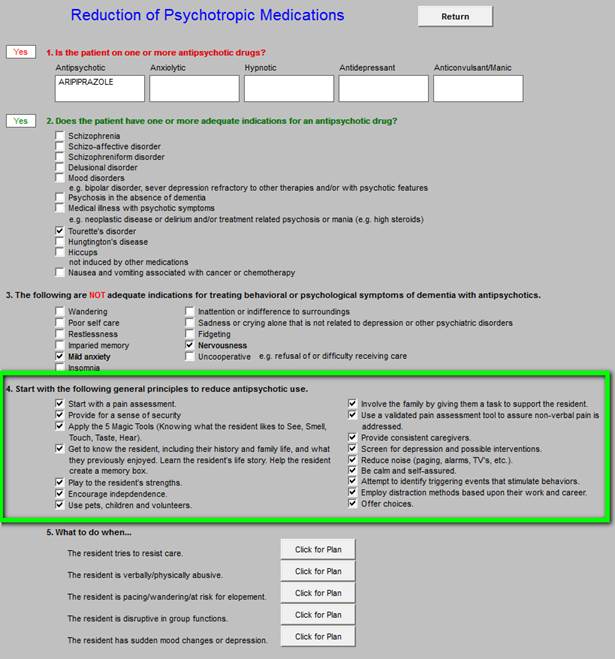
The above principles are used for the reduction of the use of physical restraints. The most important actions are to start with a pain assessment and a screen for depression. These assessments can be done with tools provided by SETMA: see Patient-Centered Medical Home Annual Questionnaires for:
Fall Risk, Pain Assessment, Functional Assessment, Wellness and Stress; see Depression Tutorial for depression evaluation.
Fear is created by disorientation and confusion. The “5 Magic Tools” are helpful in enhancing orientation and decreasing confusion. These “Magic Tools” involving “knowing what the resident likes to See, Smell, Touch, Taste, Hear.” Remember that new and/or strange environments can disorient and confuse patients. Using these five sensory perceptions to create a familiar and pleasant environment can help patients regain their sense of security and safety.
Section five is entitled “What can be done when€¦” Each of the five “What Can Be Done” recommendations give specific guides for helping patients cope with their new surroundings and with their decreasing menial acuity.
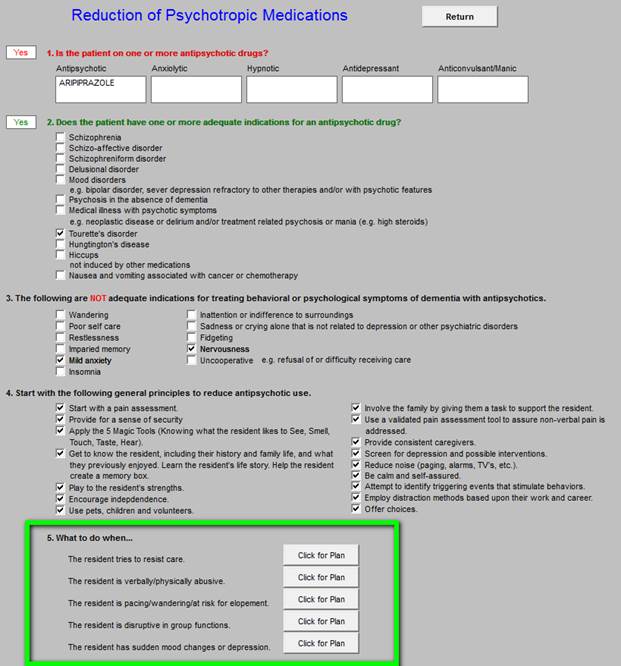
The five categories of “What to do when€¦” are:
- The resident tries to resist care
- The resident is verbally/physically abusive
- The resident is pacing/wandering/at risk for elopement
- The resident is disruptive in group functions
- The resident has sudden mood changes or depression
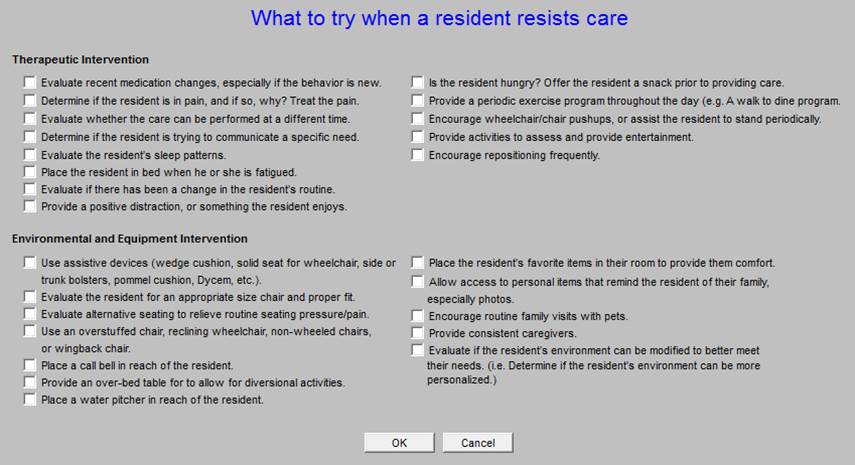
The first is “what to do when the patient resists care.”
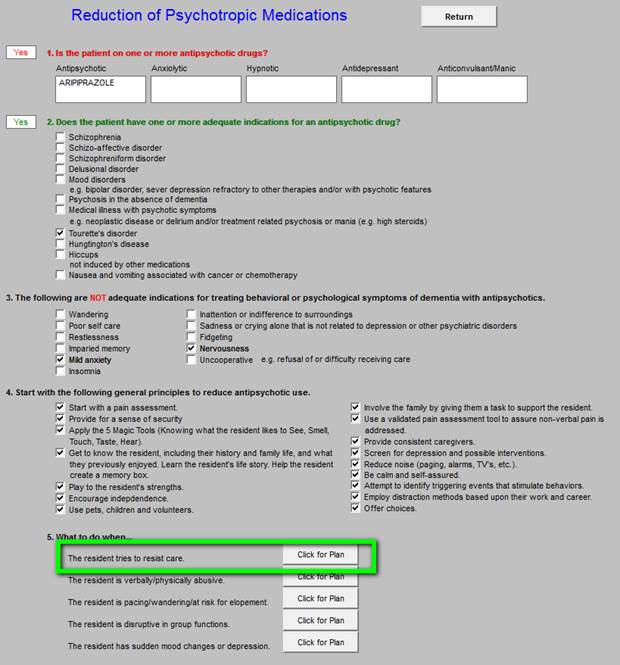
When the patient resists care, the following suggests may be helpful. There are two categories:
- Therapeutic Interventions
- Environmental and Equipment Intervention
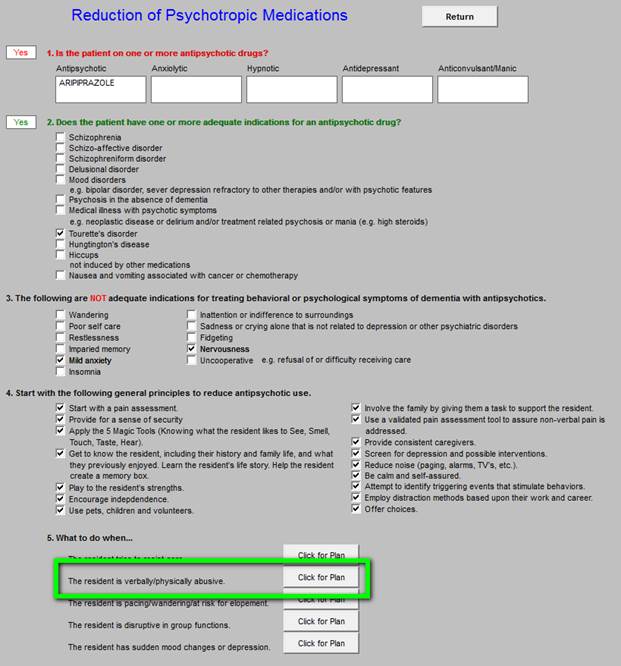
The second category is “What to do when the resident is verbally/physically abusive.”

The second category is “What to do when the resident is verbally/physically abusive.”
When specific boxes are checked, they will appear on the chart note, which then can be placed on the chart as a plan of care and treatment plan.
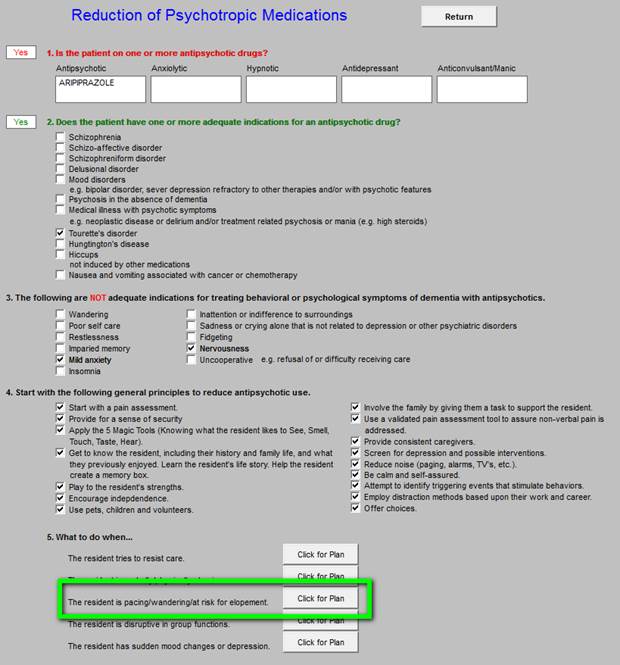
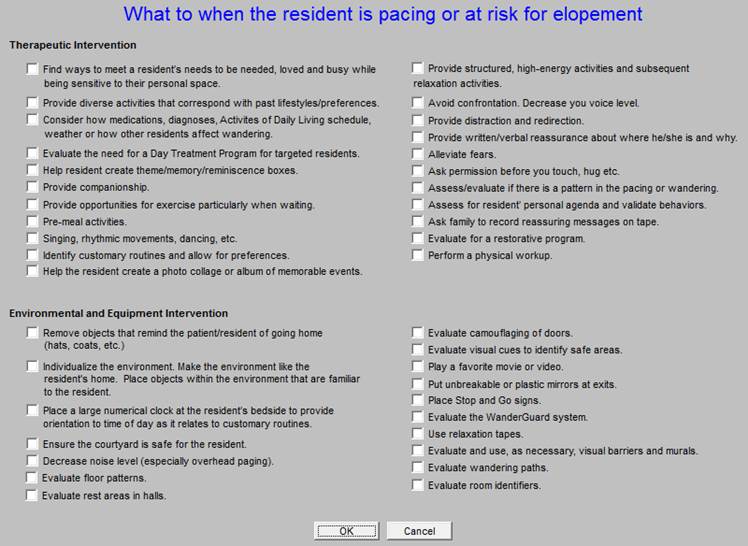
The third category is “What to do when the resident is pacing/wandering/at risk for elopement.”
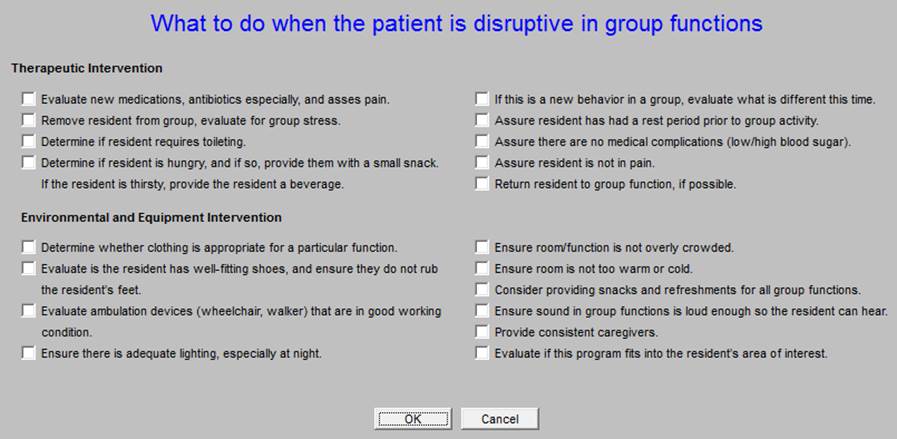
The fourth category is “What to do when the resident is disruptive in group functions.”
These are the therapeutic and environmental recommendations for residents who are disruptive in a group.
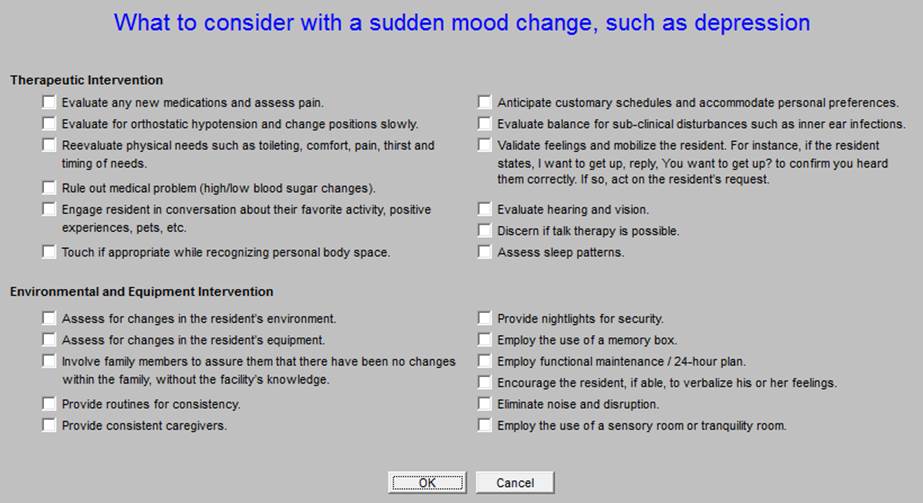
The fifth and last section of “What to do when€¦” relates to when “The resident has sudden mood changes or depression.”
The following are the therapeutic and environmental recommendations for residents who have sudden mood changes and/or depression.
As with all clinical decision supports, this tool kit is evaluational for the resident and it is also educational for the provider. The more familiar caregivers become with these interventions both therapeutic and environmental, and the more frequently the caregivers use this tool kit, the more effective the facility and caregivers will become in appropriately using antipsychotics for the benefit of the resident.
Once the tool kit is reviewed in the care of a resident with the checking off of the intended interventions, the chart note will be completed and will be placed on the resident’s chart. The result of the resident’s evaluation with this tool kit will be reviewed by the team caring for the resident. The recommendations and interventions will be incorporated into the care plan for the resident.
|