|
One of the most neglected areas of acute and critical care is nutrition. Also, one of the most litigated areas in long-term residential and/or nursing home care is malnutrition.
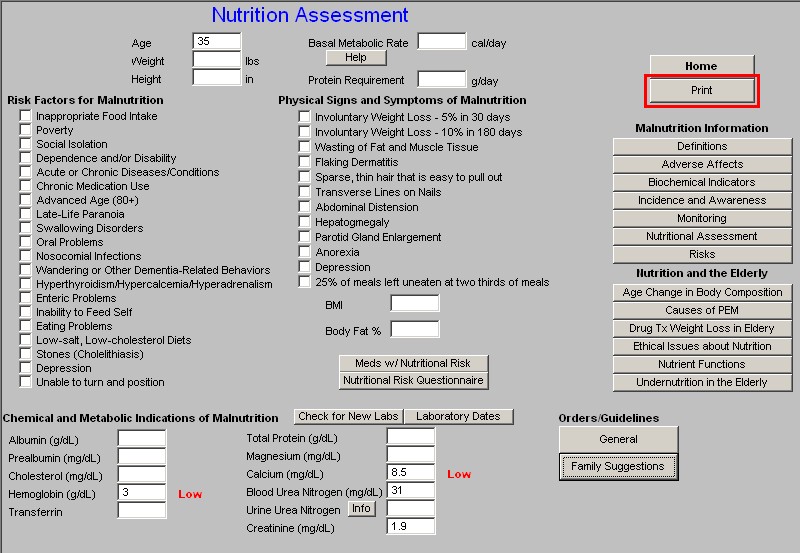
SETMA’s Nutrition Assessment Template makes it possible to objectively document a patient’s nutritional status in regard to:
- Risk Factors for Malnutrition
- Physical Signs and Symptoms of Malnutrition
- Chemical and Metabolic Indications of Malnutrition
The Nutrition Template can be launched from the:
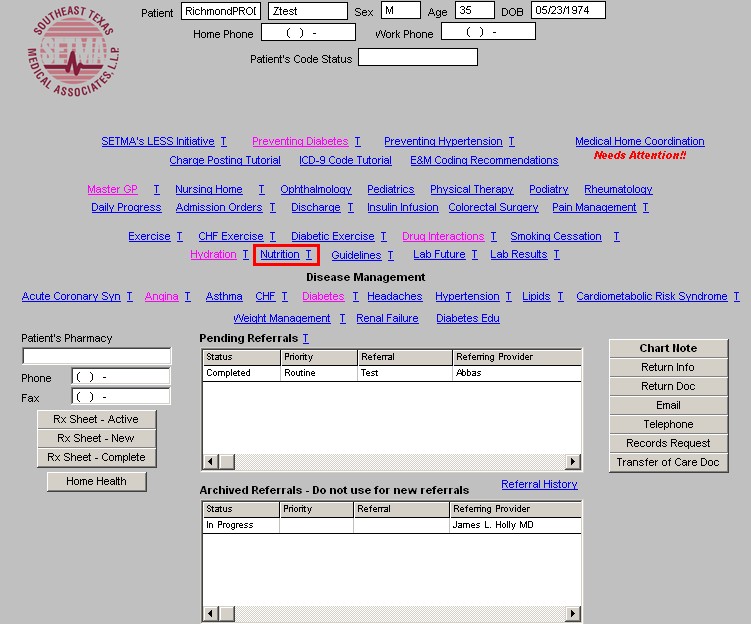
- SETMA Navigation Bar of Patient Data Master template
- SETMA Navigation Bar of Nursing Home Master template
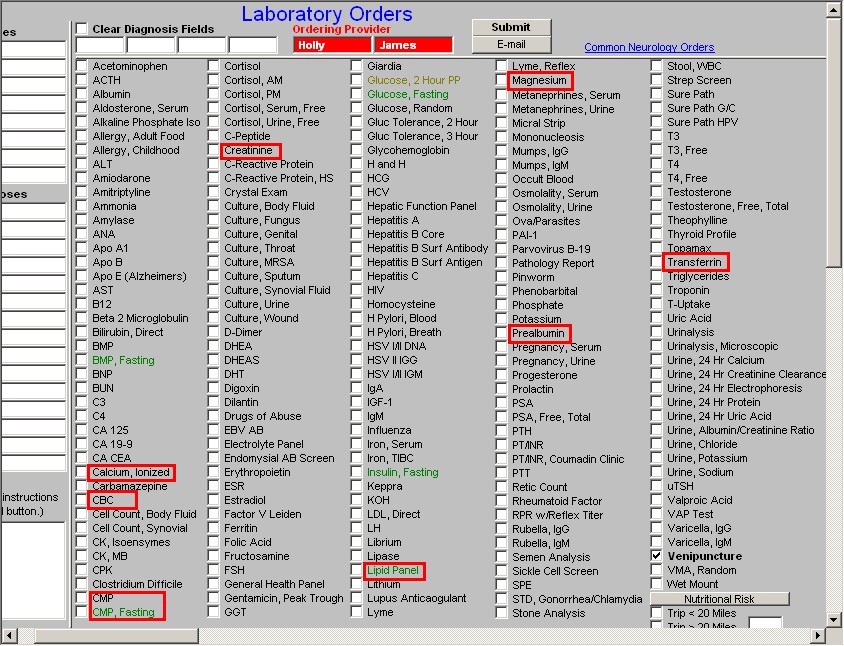
The laboratory nutritional assessment of a patient can be completed by:
- Going to the Plan Template on the GP Master Suite of Templates and
- Opening the Lab Charge Posting Template.
- At the bottom of the fifth column of that template, there is a button entitled “Nutritional Risk.”
- When clicked 8 lab studies are highlighted in blue.
- The boxes next to each of these should be clicked which will order all of the test necessary to properly evaluate the patient’s nutritional status.
- The ICD-9 Codes for Malnutrition should be used with this set of tests.
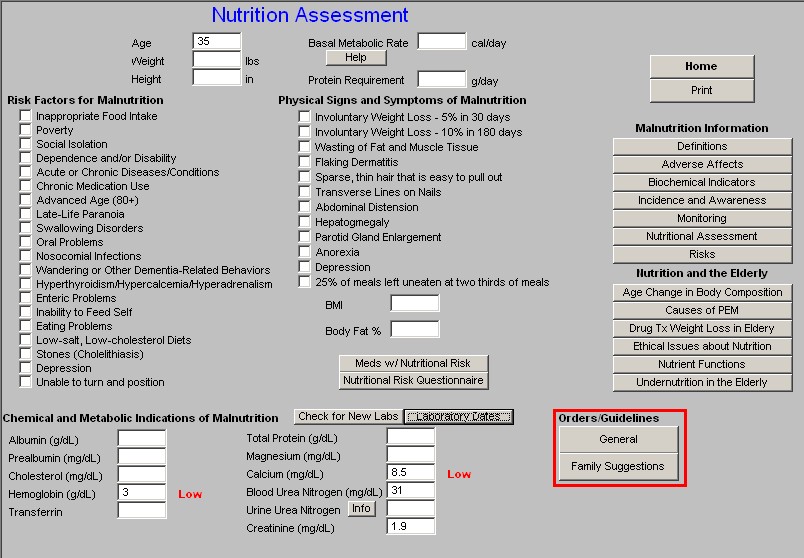
The Nutrition Template is organized into four sections from top to bottom. They are:
Top Section:
The following patient data is pulled from other parts of the EMR:
- Age
- Weight
- Height
- BMI
- Body Fat %
- Basal Metabolic Rate – there is a help button which gives details about the patient’s BMR. If the BMR is not displayed, it it is simple to go to AAA Home, click on Master GP, go the Nursing template, click in the box beside BMR, add the patient’s level of activity and click “OK.” The BMR is automatically calculated and displayed on the Nutrition Template.
- Protein Requirements – Among the very important aspects of a patient’s nutritional status is appropriate protein intake. In the first help button to the right of the Nutrition button two definitions are given:
- Workmanship – a form of malnutrition caused by inadequate protein intake
- Erasmus -- a form of failure to grow with emaciation in face of a fair appetite.
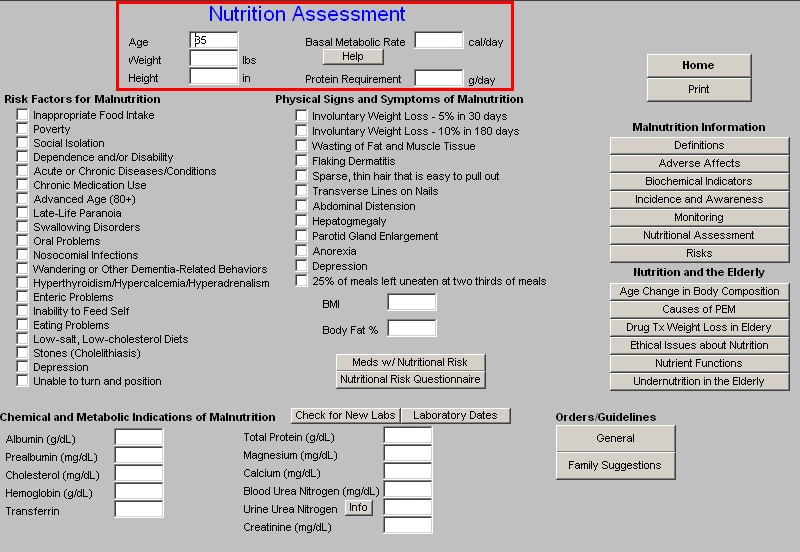
The second section of the Nutrition Assessment is composed of three columns:
Risk Factors for Malnutrition
- Inappropriate Food Intake
- Poverty
- Social isolation
- Dependence and/or Disability
- Acute of chronic Diseases/conditions
- Chronic medication use
- Advanced aged (80+)
- Late-Life Paranoia
- Swallowing Disorders
- Oral Problems
- Nonsocial Infections
- Wandering or Other Dementia-related Behaviors
- Hyperthyroidism/Hyperglycemia/Supernaturalism
- Epicenter Problems
- Inability to feed self
- Eating Problems
- Low-salt, low-cholesterol Diets
- Stones (Cholinesterase)
- Depression
- Unable to turn and position
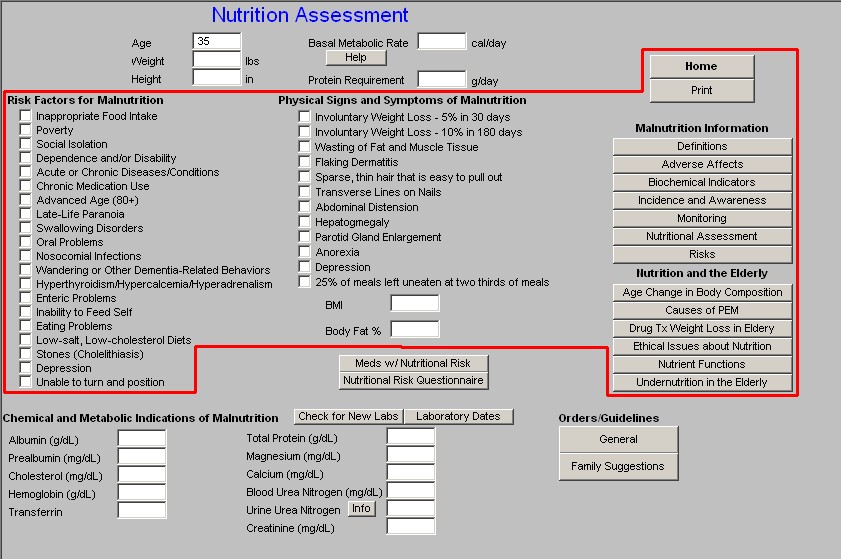
This check list not only provides an excellent risk stratification for nutritional compromise in a patient but also provides an excellent guide to evaluation of nutritional problems.
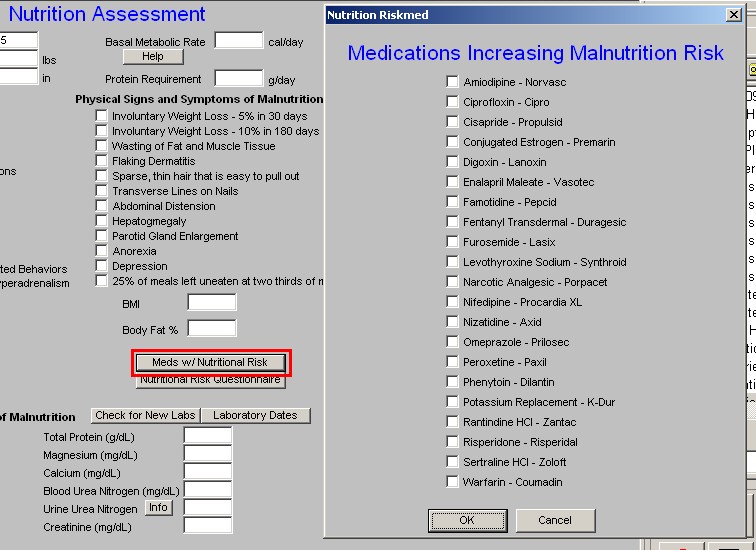
Midway down the first column and next to the Risk Factors for Malnutrition are two buttons:
Meds with Nutritional Risk – this is the list of common medications which can contribute either to decrease appetite or to decrease absorption. Any patient at nutritional risk ought to be evaluated for the possibility of avoiding these medications.
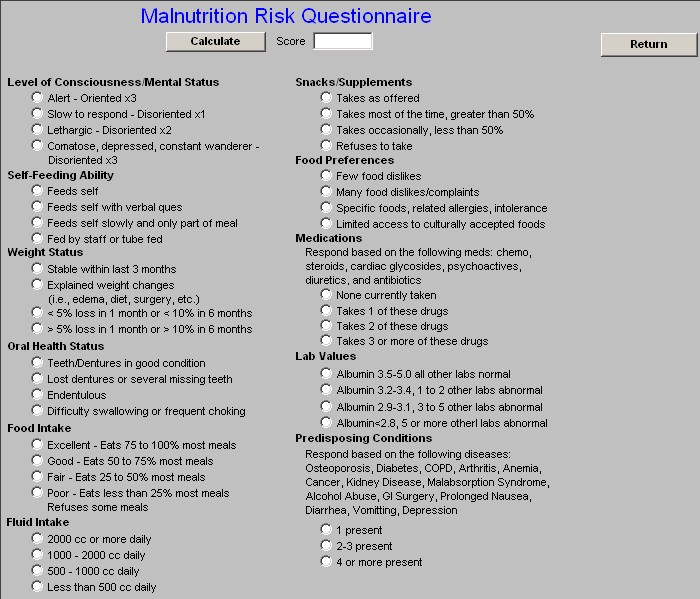
Nutritional Risk Questionnaire – based on the following categories, a score of 10 or higher places the patient at a high risk of malnutrition. The categories are:
- Level of Consciousness/Mental Status
- Self-feeding ability
- Weight Status
- Oral health status
- Food intake
- Fluid intake
- Snacks/Supplements
- Food Preferences
- Medications
- Lab Values
- Predisposing Conditions
Column 2:
Physical Signs and Symptoms of Malnutrition
- Involuntary Weight Loss – 5% in 30 days
- Involuntary Weight Loss – 10% in 180 days
- Wasting of Fat and Muscle Tissue
- Flaking Dermatitis
- Sparse, thin hair that is easy to pull out
- Transverse lines on Nails
- Abdominal distension
- Hepatomegaly
- Parotid Gland enlargement
- Anorexia
- Depression
- 25% of meals left uneaten at two thirds of meals.
Column 3:
Print Button -- this creates a document for the Nutritional Assessment Template
Malnutrition Information -- these are provider education pieces on nutrition
- Definitions
- Adverse Affects
- Biochemical Indicators
- Incidence and Awareness
- Monitoring
- Nutritional Assessment
- Risks
Nutrition and the Elderly – these are provider education pieces
- Age Change in Body Composition
- Causes of PEM
- Drug Tx Weight Loss in Elderly
- Ethical Issues about Nutrition
- Nutrient Functions
- Undernutrition in the Elderly
The third section from top to bottom is:
Chemical and Metabolic Indications of Malnutrition
- Albumin
- Prealbumin
- Cholesterol
- Transferrin
- Total Protein
- Magnesium
- Calcium
- Blood Urea Nitrogen
- Urine urea nitrogen -- there is an “info” button which explains what urine urea nitrogen is.
- Creatinine
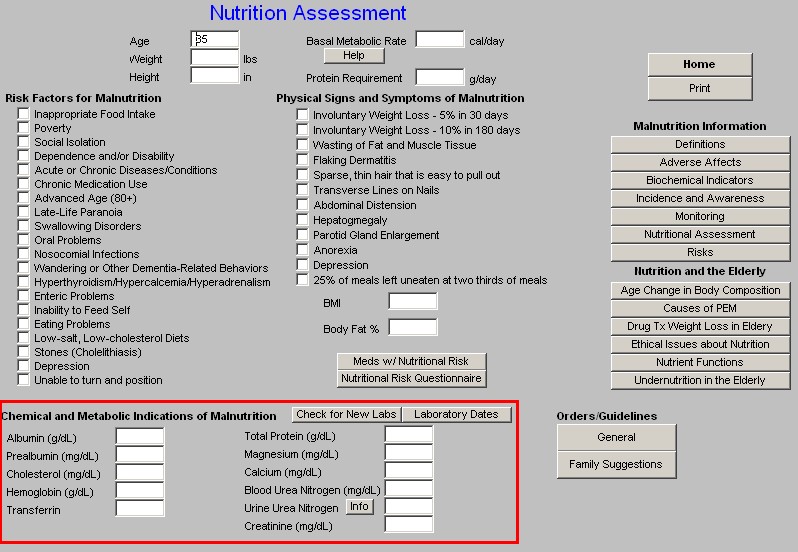
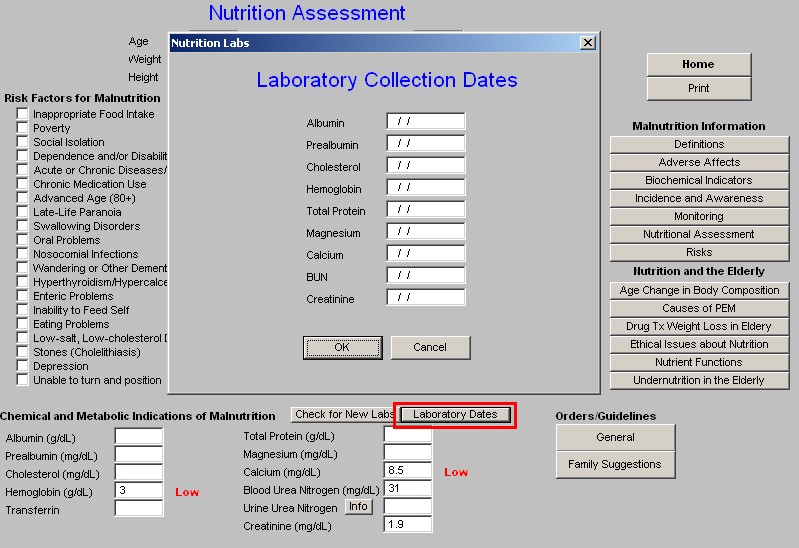
To the right of this section are two buttons:
- Check for new lab – this populates the lab results with the most current lab.
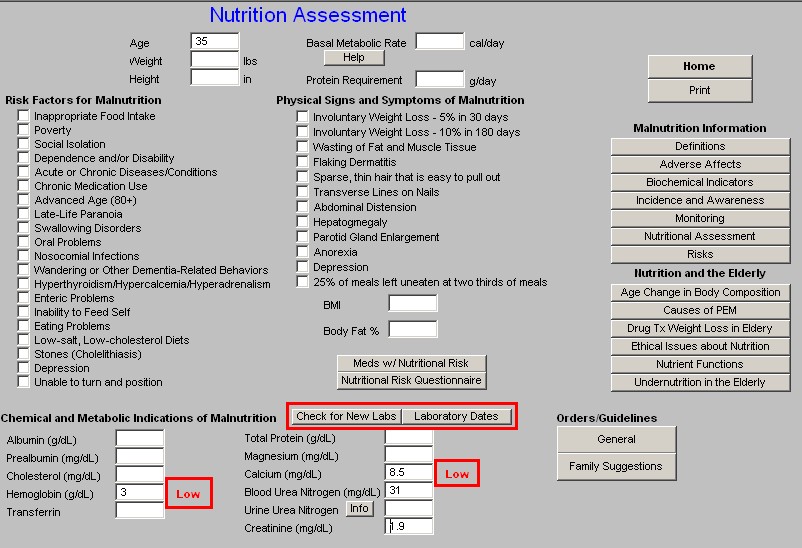
- Laboratory Dates – this tells you when the lab was done.
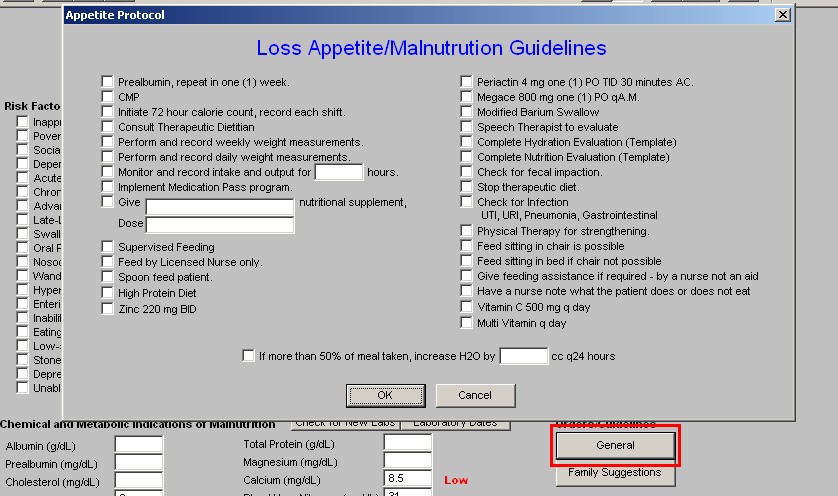
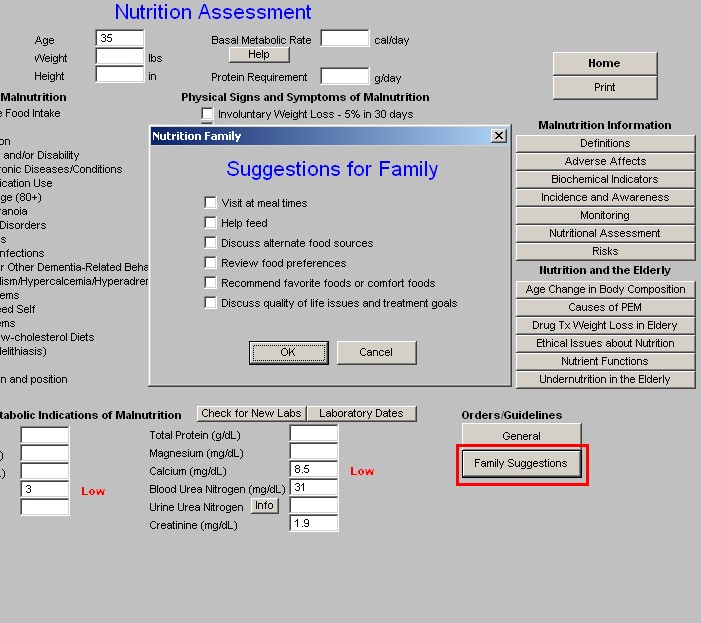
The last section from top to bottom has two buttons and is entitled “Orders/Guidelines”
General – launches a pop-up entitled Loss of Appetite/Malnutrition Guidelines
Family Suggestions – six suggestions which can be made to the family to improve the nutrition of their loved one.
The “Print” button creates a document with all of the information competed on this template. The information also is added to the document of the Master GP and the Master Nursing Home chart notes.
|