|
Framingham Heart Study Risk Calculators Tutorial: History and Usefulness of the Framingham Calculators & SETMA’s Innovative Use of Calculators including SETMA’s “What If Scenario”
History of Framingham
In 1948, the Framingham Heart Study embarked on an ambitious project in health research to identify the common factors that contribute to cardiovascular disease by following its development over a long period of time in a large group of participants
The Framingham Heart Disease Epidemiology Study was launched to help physicians better understand heart disease. To do this, researchers examined the lives and habits of ordinary
people living in a suburban Boston town called Framingham to determine whether there was any connection between the way they lived and the health of their hearts. They investigated the risk factors that people were born with (genetic factors) and those they were exposed to (environmental factors), to see which contributed to the development of heart disease.
The researchers recruited 5,209 men and women between the ages of 30 and 62 from the town of Framingham, Massachusetts, and began the first round of extensive physical examinations and lifestyle interviews that they would later analyze for common patterns related to CVD development. Since 1948, the subjects have continued to return to the study every two years for a detailed medical history, physical examination, and laboratory tests, and in 1971, the Study enrolled a second generation - 5,124 of the original participants' adult children and their spouses
- to participate in similar examinations.
In 1994, the need to establish a new study reflecting a more diverse community of Framingham was recognized, and the first Omni cohort of the Framingham Heart Study was enrolled. In April, 2002 the Study entered a new phase, the enrollment of a third generation of participants, the grandchildren of the Original Cohort. In 2003, a second group of Omni participants was enrolled.
SETMA’s Innovative Use of the Framingham Risk
This tutorial explains the changes and use of SETMA‘s deployment of the 12 risk calculators published by the Framingham Heart Study. These tools are not absolute and must be used as an indication of potential cardiovascular and cerebrovascular risk and not as an absolute indicator of future disease. After the tutorial there is detailed information about risk factors and the Framingham.
One of the most interesting tools is the calculation of a patient’s relative heart age. It is explained below. This will be a useful tool for encouraging life-style modifications by patients but is only an indication and not an absolute assessment of heart age. If you couple SETMA’s “What If Scenario” with the Framingham and SETMA’s electronic deployment of the Transtheoretical Assessment of Stages of Change, you can have an effective means of helping patients change their behavior in a sustainable way.
The most innovative use of the Framingham Risk Calculators were suggested by SETMA‘s associates at the Diabetes Center of Excellence in Boston (SETMA is the only multi-specialty Affiliate of the Diabetes Center of Excellence). Drs. Richard Jackson and Ken Snow, while visiting SETMA, recommended the adding of a “What If Scenario” to our display of all twelve calculators.
If You Make a Change it Will Make a Difference
The concept is that we are asking patients to make changes which will not show up as benefits for decades. Of course, ignoring those changes will result in irrevocable deterioration in the patient‘s health over those decades. But how do you prove to a patient that if you make a change, it will make a difference? One way is with the Framingham Risk Calculators being presented to the patient with the inclusion of the changes which would result if the patient improved the elements of the risk calculator.
Even though these risk calculators are not perfect, they are still the best we have. And, it is imperative that patients know and that their provider knows what their risk is, because it is with the knowledge of the patient‘s cardiovascular risk that a plan of care and a treatment plan can be designed to help preserve the patient‘s health.
Remember, Risk is an attempt to determine what the future might be like which means it is imprecise. Some people with a high risk will not experience poor health and some who have low risk will. Overall, however, those with high risk will have more heart attacks and strokes than those with low risk.
Dynamic Complexity
The problem with biological systems is that change, even change which results in deterioration of your health, does not occur quickly and it often occurs without any signs or symptoms until the illness, or disease process has already caused significant damage. There is no explanation of this principle more apt to our use of risk calculators than Peter Senge‘s explanation of dynamic complexity in The Fifth Discipline.
Senge defines dynamic complexity as a situation where cause and effect are subtle, and where the effects over time of interventions are not obvious. This perfectly describes the development of many disease states and the benefit of their treatment. We know that obesity causes, or contributes to most diseases including diabetes, hypertension, heart disease, cancer, etc. In these conditions, -obesity is the cause; cancer is the effect, but the change is slow and is not apparent. Also, the results of treatment are very slow. Consequently, it is hard to sustain the changes necessary to eliminate the cause, which is obesity, in order to avoid the -effect which is cancer.
Shifting the Burden
There are structural problems which aggravate the obvious solutions to a business or a health problem; Senge addresses one of these and calls it the shifting the burden. He defines shifting the burden, as -an underlying problem generates symptoms that demand attention. But the underlying problem is difficult for people to address, either because it is obscure or costly to confront. So people shift the burden of their problem to other solutions well intentioned, easy fixes which seem extremely efficient. Unfortunately, the easier solutions‘ only ameliorate the symptoms; they leave the underlying problem unaltered. The underlying problem grows worse, unnoticed because the symptoms apparently clear up, and the system loses whatever ability it had to solve the underlying problem.
This happens in healthcare when a person looks to providers or medications to solve a problem which can only be solved by their own habits, choices, and decisions. A pill, procedure, or prescription is sought in order to overcome obesity. It will work for a short while but not long term. When it fails, more aggressive interventions are tried without addressing the fundamental problem.
The Quick Fix Deception
Senge‘s business prescription is a good one for healthcare, also. He says, “Beware the symptomatic solution...that address only the symptoms...not fundamental causes, tend to have short-term benefits at best. In the long term, the problem resurfaces and there is increased pressure for symptomatic response. Meanwhile, the capability for fundamental solutions can atrophy”. Senge adds, “The easy solution...the quick fix...solves the problem temporarily(but) a shifting of burden structure lurks behind many solutions (and) explains a wide range of behaviors where well-intentioned solutions‘ actually makes matters worse over the long term.”
Senge and Medicine
The longer a person delays addressing the -real cause of their problem, the fewer options and the fewer resources they have for dealing with the -real cause of the problem. For instance, the longer a person fails to exercise, often resulting in gaining weight and diminishing heart function, the more difficult effective solutions will be once a person determines to improve their health. If a person continues to -shift the burden of their own irresponsibility to another, expecting an artificial solution to relieve the burden created by the rejection of the real solution, they will never achieve their goal. In this case, the harder the patient pushes for solutions from a healthcare system which cannot solve their problem, for which a natural and obvious solution exists, the less benefit the patient will achieve. It is possible to ignore the real solutions - i.e., activity such as walking - until the knees and other joints have deteriorated and it is not possible to become active. In that case, more and more pressure is placed on the artificial system with less and less satisfaction with the results.
Risk Calculators: Dynamic Complexity and Shifting the Burden
These are the reasons for our using risk calculators. Because in a biological system proving the benefit of fundamental solutions by waiting for the negative consequences of poor health choices is not acceptable, we use -risk calculators to project what those poor choices will lead to. Hopefully, those risk calculators will help patients make a decision to make a change.
What If?
Because it takes SETMA only one second (really) to calculate all twelve risk calculators, we thought we were doing great. However, when we showed this function to our new colleagues from Joslin Diabetes Center, Dr. Richard Jackson commented that these scores overstate the risk and Dr. Kenneth Snow asked if we could show the patient how their risk would be affected if they make a change in their habits? Sadly, we had to admit that we could not. That was on Tuesday November 30, 2010.
We realized that while the patient has to know their risk, to understand dynamic complexity and its dangers for their ignoring their health until it is too late, and to avoid shifting the burden of responsibility from themselves to another, their healthcare providers have a responsibility to show them that if they make a change that it will make a difference.
In responding to Drs. Jackson and Snow‘s questions, SETMA built a -What-If scenario into our display of the Framingham Cardiovascular and Cerebrovascular Risk Score calculations. In the following screen shot, you will see the Risk Calculator Results for a patient with the following information:
- Age - 54
- Sex - M
- BMI - 28.6
- Weight - 210
- Height - 72
- Cholesterol - 212
- HDL - 36
- Blood Pressure - 144/98
- Diabetes - Yes
- Smoker - No
- HbA1c - 8.1
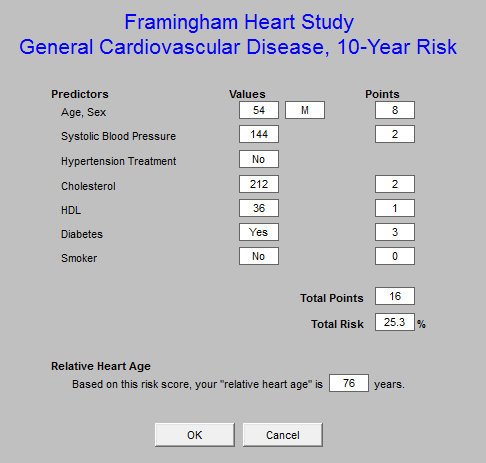
The General Cardiovascular Disease 10-Year risk
This score projects the probability of a person having a major cardiovascular event such as a heart attack or stroke in the next ten years. The above patient‘s real heart age is 54 years but the relative heart age is 76 years (his health is deteriorating more rapidly than he is aging), and the 10 year risk is high at 25.3%. These are very discouraging number for a 45 year old man. But now that we have added the -What If? section, we can assure this man that if he will make a change, it will make a difference. In addition, the greatest opportunity for improvement in his risk is indicated by the change in risk with each of the scenarios below.
- If he changes all of the elements in this calculation which are changeable (systolic blood pressure, cholesterol, smoking, hypertension treatment), his risk will improve. The unchangeable features are age, gender and diabetes.
- If he changes all of the elements to -evidenced-based goals, his risk will drop to 9.4% and his -relative heart age will drop from 80 to 54. These are dramatic improvements in his risk. We can categorically assure him that -if he makes a change, it will make a difference.
- If he changes all of the elements by a 20% improvement, his risk will drop to 15.6% and his -relative heart age will drop to 64. Obviously these are not as good as the result of treating him to goal, but they are significantly improved.
- The changes for treating his blood pressure to goal without affecting the other elements shows a drop in risk as does changing the cholesterol. There is no improvement for smoking cessation in that it is noted that this patient does not smoke.
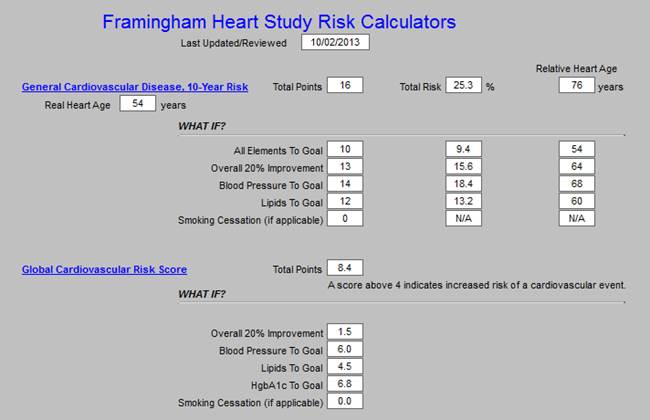
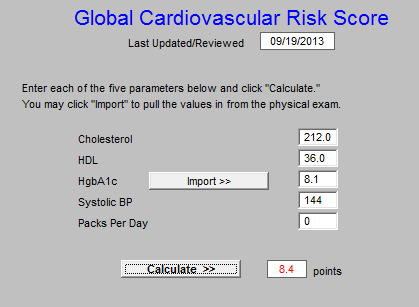
The second risk score is the Global Cardiovascular Risk Score, which is technically not a Framingham Calculator, bit which was derived from the Framingham Data. It was developed in order to eliminate the unchangeable features such as gender and age which are so heavily weighted in the Framingham Calculators so that many young people with significant risk are overlooked and many elderly people with lower risk are still rated at a very high risk. In addition, while others of the calculators take into consideration whether the patient has diabetes or not, as diabetes is an independent risk factor for heart disease, the Global Cardiovascular Risk Score takes into account whether patients with diabetes are well controlled, or not, as is indicated by the hemoglobin A1C (HbA1c).
The elements in this score are HDL, Systolic Blood Pressure, HbA1C, packs per day smoking and total cholesterol. As can be seen, if all of these elements are treated to goal, the risk goes from 13.9 points to 0.5 points. It is possible to get some indication of the contribution of each element to the risk by seeing how the risk changes when only one of the elements is changed such as blood pressure, lipids or HbA1C. As is suggested by this review, the most important thing to control is your blood pressure.
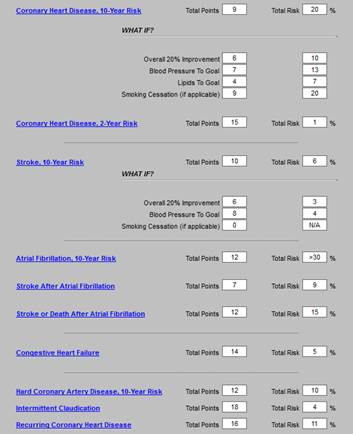
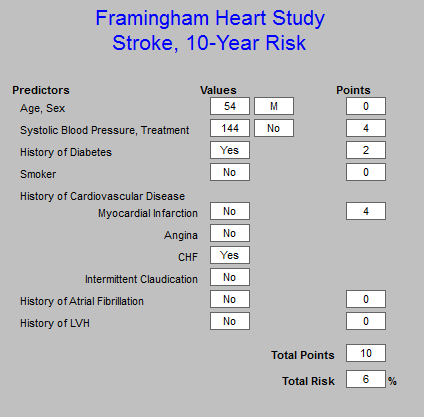
Stroke Risk - What IF?
The final calculator for which the -What If? scenarios have been calculated is -stroke risk, which is shown on the template below. The elements of this calculator are:
- Age 55-84
- Systolic blood pressure
- Diabetes mellitus
- Cigarette smoking,
- Prior cardiovascular disease (CHF, MI, Peripheral Vascular Disease, Angina)
- Atrial fibrillation
- Left ventricular hypertrophy
- Use of hypertensive medication
The current calculation of 16% risk is shown and the improvement with each scenario is displayed. Of interest is that simply controlling the blood pressure achieves almost all the possible improvement, i.e., from 16% to 5%. And, there is no difference between a -20% improvement and -a treatment to goal, demonstrating that it is not necessary to be perfect in order to achieve significant improvement; said another way, -If you make a change - even a small change -- it will make a difference.
Plan of Care and Treatment Plan
If a patient is going to make a change which will make a difference, there must be a basis on which change can be expected. We know that conversations at the time of an office visit are part of that decision to make a change. However, without a written, personalized plan of care and treatment plan, few patients will successfully make those changes and sustain them.
The -WHAT-IF? scenarios described above will be added to patients‘ diabetes, hypertension and/or lipid plans of care and treatment plans. These documents are the -batons which are passed from one member of the healthcare team - your healthcare provider - to another member of the team - the patient. If the patient will study these documents, we believe it will encourage them to make changes and it is our confidence that those changes will make a difference. With the patient‘s name and personal data in each plan, the probability of their studying the material is greatly increased.
SETMA Tutorial For Use of Framingham Risk Calculators
The SETMA Framingham Heart Risk Calculators can be found on the following Disease- Management Master Templates:
- Diabetes,
- Lipids,
- Hypertension
- CHF
- Acute Coronary Syndrome
- Chronic Stable Angina
This is an illustration taken from the Lipids Disease Management Tool:
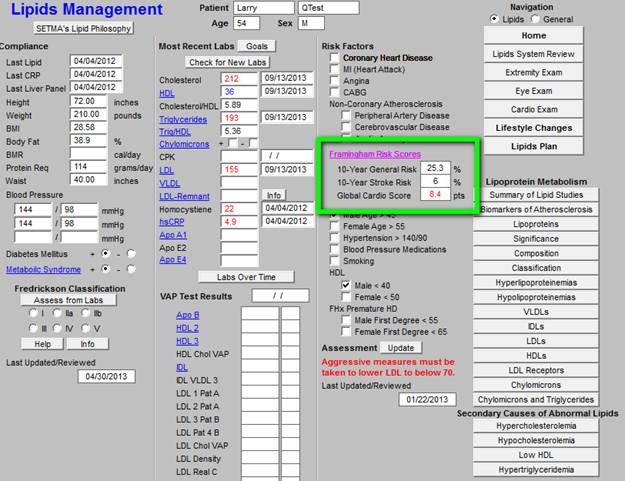
The three major Risk Score results - 10-Year General Cardiovascular Risk, 10-Year Stroke Risk and the Global Cardio Score -- are displayed on each master templates. When the button entitled Framingham Risk Scores is depressed on any of the above named master templates, the Framingham Heart Risk Calculator is launched. Without any other action on the provider‘s part, all twelve calculations are made. All data points are aggregated electronically for this purpose.
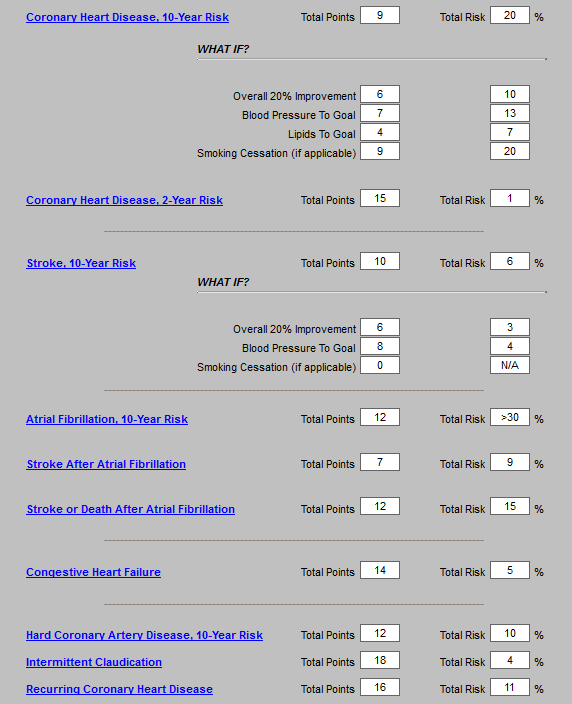
SETMA‘s deployment of the Risk Calculators (in the order of their display) includes:
- General Cardiovascular Disease, 10 Year Risk
- Global Cardiovascular Risk Score (Not a Framingham Score but built on their data)
- Coronary Heart Disease 10 Year Risk
- Coronary Heart Disease 2 Year Risk
- Stroke, Ten Year Risk
- Atrial Fibrillation, 10 Year Risk
- Stroke After Atrial Fibrillation
- Stroke or Death after Atrial Fibrillation
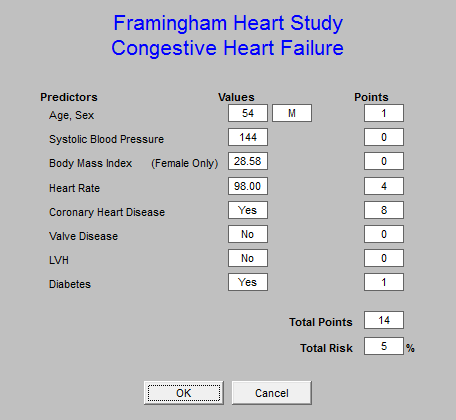
- Congestive Heart Failure
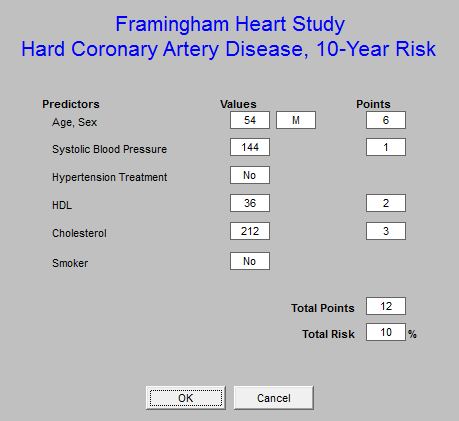
- Hard Coronary Artery Disease, 10 year Risk
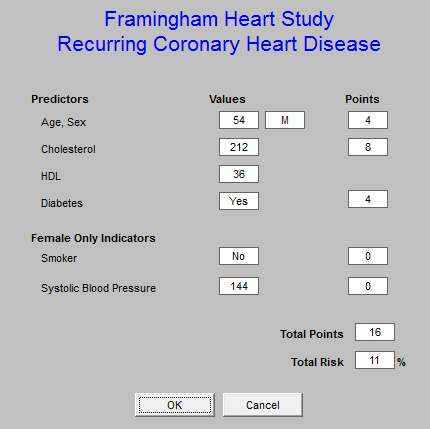
- Recurring Coronary Heart Disease
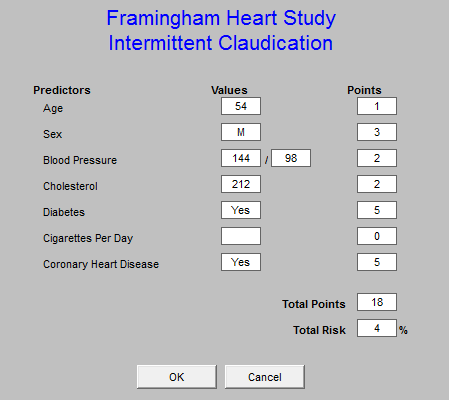
- Intermittent Claudication
The following is the template which appears when the button entitled Framingham Risk Scores is depressed. It will be noted that the titles of each of the risk calculators is in blue. This means that each is a hyperlink and when depressed the elements on the basis of which the score is calculated is displayed.
This function is a useful teaching tool, as it possible to review these elements with a patient when any score is being discussed. This will be a useful means of alerting patients to the changes they need to make in their lifestyles or treatment regimens in order to moderate their risk. The date that the Framingham Risk Scores were calculated and reviewed is noted at the top of the template.
The remainder of this tutorial will be a review of the elements of each of the risk scores with an introductory statement for each, taken from the Framingham official website at www.framinghamheartstudy.org, followed by SETMA‘s display of the risk elements when the hyperlinks above are launched.
The introductory material includes:
- Title of risk calculator
- Source from which it is taken
- Outcome which is the end-point for the risk calculation
- Duration of follow-up
- Population of interest
- Predictors
General Cardiovascular Disease (10-Year Risk)
(D'Agostino, Vasan, Pencina, Wolf, Cobain, Massaro, Kannel. 'A General Cardiovascular Risk
Profile for Use in Primary Care: The Framingham Heart Study', Circulation 2008)
Outcome -- CVD (coronary death, myocardial infarction, coronary insufficiency, angina, ischemic stroke, hemorrhagic stroke, transient ischemic attack, peripheral artery disease, heart failure)
Duration of follow-up -- Maximum of 12 years, 10-year risk prediction
Population of interest -- Individuals 30 to 74 years old and without CVD at the baseline examination
Predictors -- Age, Diabetes, Smoking, Treated and untreated Systolic Blood Pressure, Total cholesterol, HDL cholesterol, BMI replacing lipids in a simpler model.
Global Cardiovascular Risk Score
This is the only risk calculator which was not published by the Framingham Heart Study. It is a modification of the risk calculator based on the Framingham data but with the elimination of age and gender. The rationale for this was that the weight of age in the Framingham study was so great that it underestimated the cardiovascular risk in the young and overestimated it in the elderly.
The Global Cardiovascular Risk Score eliminates the age and gender bias and gives a more accurate estimate of the relative risk of al groups without regard to age. The following is the pop-up which appears when the Global Cardiovascular Risk hyperlink is launched.
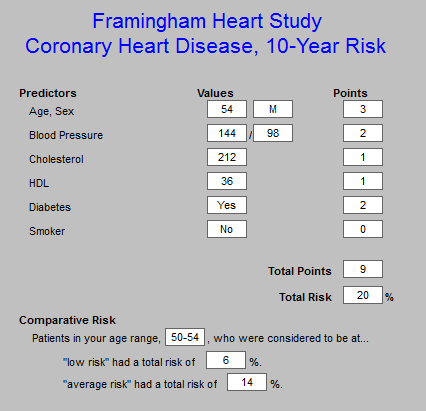
Coronary Heart Disease 10-Year Risk
(based on Wilson, D'Agostino, Levy et al. 'Prediction of Coronary Heart Disease using Risk Factor Categories', Circulation 1998)
Outcome -- Coronary Heart Disease
Duration of follow-up -- Maximum of 12 years, 10-year risk prediction
Population of interest -- Individuals 30 to 74 years old and without overt CHD at the baseline examination
Predictors - Age, Diabetes, Smoking, JNC-V blood pressure categories, NCEP total cholesterol categories, LDL cholesterol categories,
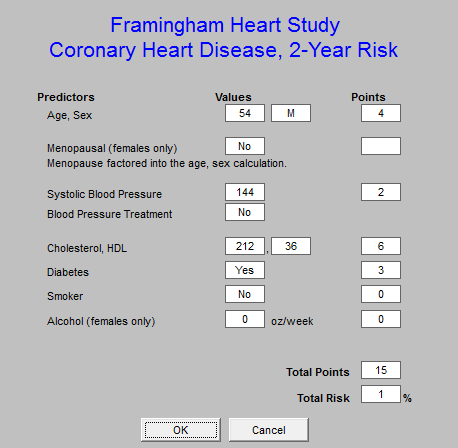
Coronary Heart Disease (2-Year Risk)
( D'Agostino, Russell MW, Huse DM et al. 'Primary and subsequent coronary risk appraisal: new results from the Framingham Study', American Heart Journal 2000)
Outcome -- First Coronary Heart Disease
Duration of follow-up -- Maximum of 4 years, 2-year risk prediction score sheets Population of interest -- Individuals free of all of the following CVDs before examination; CHD (includes myocardial infarction, coronary insufficiency, and angina pectoris); stroke (ischemic or hemorrhagic); transient ischemic attack; congestive heart failure; intermittent claudication
Predictors - Age, Systolic blood pressure (SBP), Cigarette smoking status (1 if current smoker, 0 otherwise), Fasting lipid level (totals and HDL Cholesterol), Physician diagnosis of diabetes at the current or a previous examination, Use of antihypertensive medication (yes/no),
Stroke
(D'Agostino, Wolf, Belanger, Kannel 'Stroke Risk Profile: Adjustment for Antihypertensive
Medication', Stroke 1994)
Outcome -- Stroke
Duration of follow-up -- 10 years
Population of interest -- Individuals aged 55 to 84 years, free of stroke at baseline Predictors - Age, Systolic blood pressure, Diabetes mellitus, Cigarette smoking, Prior cardiovascular disease, Atrial fibrillation, Left ventricular hypertrophy, Use of hypertensive medication
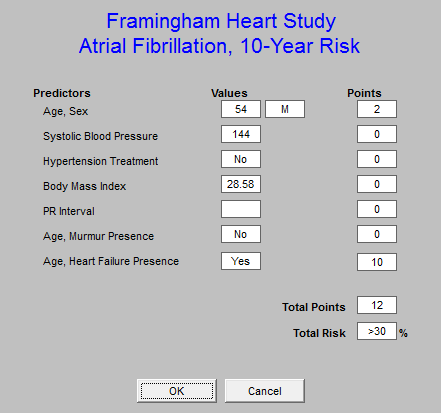
Atrial Fibrillation (AF) (10-year risk)
(Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D'Agostino RB, Sr., Newton- Cheh C, Yamamoto JF, Magnani JW, Tadros TM, Kannel WB, Wang TJ, Ellinor PT, Wolf PA, Vasan RS, Benjamin EJ. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort Lancet 2009;373:739-745.)
Outcome -- First AF
Duration of follow-up -- Maximum of 12 years, 10-year risk prediction score sheets Population of interest -- Participants free of AF at baseline, aged 45 to 95 years Predictors - Age, Male sex, Body mass index, Systolic blood pressure, Treatment for hypertension, PR interval, Significant murmur, Prevalent heart failure
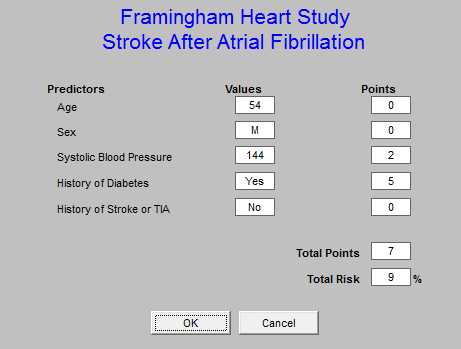
Stroke After Atrial Fibrillation
(Wang, Massaro, Levy et al. 'A Risk Score for Predicting Stroke or Death in Individuals with
New-Onset Atrial Fibrillation in the Community', JAMA 2003)
Outcome -- Stroke
Duration of follow-up -- Maximum of 10 years; mean 4 years; 5-year risk estimated Population of interest -- 705 individuals aged 55 - 94 years from the Original and Offspring Cohorts of the Framingham Heart Study meeting the following criteria: had an occurrence of new-onset Atrial Fibrillation (AF) not treated with warfarin at baseline did not have a stroke, transient ischemic attack (TIA), or death within 30 days of AF diagnosis without rheumatic mitral stenosis
Predictors - Age, Gender, Systolic blood pressure, Diabetes, Prior stroke or ischemic attack
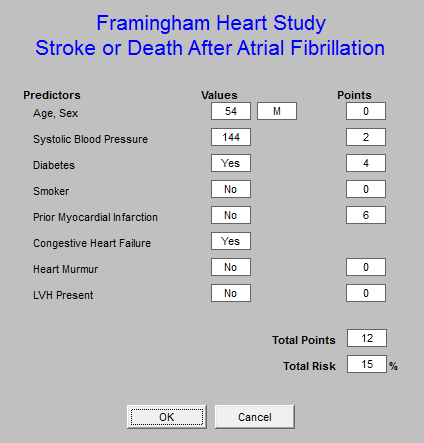
Stroke or Death After Atrial Fibrillation
(Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D'Agostino RB, Larson MG, Kannel WB, Benjamin EJ. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049-1056.)
Outcome -- Stroke or death
Duration of follow-up -- Maximum of 10 years; mean 4 years; 5-year risk estimated Population of interest -- 705 individuals aged 54 - 94 years from the Original and Offspring Cohorts meeting the following criteria: had an occurrence of new-onset Atrial Fibrillation (AF) not treated with warfarin at baseline did not have a stroke, transient ischemic attack (TIA), or death within 30 days of AF diagnosis without rheumatic mitral stenosis
Predictors - Age, Gender, Systolic blood pressure, Prior stroke or ischemic attack, Diabetes
Congestive Heart Failure
(Kannel, D'Agostino, Silbershatz, Belanger, Wilson, Levy. 'Profile for Estimating Risk of Heart
Failure' - Arch Intern. Med. 1999)
Outcome -- Congestive Heart Failure
Duration of follow-up -- Maximum of 38 years, 4-year risk prediction (pooled logistic regression)
Population of interest -- Individuals 45 to 94 years old with coronary disease, hypertension or valvular disease
Predictors - Age, Left Ventricular Hypertrophy, Heart rate, Systolic Blood Pressure, Coronary Heart Disease, Valve Disease, Diabetes, BMI, Vital Capacity (some models), Cardiomegaly (some models)
Hard Coronary Heart Disease
(The Adult Treatment Panel III, JAMA. 2001)
Outcome -- Hard coronary heart disease (HCHD) (myocardial infarction or coronary death)
Duration of follow-up -- Maximum of 12 years with risk calculated at 10 years
Population of interest -- Individuals free of CHD, intermittent claudication and diabetes, 30-79 years of age
Predictors - Age, Total cholesterol, HDL, SBP, Treatment for hypertension, Smoking status
Recurring Coronary Heart Disease
(D'Agostino, Russell MW, Huse DM et al. 'Primary and subsequent coronary risk appraisal: new results from the Framingham Study', American Heart Journal 2000)
Outcome -- Subsequent CHD (includes mostly hospitalized events consisting of myocardial infarction, coronary insufficiency, angina pectoris, and sudden and non-sudden coronary death) Duration of follow-up -- Maximum of 4 years, 2-year risk prediction
Population of interest -- Individuals who had at least one CHD event or ischemic stroke before examination and survived the acute stage of that event.
Predictors - Age, Systolic blood pressure (SBP), Cigarette smoking status (1 if current smoker,
0 otherwise), Fasting lipid level (total and HDL cholesterol), Physician diagnosis of diabetes at the current or a previous examination
Intermittent Claudication (IC)
(Murabito, D'Agostino, Silbershatz, Wilson 'Intermittent Claudication: A risk profile from the Framingham Heart Study', Circulation 1997)
Outcome -- Intermittent Claudication
Duration of follow-up -- 4-year intervals pooled for a total of 38 years
Population of interest -- Individuals free of IC at the baseline examination
Predictors - Age, Sex, Serum cholesterol, Hypertension, Cigarette smoking, Diabetes, Coronary heart disease
Important Note for SETMA’s use of the Framingham Heart Study Calculator
Left Ventricular Hypertrophy -- LVH
Because all of the data for the Framingham Risk Score calculations is aggregated from
SETMA‘s EMR data base, it is important that all of the data points be present which are required
for their accurate calculation.
LVH is the most problematical element and one of the most important. LVH leads to a fivefold to 10-fold increase in cardiovascular risk in hypertensive patients. It is usually the response to a chronic volume or pressure load. The two most important pressure overload states are systemic hypertension and aortic stenosis. The following methods can be used to determine LVH:
1. Electrocardiogram (ECG) - LVH can produce five major ECG changes: increased QRS voltage; increased QRS duration; left axis deviation; repolarization (ST-T) changes; and left atrial abnormality. The major criteria used in the ECG diagnosis of LVH are:
a. Sokolow-Lyon indices - There are two criteria with these widely used indices: Sum of S wave in V1 and R wave in V5 or V6 3.5 mV (35 mm) and/or R wave in aVL 1.1 mV (11 mm)
b. Cornell voltage criteria - These criteria are based upon echocardiographic studies designed to detect a LV mass index >132 g/m2 in men and >109 g/m2 in women.
1) For men: S in V3 plus R in aVL >2.8 mV (28 mm)
2) For women: S in V3 + R in aVL >2.0 mV (20 mm)
2. Echocardiogram - This study is needed for a comprehensive assessment of LVH in order to determine cardiovascular risk in hypertensive patients
3. Cardiac Catherization
4. Pro-BNP - the left ventricular mass can be shown to be increased when the proBNP is at or above 35 pg/ml
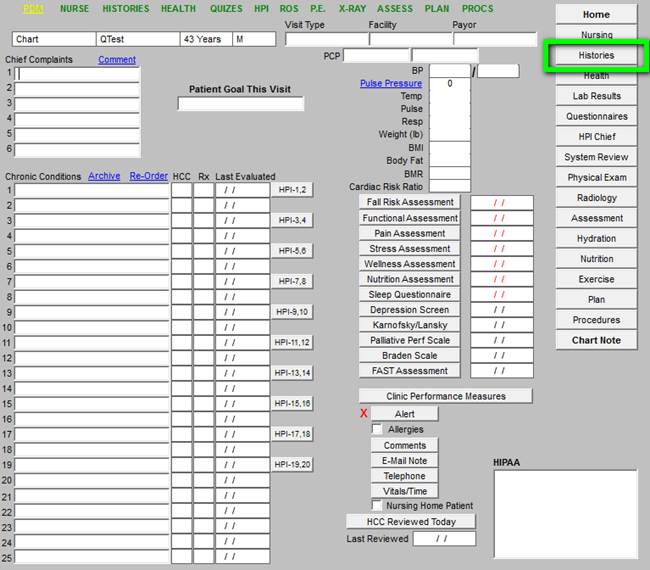
The documentation of LVH in SETMA’s data base is found on the Cardiac Historytemplate. This template can be found by the following steps:
From the Master GP Template, the Navigation Button entitled History is depressed
From the History template the Cardiac History button is depressed
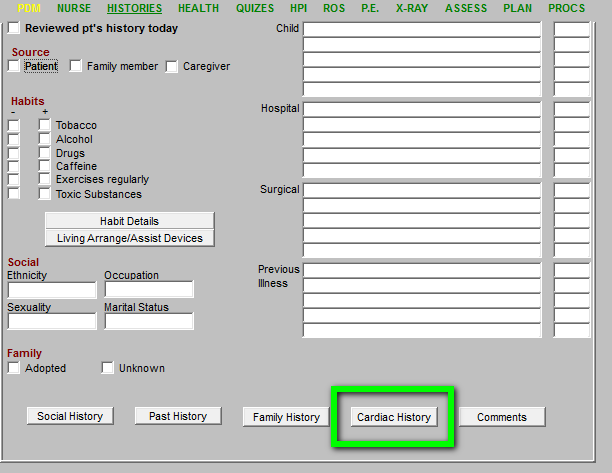
On the Cardiac History template, the documentation of the LVH is found. This is the point from which the presences or absences of LVH is determined for the Framingham Scores.
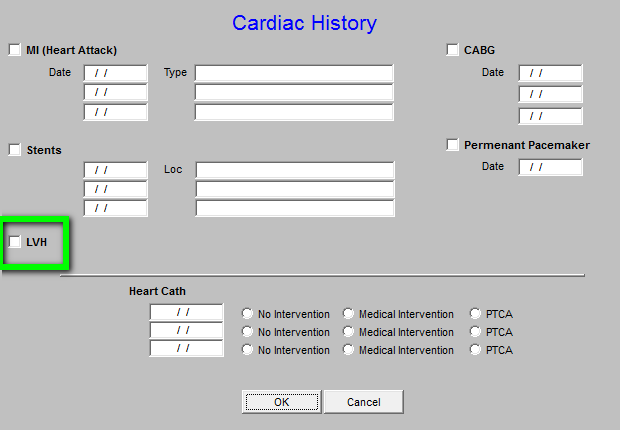
It is very important to denote whether or not your patient has LVH in order for the Framingham
Risk scores to be accurate.
The Value of Framingham Calculators
In August, 2010, the American Family Physician (reference: Global Risk of Coronary Heart Disease: Assessment and Application, Anthony J. Viera, MD, MPH and Stacey L. Seridan, MD, MPH, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, North Carolina Am Fam Physician. 2010 Aug 1;82(3):265-274) made the following observations:
-Coronary heart disease is the most common cause of death in the United States. The conventional risk factor approach to primary prevention excludes many patients who could benefit from preventive therapies. A global risk approach allows more accurate estimates of risk to guide clinical primary prevention efforts. Global risk of coronary heart disease is a calculation of the absolute risk of having a coronary heart disease event (e.g., death, myocardial infarction) over a specified period. It is based on an empiric equation that combines major risk factors, such as blood pressure and cholesterol levels. When physicians know a patient‘s global risk of coronary heart disease, they are more likely to prescribe risk-reducing therapies such as antihypertensives, statins, and aspirin. In addition, patients who know their risk level are more likely to initiate risk-reducing therapies. Many tools are available to estimate global risk, including several Web- based calculators. In the United States, tools based on the Framingham Heart Study are recommended.
Current Best Practices for Presenting Global CHD Risk Information to Patients
- Global CHD risk should be presented with comparative information for persons of the same age and sex who have no risk factors
- In addition to presenting the absolute risk as a percentage, consider presenting in other numerical formats (e.g., number of persons per 1,000 over a specific period) or picture format (e.g., number of smiley/sad faces out of 100 persons)
- Rather than categorizing risk as low, moderate, or high, a person’s risk should be placed in the context of what is considered an actionable level.
- Global CHD risk should be presented in isolation of other risks (or with emphasis on the CHD risk)
- Global CHD risk should be presented with information about controlling risk
- Global CHD risk appears to be more influential when presented by physicians (as opposed to non-physician personnel or a computer program)
Suggested Thresholds for Interventions for Primary Prevention of CHD
Absolute risk of hard CHD event over 10 years
Intervention |
≤ 5% |
6 to 10% |
> 10% |
≥ 20% |
Lifestyle modifications* |
Yes |
Yes |
Yes |
Yes |
Blood pressure-lowering medication |
Yes† |
Yes |
Yes |
Yes |
Aspirin chemoprevention‡
Statin therapy |
No
No |
Consider
Consider |
Yes
Consider |
Yes
Yes |
Smoking cessation counseling and pharmacologic aides
Any patient who smokes
Cardiovascular Disease Risk Factors
There are three categories of cardiovascular disease risk factors: major, independent risk factors;
predisposing risk factors; contributing risk factors.
The Major Independent Risk Factors
These are the risk factors which will contribute to the causation of heart disease directly and without the influence of any other condition. It is imperative to eliminate these factors either by lifestyle changes or by medication if required for control.
- Cigarette smoking - without the commitment to stopping smoking, a person CANNOT support any claim to the desire to maintain, improve, or restore their health. The first requirement to stop smoking is a decision and personal commitment to quit.
- Elevated blood pressure - remember, if you are 55 years of age, and if you DO NOT have high blood pressure, your life time risk of developing high blood pressure is 90%, if you do not take steps to avoid its development. These steps include diet, exercise, stopping smoking, etc. The first step is to have a medical examination with your blood pressure being taken properly and repetitively.
- Elevated serum total (and LDL) cholesterol - you cannot know your LDL without a blood test which must be taken while fasting. Once you know you have elevated LDL, you will require lifestyle modification - weight loss, exercise and stopping smoking - and probably will require medication.
- Low serum HDL cholesterol -- you cannot know your HDL without a blood test. Once you know that your HDL is low, you will require an exercise program and medication to raise it.
- Diabetes mellitus - if you have diabetes, you can‘t -get rid of it, but you can successfully live with it through education, discipline and excellent healthcare. It is critical that you know and remember your hemoglobin A1C number and that you
collaborate with your healthcare provider to improve it until it is consistently below 6.0.
- Advancing age - there is only one way to stop getting older and that is not acceptable to any of us. However, you can -age well by the choices you make. And, even if you have made bad choices in the past, you can reverse many of the effects of those choices with lifestyle changes and medical attention.
Predisposing risk factors
These factors work with other risk factors to produce heart disease and vascular disease. They are important but not as critical as the risk factors above. It is not possible to ignore obesity as a risk factor for heart disease but if you have o choose between losing weight and stopping smoking - stop smoking.
- Obesity - the bad news is that any level of overweight or obesity is harmful to your health. The Good news is that you don‘t have to be at your ideal body weight to improve your health. A twenty-pound weight loss can make a huge difference, even if you are greatly obese.
- Abdominal obesity - the focus of our attention on obesity must be the fat around the waist and abdomen. It is the fat cells around our abdomen which produces harmful substances which contribute to heart disease and illness.
- Physical inactivity - a sedentary lifestyle is a greater risk factor for the development of congestive heart failure than having diabetes. Most people can‘t make a decision about whether they are going to have diabetes or not, but you can make the decision to take a daily, 30-minute brisk walk.
- Family history of premature coronary heart disease - you can‘t choose your parents or grandparents, but if they have or had heart disease you can pay closer attention to your own health and the modifiable risk factors over which you do have control.
- Ethnic characteristics - as with your ancestors, you cannot choose your ethnicity, but if your race increases your risk of heart disease, you can control other factors more aggressively.
- Psychosocial factors - living a stressful lifestyle and/or not dealing with stress constructively will increase your risk of heart disease.
Conditional risk factors
These are risk factors whose significance is not totally know and/or which are not the primary focus of strategies to prevent heart disease. However, when the other factors are controlled or while they are being controlled, these factors will either be being improved or can be given sttention. All of them require specialized blood tests which are readily available. They should be part of your evaluation if you are serious about your health. Insurance will not always pay for these tests which will test your seriousness about your health as you determine how you will use your discretionary income.
- Elevated serum triglycerides - this value will be determined when your lipids are measured by your doctor. If your levels are very high, they can be improved by controlling your diabetes, or by changing your diet if you are not diabetic. Excessive, non-fibrous, simple carbohydrates contribute to elevated triglyceride levels.Small LDL particles - diet, exercise and medication can change the size of your LDL.
- It is not only the total value of your LDL which is important but the size of the particles. Small particles have a greater effect on the development of heart disease than larger LDL particles.
- Elevated serum homocysteine - this is determined by a simple blood tests and responds to treatment if it is elevated. While presently not paid for by some insurance plans, it will be some day. It is important for you to know your value and to decrease it if it is high.
- Elevated serum lipoprotein(a) -- Lp(a) is predominantly a genetic trait whose level remains more or less constant after puberty. Levels of greater than 30mg/dl have been demonstrated to independently increase the risk of CHD by six fold. Lp(a) verbalized as -Lp little a.‘ is a modified form of LDL. When both Lp(a) and LDL are elevated, the patient has a particularly high risk of developing coronary disease. Reduction of LDL and Lp(a) is associated with a reduction in clinical events and disease severity. Most of the lifestyle modifications (diet, exercise) and pharmaceutical agents known to reduce cholesterol have little or no effect on Lp(a) concentration. Fish oil-based diets have shown some ability to reduce Lp(a) levels, while niacin and N-acetylcysteine have shown (NAC), in certain studies, a pronounced ability to reduce Lp(a) levels.
- Prothrombotic factors (eg, fibrinogen) - -Prothrombotic means an increased possibility of forming blood clots. There are a number of -factors, proteins or substances in the blood which increase the risk of developing a blood clot. It must always be remembered that blood clotting or not clotting is a delicate and critical balance. If your blood cannot or will not clot, you will bleed to death; if your blood clots to readily, you will die of a heart attack or other abnormal blood clotting. Normally, this clotting/not- clotting is kept in balance naturally, but in disease processes or abnormal circumstances it is not. More people have a problem with too much clotting than with not clotting enough which is why an aspirin-a-day is recommended for diabetics and those with risk factors for heart disease. Measuring your serum fibrinogen levels, uric acid, calcium, magnesium, plasminogen activator inhibitor, d-dimer, platelet count and other tests will help your healthcare provider give you an estimate of whether you have a prothrombotic state and what you can and should do about it.
- Inflammatory markers (eg, C-reactive protein) - There are a number of inflammatory makers in the body. Heart specific C-reactive protein, which goes up naturally when you have an infection, is an emerging risk factor which may become a major independent risk factor in years to come. All of the inflammatory makers are part of the Cardiometabolic Risk Syndrome which was previously called -insulin resistance syndrome, -syndrome X or the -metabolic syndrome. Whether you have this syndrome is easy for your healthcare provider to determine with simple blood tests and a well-established equation.
The following is a partial list of patient factors which contribute to less than optimal healthcare in the United States today:
- Lifestyle - Inactivity, poor diet, overeating, smoking, excessive alcohol consumption. Much more than genetics, lifestyle often adversely affects patient health.
- Access to healthcare - There are groups of people who have limited access to healthcare. Others cannot afford the healthcare which has been recommended. Either cause decreases or even eliminates the potential health benefit of care.
- Adherence - Patient non-adherence with prescribed treatment plans is a major problem.
When patient fail to take their medications, follow-up with care as recommended or follow-through with treatment recommendations, they limit the benefit they could have received.
- Refusal - There is a difference between adherence and refusal to accept a treatment recommendation. The second most common reason for internet searches is question about healthcare. The problem is that while patients are getting more information than ever before, often that information is invalid.
- Complacen cy - The failure of patients to seek care or to follow known beneficial care. Very often patients don‘t feel badly and as a result are unwilling to engage in uncomfortable, complicated and sometimes expensive care which can interfere with their lifestyles. The problem is that most of the illnesses which can be treated successfully but which can kill you if they aren‘t, don‘t have significant symptoms until irreversible damage has been done to your body.
Boiled Frog Analogy
The boiled-frog analogy has often been used to illustrate the reluctance of people to change their behavior because they are not uncomfortable. The analogy describes a frog which is placed in a pot of cool water. The frog is comfortable and senses no danger. When the pot is placed on a stove and heat is applied, the change is so gradual that the frog is not aware of the danger until it is too late. The frog boils to death.
This is not unlike a patient who complains, -But, I was fine yesterday, why am I unable to move my left arm today? The reason is that the patient did not take their blood pressure medication and did not control their weight and did not stop smoking until it was too late. The cause of the stroke started many years before the actual event. By the way, it is NEVER -too late to begin making changes. Recent research has shown that smokers who are diagnosed with lung cancer live longer and are more comfortable if they stop smoking than are the patients who are diagnosed with lung cancer and continue to smoke. It is NEVER too late to quit smoking.
Creating Discomfort in Patients
The problem remains as to how to change patient behavior. This was a problem for providers as well. The tendency of healthcare providers not to -change, is called -treatment inertia. If is the inclination not to change things even when patients are not treated to goal. In addressing this, SETMA began publicly reporting provider performance by provider name. This created discomfort in the providers and has had a positive effect on the quality of care patients are receiving.
But, how do we make the patient uncomfortable enough that they will make and sustain changes in their lifestyles and compliance with a plan of care? One of the ways is with -risk stratification.
The calculation of a patient‘s risk of developing significant health problems and the showing of that calculation to the patient is one way SETMA attempts to encourage patients to make and sustain change. SETMA uses many tools to evaluate patient health risk. All are described on SETMA‘s website at www.jameslhollymd.com under the heading Electronic Patient Management Tools.
Two categories of risk tools are described there, under the following titles:
Preventive Heath Tools
- LESS Initiative
- Smoking Cessation
- Exercise
- Diabetic Exercise
- CHF Exercise
- Preventing Diabetes
- Preventing Hypertension
- Weight Management
Framingham Cardiovascular Risk
- Cardiometabolic Risk Assessment
- LDL Levels
- Fredrickson Classification of Dyslipidemia
- Lipid Disease Management
- Framingham Heart Study Risk Calculators
|