 |
James L. Holly, M.D. |
|
 |
|
|
|
|
|
|
|
|
Designing an EMR on the Basis of Peter Senge's The Fifth Disciple
James L. Holly, MD
Abstract:
It is possible for healthcare providers to be overwhelmed by the volume of valuable information available for medical decision making. The organization and storage of that information is particularly ill suited for easy access and application in clinical settings. Electronic patient records has the potential for making current and future information available for use in improving the quality of treatment out comings.
Success in applying medical science and random-controlled-trials date to healthcare will be dictated by the design of EMR products and particularly by the display of data and treatment decision-making tools. In his book, The Fifth Discipline, Dr. Peter Senge identifies "systems thinking" as the solution to the management of complex data issues in business. These principles are equally applicable in medicine and particularly in the design of EMR tools for the support of healthcare decision making.
Utilizing Senge's concepts of metanoia and circular causality, this paper examines the implications of systems thinking for the design of EMRs and for the display of data. In addition, the issues of data sharing between specialties, disciplines and disease management is addressed.
Introduction
The complexity of medical knowledge is created both by its volume and by the manner in which that information is packaged. Applying that complex knowledge base effectively will require a fundamental shift in physician approach to information. Electronic medical records (EMR) provides the means for that shift but does not dictate that such a shift will take place. Often EMR is only used as a glorified transcription tool whereby a patient encounter is documented electronically without providing significant advantages in processing of information and without the patient profiting from sound science.
Systems Thinking and Healthcare
In his seminal work, Dr. Peter Senge addresses "systems thinking." While the term does not refer to computer systems, the principles apply to health care delivery via an electronic format as legitimately as to other business enterprises.
Senge states, "Learning has come to be synonymous with 'taking in information.'...Yet, taking in information is only distantly related to real learning." Classically, healthcare has focused upon "taking in information" in the form of facts. The hurdle required to enter medicine as a physician is the proven ability to absorb and retain tens of thousands of isolated pieces of information and then to be able to repeat that information in a test format. Clinical training attempts to take the static database created by these facts and transform it into a dynamic tool which can provide answers to complex disease-process questions. This is where the complexity comes into healthcare: how do you take a linear database and transform it into a circular, global, decision-making tool?
Senge also identified the problem with which healthcare is faced today. He stated: "System thinking is needed more than ever because for the first time in history, humankind has the capacity:
- To create far more information than anyone can absorb,
- To foster far greater interdependency than anyone can manage
- To accelerate change far faster than anyone's ability to keep pace.
Undermining Confidence
Senge concludes, "Complexity can easily undermine confidence and responsibility." Confidence is undermined when the vastness of available, valuable and applicable information is such that it appears futile to the individual to try and "keep up." In healthcare, once confidence is undermined, responsibility is surrendered as providers tacitly ignore best practices, substituting experience as a decision-making guide. While experience is not without merit in medical decision making, it is not the best guide.
Any sense of healthcare provider helplessness has a solution, but it is not based on attempting to take in more and more information. Senge states, "Systems thinking is the antidote to this sense of helplessness that many feel as we enter the 'age of interdependence.'" The solution is not only to "see" the interrelatedness of disease-processes, one disease aggravating or precipitating another, but also to see the dynamic interaction between the treatments of two or more simultaneously occurring pathological processes. The solution also allows the healthcare provider to "see" how the treatment of one disease processes is required in order to augment and/or to facilitate the treatment of another.
Medical Knowledge Overload
No intellectual discipline is more illustrative of Senge's principle of undermining confidence/responsibility than is the knowledge base required to perform excellently in the delivery of healthcare. Depending upon how you count, there are between 4,000 and 7,000 medically-related journals presently being published. There are over 1,000 medically-related journal articles published each day.
In 2004, the Journal of the Medical Library Association published an article entitled, "How Much Effort is needed to keep up with the literature relevant to primary care?" Here are the authors' conclusions:
- There are 341 currently active journals which are relevant to primary care.
- These journals publish approximately 7,287 articles monthly.
- It would take physicians trained in epidemiology an estimated 627.5 hours per month to read and evaluate these articles. That translates into 21 hours a day, seven days a week, every month.
In 1997, The British Medical Journal stated that there are over 10,000,000 medically-related articles on library shelves of which about 1/3rd are indexed in the Medline database compiled by the National Library of Medicine. If a healthcare provider receives only an average of 8 journals, including those which are free, it can be seen how overwhelming the problem of information is.
This is the level of the problem for individual physicians, but what about collaborative efforts to organize medical data? The Cochrane Collaboration was started in 1992 following Dr. Archie Cochrane's 1979 statement in which he opined "It is surely a great criticism of our profession that we have not organized a critical summary, by specialty or subspecialty, adapted periodically, of all relevant randomized controlled trials."
There are now fifteen Cochrane Centers around the world with 1,098 complete reviews and 866 protocols (reviews in progress). It is estimated that it will take 30 years to complete reviews on random-controlled studies (RCTs) in all fields of medicine which presently exist. At the end of those 30 years, nothing would have been done on the RCTs which will have been completed in the intervening 30 years.
Without medical knowledge, quality-of-care initiatives will falter, but the volume of medical knowledge is so vast that it can overwhelm healthcare providers. Stated a different way, the good news about healthcare today is the state of our current knowledge; it is excellent. The bad news is the form in which that knowledge is stored and/or accessed. The solution is "a shift of mind."
METANOIA - A Shift of Mind
In The Fifth Discipline, Senge comments about the Greek term Metanoia:
"The most accurate word in Western culture to describe what happens in a learning organization is one that hasn't had much currency for the past several hundred years...The word is 'metanoia' and it means s shift of mind...For the Greeks, it meant a fundamental shift or change...
"To grasp the meaning of 'metanoia' is to grasp the deeper meaning of 'learning,' for learning also involves a fundamental shift or movement of mind. Learning has come to be synonymous with 'taking in information.'...Yet, taking in information is only distantly related to real learning."
Change is not easy. It often creates anxiety and insecurity, even and maybe especially among healthcare providers. However, to create excellence in healthcare, which is more of a process than it is a characteristic of a product, providers must continually be "learning.," which will require a change in the understanding of the nature of learning and will also require the elimination of barriers to learning. To sustain the learning process created by this "shift of mind" healthcare providers need tools which facilitate change rather than processes which support the status quo.
Learning Disabilities
There are a number of "learning disabilities," which afflict organizations which attempt to make this shift. As an organization attempts to learn from experience and attempts to analyze that experience, these disabilities prevent an organization or an individual from making the changes which would make a difference in outcomes and in effectiveness.
Fixation on Events
"Fixation of events" is a learning disability which results because we become mesmerized with things which occur rather than looking at their cause. Events occur suddenly and demand our attention, while the processes which provide the leverage for effecting change are subtle and occur slowly over time. In a biological system, such as the human body, this is also true. The primary threat is not the heart attack but the weight gain, the inactivity, the cigarette smoking, and the cholesterol, all of which produce the heart attack. Linear thinking focuses on the event and not the long-standing problems which resulted in the event.
A patient has a heart attack. Linear thinking results in the placing of a stent and the treatment of irregular heart beats. Circular thinking and what we shall examine later - complex circularity - addresses the blood sugar, the weight, the tobacco, the waist size, the cholesterol, the stress, the inactivity, etc. Linear thinking is valuable but it must be followed up by the global evaluation of the patient. Because the slow processes do not demand our attention, it is easy to neglect them unless something requires us to focus upon them.
In effecting a change in thinking in healthcare delivery, EMR allows the:
- Capturing and processing of data focusing on the slow processes,
- Auditing of efforts to change those slow processes and
- Measuring of the effectiveness of those efforts over time.
- Evaluation of the quality of his/her care by the provider at the point and time of care.
However, unless that display of data is integrated across an entire biological entity, the change itself will be imprisoned by a linearity of thinking which obscures the dynamic interaction of all systems of the biological entity.
The Parable of the Boiled Frog
A corollary to this mental barrier to learning is "The Parable of the Boiled Frog." "Learning to see slow, gradual processes requires slowing down our frenetic pace and paying attention to the subtle as well as the dramatic." The slowly boiled frog does not react to the slowing heating water because the frog does not become uncomfortable until the damage has already been done.
The slow "boiling" which comes from the deterioration of health requires a new methodology for effecting change in patient and provider behavior. Part of that will be achieved by enhancing the capability of a healthcare provider to create discomfort in the patient in order to effect change which will benefit the patient in the long run. Part of that will be achieved by the creation of discomfort in the provider via self-auditing at the point of care which allows the provider to measure his/her performance against an accepted standard.
Because the processes which ultimately destroy health are mostly painless and are invisible, effective intervention requires making the effect of those processes apparent. Data display, which is longitudinal and comparative, can create discomfort in the patient and provider, which discomfort can contribute to change.
The Delusion of Learning from Experience
This disability also results from the slow change in systems, particularly biological systems, which make it impossible to associate personal experience with effective treatment. Healthcare strategies based on personal observation will by their nature be inadequate as the consequences are seen long after the intervention. One of the problems with learning from experience is that it results not only in very slow change in patients but it also results in reluctance or neglect by providers to make changes which will benefit patients.
"Treatment inertia" is defined as "lack of treatment intensification in a patient not at evidence-based goals for care." (Advances in Patient Safety, Vol 2, Patrick J O'Connor) The causes of treatment inertia are these "learning disabilities" which prevent a healthcare organization from adopting a learning culture. The shift of mind which is fundamental to learning - more even than memorizing new information - requires focusing upon the slow processes which cause deterioration in biological systems and it also requires the willingness to subject personal experience to the critique of evidenced-based care. This shift of mind is at the core of systems thinking.
Patterns of Change Rather than Static Snapshots
In summarizing systems thinking, Senge almost seems to have healthcare in mind. He describes systems thinking as, "A discipline of seeing wholes...a framework for seeing interrelationships rather than things and patterns of change rather than static 'snapshots.'" Historically, medical records have been snapshots of a patient's condition without any connection between the past and the future. EMR has changed that, or at least EMR has the potential of making that changing. With the cumulative data capacity of EMR, which provides a longitudinal portrait of the patient, patterns of change can be viewed seasonally and progressively.
The application of these concepts to medicine provides an elegant framework with which to study the design of the tools used to effect change in behavior of patients and physicians, and to shift the focus from information and experience to evidenced-based outcomes and data analysis over time. The shift of mind requires that the patient be seen as a whole.
If the patient's surgery is a success, it makes no difference if the patient dies; it makes no difference if the patient's kidneys are in great condition but the patient dies of a heart attack. Health initiatives must be global for the preservation of the life and well-being of the person. The "interrelations" of disease processes and disease causation and the patterns of change required to regain or retain health are pivotal concepts in healthcare.
Designing the Tools Needed When the Shift Takes Place
The final systems-thinking concept which will help design an EMR which will facilitate active learning, avoid learning disabilities and result in dynamic data management and which will change physician and patient behavior is the concept of "complexity.".
Remember, The Fifth Discipline was written to effect change in corporations and business, but the principles apply eloquently to healthcare delivery and even to the behavior of biological systems. Systems thinking requires the analysis of complex problems. Most analysis focuses upon multiple variables and a plethora of data. This is "detail complexity." However, the greatest opportunity for effecting change in an organization or an organism is in what Senge calls "dynamic complexity."
"Dynamic Complexity" occurs when "cause and effect are subtle, and where the effects over time of interventions are not obvious." The applications to medical research design are intriguing but beyond this discussion, but whether in corporations or medicine, "the real leverage in most management situations lies in understanding dynamic complexity."
To design a healthcare delivery tool which facilitates excellence will require a system which approaches healthcare from this vantage point. Display of data can obscure effective management if all it does is present more detail while ignoring, or further obscuring, the dynamic interaction of one part of a biological system with another. The circle describes a biological system much more effectively than a straight line. Yet, most medical data is displayed in a linear fashion. The difference is critical.
Seeing Circles of Causality
"Reality is made up of circles, but we see straight lines...Western languages...are biased toward a linear view. If we want to see system-wide interrelationships, we need a language of interrelationships, a language of circles." (The Fifth Disciple)
It is here that we see the application of The Fifth Discipline to medical information technology most clearly. The following concepts derive from Senge's systems principles:
- Healthcare delivery is not improved simply by the providing of more information to the healthcare provider at the point of care.
- Healthcare delivery is improved when the organization of that information is such that there is a dynamic interaction between the provider, the patient, the consultant and all other members of the healthcare equation, as well as the simultaneous integration of that data across disease processes and across provider perspectives, i.e., specialties.
- Healthcare delivery is not necessarily improved when an algorithm for every disease process is produced and made available on a handheld, pocket-computer device but it is improved when the data and decision-making tools are structured and displayed in a fashion which dynamically change as the patient's situation and need change.
- Healthcare delivery also improves when data and information processed in one clinical setting is simultaneously available in all settings. This improvement does not only result from efficiency but from the impact the elements contained in that data set exert upon multiple aspects of a patient's health. In this way, the data reflects the dynamic within the system under analysis, which in the case of healthcare is a living organism which is constantly changing.
- Healthcare is improved when there is simultaneous evaluation of the quality of care as measured by evidenced based criteria is automatically determined at the point of and at the time of care. Healthcare is improved when the data display makes it simple for the provider to comply with the standards of care, if the evaluation demonstrates a failure to do so.
- Healthcare is also improved when data can be displayed longitudinally, demonstrating to the patient over time how their efforts have affected their global well-being. This is circular rather than linear thinking. A person begins at health. Aging and habits result in the relative lack of health. Preventive care and positive steps preserve, or restore health.
- Healthcare improvement via systems will require dynamic auditing tools which give the provider and the patient immediate feedback on the effectiveness of the care being provided and received.
If then, excellent healthcare requires healthcare organizations:
- to be "learning organizations"
- to avoid "learning disabilities"
- to think in a circular rather than a linear fashion
- to look at dynamic complexity rather than detail complexity
How would data need to be displayed to support these functions?
If health science has the capacity:
- To create far more information than anyone can absorb,
- To foster far greater interdependency than anyone can manage
- To accelerate change far faster than anyone's ability to keep pace.
How can electronic patient records and/or electronic patient management help solve these problems and make it possible for healthcare providers to remain current and fulfill their responsibility of caring for patients with the best treatments available?
First, the data organization must see the patient:
- As a whole rather than as a summary of many different parts; this requires a circular perspective of a patient's life.
- As a living organism rather than as a disease process; this requires a circular perspective of a patient's life.
Second, the data organization and management must:
- Encourage and provoke change in patient behavior.
- Encourage and provoke change in provider behavior.
- Provide feedback to the provider at the point and time of service whereby the excellence of care can be measured.
Third, the data manipulation must have:
- Multiple points of entry
- Easy and dynamic interaction between the various elements of the database
- Automatic summarizing of the patient's care as measured against evidenced-based criteria
The principles which have guided Southeast Texas Medical Associates' development of a data base which supports these requirements are:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
For more information on SETMA's approach to IT and Disease Management see additional information at www.jameslhollymd.com. Particularly of interest may be Special Services which describes our specialty clinics and a series of articles on Medical Records under the section entitled, Your Life Your Health.
Linear and Circular Causality Thinking
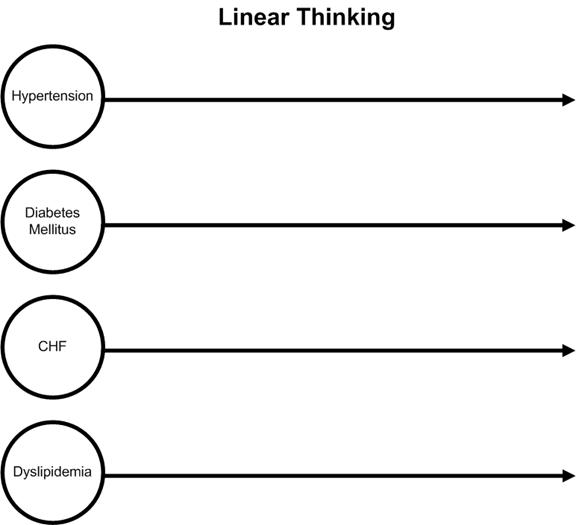
Schematically, this data organization can be contrasted with linear thinking. Thinking linearly, a healthcare provider would begin with a disease or problem and focus exclusively on that problem until it was resolved and then go to another problem. Each problem would be dealt with in isolation and without interaction between the two. In biological systems, as in business, nothing occurs in isolation. The following is a simply representation of linear thinking in medicine.
On the other hand, reality in a biological system can only be effectively approached from a circular- causality platform which is designed to encourage and facilitate the dealing with complex, interrelated problem solving for maximal effectiveness. Schematically, this would be represented as follows.
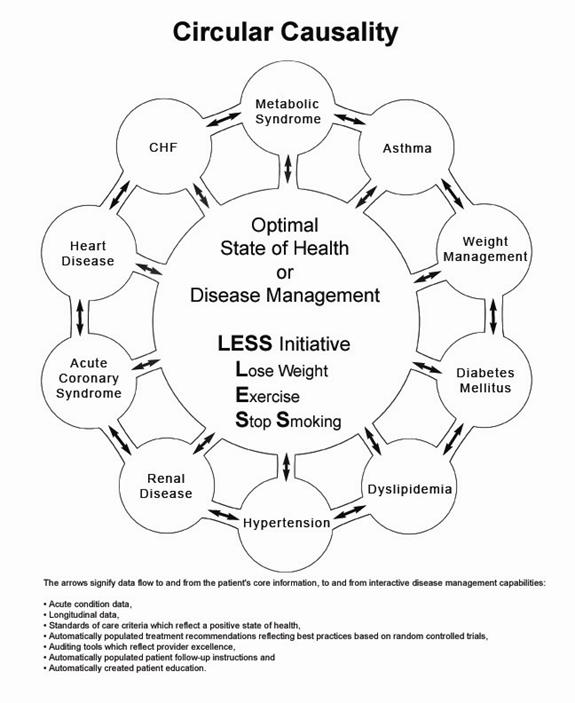
Can this be done? What would it look like? While Southeast Texas Medical Associates' EMR Data Base, which is built on NextGen's platform, is not perfect, it is a significant step forward in addressing healthcare delivery utilizing Senge's Fifth-Discipline principles.
The following materials contain in this section of our website will illustrate some of these design issues which allow integration not only across disease management boundaries but also across specialties.
|
|
|
|
|
|
|
|
|
|
|