|
As SETMA has continued to develop its Patient-Centered Medical Home, we have worked with the guidance of the standards published by CMS, NCQA and AAAHC, as well as the medical literature. We have also worked independent of the published materials to develop our concept of Care Coordination in our efforts to achieve Coordinated Care.
Our PC-MH Coordination Review template has been discussed at the following link. (http://jameslhollymd.com/epm-tools/Tutorial-Medical-Home-Coordination-Review ) It provides a tool in which to review many of the elements required in order to produce coordinated care. A new tool has now been added. As demonstrated below it is entitled Care Coordination Referral and it is launched from the AAA Home Template in our EMR.
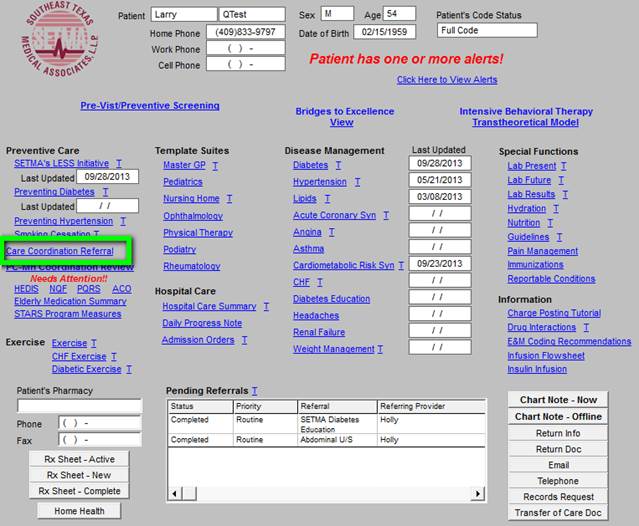
When depressed, the “Care Coordination Referral” template is launched.
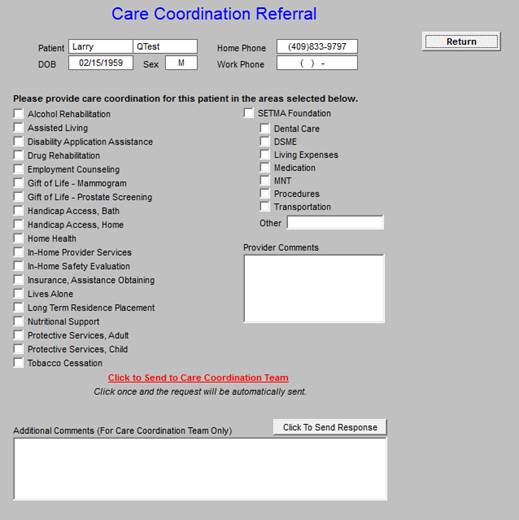
This template allows the provider and/or nurse to send an e-mail to Care Coordination which gives guidance for the special needs which a patient has. Several functions are included with this template:
- If a provider completes three or more referrals in any given encounter, an e-mail is automatically sent to the Director to allow for the coordination of those referrals to increase convenience and compliance.
- The first column allows for the provider to indicate the special needs which the patient has and which would or might benefit from a follow-up contact from the Care coordination team.
- A comment box is present which allows for a description of a need not covered in the list.
- The second column allows for the provider to indicate that the patient has financial needs and the service for which that need exists.
Once the provider or nurse checks the needs which exist, the red button entitled “Click to Send to Care Coordination Team” is launched. The button will turn to green which indicates that the e-mail has been sent to the Director of Care Coordination.
Care Coordination Tasks
The following are a list of “duties” performed by the Care Coordination Department. Keep in mind that the Department encounters many other patient needs which are taken care of as they arise:
- Hospital follow-up calls the day after hospital discharge for every patient. At the time of the call, the staff also does an assessment for any barriers the patient may have to their medical care. The following takes you to the tutorial for how to schedule and execute the call. ( http://jameslhollymd.com/epm-tools/Tutorial-Hospital-Follow-up-Call) As of September, 2013, the Department is making over 33,000 calls a year.
- On Fridays, patients that are in our workflow before 11:30am, showing that they are being discharged that day, are contacted by phone and information is given on how to contact the SETMA provider on call for afterhours and through the weekend. Patients are encouraged to contact the provider before simply returning to the ED.
- Clinic follow-up calls for patients that are at high risk for readmission to the hospital are scheduled by this department after the initial follow-up call. These calls are made to the at-risk patient, three days after the initial call or in the case of a patient that sees the provider on the third day after discharge, the patient is contacted the next day.
- Clinic follow-up calls for patients following an office visit with a provider. These are done as requested by the provider and can be scheduled 1 or 2 days following the visit or later as per the providers instructions. Information requested is documented and sent back to the provider.
- Follow-up calls to patients that miss a hospital follow-up appointment. A report is generated to this department at 8:30am daily and these calls are priority. If we are able to contact the patient, we try to reschedule a same day appointment if at all possible. Also at this time, the staff does an assessment for any barriers the patient may have to accessing the medical care needed.
- Follow-up calls to patients with HTN or DM that miss a scheduled appointment with their provider. Also assessing any barriers the patient may have to receiving the medical care needed.
- For patients with Next MD accounts and upcoming visits, pre-visit information is sent via this account, as well as those keeping their appointment receive post visit documents from the visit to their electronic account.
- Follow-up calls to all patients that have 3 or more referrals at one time. The Department always asks if the patient have any hindrances to completing the referrals and if they are in agreement with their treatment plan. If they have any transportation issues, co-pay issues or scheduling issues we work to resolve those.
- Infectious disease reporting. Patient demographics and documentation regarding the disease (chart notes, lab work) are faxed to the Beaumont Health Department’s epidemiology nurse. This is per the state protocol €“ reporting to the region with the region compiling data and then reporting to the state.
- All patient complaint calls. Department staff works diligently to accommodate the patient and resolve any issues. Complaints are documented and sent to the Director of Operations and the supervisor of the area where the complaint originated.
- SETMA Foundation assistance. Patients in need are contacted and information is sent to the SETMA Foundation for approval. All arrangements for needed care are handled through this office if assistance is approved by the Foundation.
- The Department also arranges assistance through community programs as needed (Meals on Wheels, Transportation for Seniors, APS when appropriate, etc). Currently, at SETMA II where this department is housed, we are available to assist the providers with patients that are in the office needing assistance.
Coordinated Care
One of the “catch phrases” to medical home is that the care is “coordinated.” While this process traditionally has referred to scheduling, i.e., that visits to multiple providers with different areas of responsibility are “scheduled” on the same day for patient convenience, it has come to mean much more to SETMA. Because many of our patients are elderly and some have limited resources, the quality of care they receive very often depends upon this “coordination.” It is hard for the frail elderly to make multiple trips to the clinic. It is impossible for those who live at a distance on limited resources to afford the fuel for
multiple visits to the clinic.
“Coordination” has come to mean to SETMA, scheduling which translates into:
- Convenience for the patient which
- Results in increased patient satisfaction which contributes to
- The patient having confidence that the healthcare provider cares personally which
- Increases the trust the patient has in the provider, all of which,
- Increases compliance in obtaining healthcare services recommended which,
- Promotes cost savings in travel, time and expense of care which
- Results in increased patient safety and quality of care.
As with the structure of quality metrics in tracking, auditing, analyzing and public reporting process and outcomes measures, coordination requires intentional efforts to identify opportunities to:
- Schedule visits with multiple providers on the same day, based on auditing the schedule for the next 30-60 days to see when a patient is scheduled with multiple providers and then to determent if it is medically feasible to coordinate those visits on the same day.
- Schedule multiple procedures, based on auditing of referrals and/or based on auditing the schedule for the next 30-60 days to see when a patient is scheduled for multiple providers or tests, and then to determine if it is medically feasible to coordinate those visits on the same day.
- Scheduling procedures or other tests spontaneously on that same day when a patient is seen and a need is discovered.
- Recognizing when patients will benefit from case management, or disease management, or other ancillary services and working to resources those needs.
- Connecting patients who need help with medications or other health expenses to be connected with the resources to provide those needs such as The SETMA Foundation, or sources.
Time, energy, and expense are conserved with these efforts in addition to increasing compliance thus improving outcomes. In order to accomplish this and to gain the leverage, synergism and advantage of coordination, a system is necessary which brings us to a new position designed by SEMTA entitled, Director of Coordinated Care.
Director of Care Coordination (DCC)
The Director of Care Coordination is responsible for building a department of Care Coordination. In many ways this could be called the “Marcus Welby Department,” as it recognizes the value of each patient as an individual and has as its fundamental mission the meeting of their healthcare needs and helping them achieving the degree of health which each person has determined to have. The driving force is to make each patient feel as if they are SETMA’s ONLY patient, just like Dr. Welby.
Initially, the DCC will work as a department of one but will have others assigned to the department as the demands of the mission expand. The DCC will establish protocols and methods for facilitating the care of patients with: special needs, complex-care needs, disease management and case management needs.
An illustration of this new function will be that of a patient who is seen at SETMA’s Wilson clinic on the West End of Beaumont. The provider determines that the patient needs an echocardiogram. The nurse will call the Care Coordination Department, which will determine if the patient can be sent to the Ultrasound Department immediately to have the test done that day. We believe that this will increase patient satisfaction as well as compliance which will improve the quality of care the patient will receive.
Integration of Care
The medical home sees the patient as a whole and not as a collection of isolated and disconnect disease processes. While this is not new and has always been the ideal of health care, it becomes a significant focus of the patient-centered medical home. Not only is the patient the major focus of the attention given, but all elements of the patient’s needs are attended to and future needs are anticipated and addressed. No longer is a patient encounter simply used to address current needs but potential future needs are identified and addressed. For instance, the young person who is seen for an upper respiratory condition but who is moderately obese, and who has a family history of diabetes, has his disease-risk addressed. In addition, recommendations are made for diabetes prevention and wellness including exercise, weight reduction, avoiding tobacco and others. Future contacts are scheduled, with our without a clinic visit, for assessing whether the patient has made the changes necessary to maintain their health.
Furthermore, through NextMD, SETMA’s secure web portal, the patient is referred to education material for achieving the desired results and a follow-up contact via e-mail is scheduled to remind the patient, without a clinic visit and without cost, to pay attention to their health.
Quality of Care and Patient Safety
A medical home measures the quality of care which patients are receiving both through process analysis and outcomes measurement through quality metrics. Quality Improvement Initiatives are planned for the improvement of care across an entire population of patients. For instance, while it is anticipated that the new Director of Coordination of Care will result in improved care, that must be measured and analyzed before it will become obvious that the anticipated improvement has occurred.
As the Director of Care Coordination works with SETMA’s Call-Center staff to address preventive health needs of our patients, it will be important to see if more people are getting their mammograms, bone densities, immunizations, etc. If they are, then the position will have
proved value. If they aren’t then new ways will have to be used to improve those outcomes.
If the DCC is responsible for scheduling multiple visits or studies on the same day, it will be necessary to measure whether or not that has improved compliance and consequently quality of care.
If the DCC is responsible for evaluating whether the post-hospital follow-up call program and the post-clinic-visit follow-up call program is having the desired result, it will be necessary to measure those outcomes. If the desired result does not occur new or additional initiatives will have to be designed.
Continuity of Care
To be a medical home, a practice must provide communication with a personal physician who accepts primary responsibility for the patient’s care. This is more than a friendly affect when the patient is seen in the clinic. It means answering inquires about health from the patient at times other than when they are seen in the clinic. It means providing telephone access with same-day response; e-mail contact through a secure web portal with same day access; it mean eliminating a patient’s anxiety about whether or not their healthcare provider cares about them by the provider being available to the patient. It may mean in some cases that the patient has the provider’s
home telephone number or cell phone number. It means doing whatever is necessary for making sure the patient knows how to access care when it is needed. The reality is that the more confident a patient is that they can reach their provider when needed; the less likely the patient is to pester the provider over trivial or unimportant matters.
Continuity of care in the modern electronic age means not only personal contact but it means the availability of the patient’s record at every point-of-care. One of the AAAHC surveyors said that his standard for judging medical records is, “Could I pick up this chart and provider excellent care for a patient whom I had never seen?” His answer after reviewing dozens of SETMA charts is, “I could easily treat any of these patients as the records are legible, complete and well organized.” Because all of the patient’s health needs are clearly documented; because all preventive and screening health needs are constantly and automatically audited; because every patient’s laboratory results, medications and diagnoses are interactive; every patent can be confident that all of their health needs are being addressed, can be addressed and will be addressed, no matter who the provider is that they see..
Another issue of continuity of care is communication among all providers and institutions that are providing care for each patient. The Health Information Exchange which SETMA is launching will provide the confidence that care given by hospitals, emergency rooms, specialists, other primary care providers, etc., will be accessible to all providers and will be integrated into the patient’s health record. In addition the secure web portal, NextMD, will allow the patient to maintain and periodically review their own personal health record. This places the patient at the center of their healthcare decision-making process, which is the ideal of patient-centered medical home.
|