|
SETMA’s PC-MH provides twenty-four-hours-a-day, seven-days-a-week access to care for our patients. This is the first and the minimal level of safety and quality for patients’ safety and continuity of care. The second level of safety and quality is that each patient’s EHR is available at all points-of-care: clinic, providers’ homes, nursing homes, emergency departments (ED), hospitals, hospice, home health, physical therapy, etc. The EHR provides a longitudinal health record which is an increasingly granular “health portrait,” rather than the traditional static “silhouette,” or “snapshot” of a patient’s health and healthcare.
The third level of continuity and safety is that admission histories and physicals and/or emergency-department records are completed in the same data base in which all care is documented. Therefore, these episodes of care are built upon the patient’s global health record including medications, allergies, histories, laboratory and procedure results, as well as preventive health and screening health standards. And, the patient’s personal plan of care and treatment plan is always available at all points of care. The hazards of medication errors are decreased, as all medications – over-the-counter, nutraceuticals (herbal) and pharmaceuticals – are available and reconciled at all points-of-care. With every hospital-care encounter the patient receives four medication reconciliations: admission, discharge, post-hospital follow-up call the day after discharge, and provider follow-up visit from the hospital.
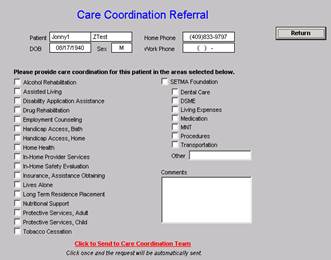
The fourth level of safety and continuity of care occurs with the multiple functions of SETMA’s Department of Care Coordination. The following is the Care Coordination Referral template. When the button displayed in “red” and entitled “Click to send to Care Coordination Team” is deployed, an e-mail is sent to the Department. The SETMA Foundation, seen in the second column, allows for SETMA providers to request financial assistance for patients who cannot afford care.
In November, 2011, in a HIMSS Leaders and Innovators Conference, the Chairman, CEO & President of AETNA said, “Convenience is the new word for quality.” Previously, SETMA established the link between “convenience” and “quality and safety,” in working through whether patient convenience is a worthy, high priority for a PC-MH. SETMA’s analysis linked the two through the following steps: “coordination” has come to mean scheduling which translates into convenience for the patient; which results in increased patient satisfaction which contributes to the patient having confidence that the healthcare provider cares personally; which increases the trust the patient has in the provider; all of which increases compliance (adherence) in obtaining healthcare services recommended; which promotes cost savings in travel, time and expense of care; which results in increased patient safety and quality of care.
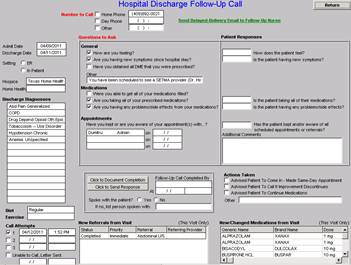
The fifth level of safety and continuity of care occurs with the post-hospital and/or post-clinic follow-up call. In SETMA’s effort to decrease preventable readmissions to the hospital, we have found two leverage points: a care-coaching follow-up call the day following hospital discharge; a follow-up by the primary care provider within five days of the discharge. The following is SETMA’s Post-Hospital Follow-up Call template. This is a 12-30 minute call, which upon occasion, with the frail-elderly, has lasted for 97 minutes, or more.
The next level of safety and quality is a clinic follow-up call which the provider can schedule at any time he/she chooses; that schedule can be two days, or two months, or any time in between or after. This additional telephone contact with the patient reinforces the treatment plan and strengthens the patient’s follow-up care. The sixth level of safety and quality is SETMA’s electronic tickler file. Follow-up care must be initiated by the practice when a patient fails to keep scheduled visits, or fails to obtain prescribed care. Through the power of electronics and the integration of Microsoft Outlook into the EHR, it is possible to create a pre-populated e-mail and delay its delivery to remind the provider to make sure the patient received scheduled care.
In one dramatic instance, a patient was seen and diagnosed with new-onset diabetes. The day following her visit, her provider explained her tests, new treatments, diabetes education, eye-care, and dental-care referrals. The patient agreed to and embraced the plan, but as the provider disconnected, he thought, “I think she is not going to follow-up”. An electronic-tickler file was created for a call three days later. On that day, an e-mail appeared in the Care Coordination queue and a follow-up call was made. The patient indicated that she appreciated the attention but was not ready to accept the fact that she has diabetes and did not intend to follow-up with the care prescribed. Continuing efforts are being made to help her accept her diagnosis and treatment. In SETMA’s Smoking Cessation Program, patients are called one month after their visit in order to follow-up cessation efforts. The follow-up clerk is reminded to make this call with an electronic tickler file which generates a pre-populated e-mail on the date the call is to be made. In addition, the previous day’s schedule of patients is audited to find patients who missed appointments for important conditions such as diabetes, hypertension, elevated cholesterol, etc. Those patients are then called to make sure they rescheduled another appointment and that they keep that appointment.
The seventh level of safety and quality is the plan-of-care and treatment plan – “the Baton” – which is discussed with the patient and family at the time of care. The personalized plan is written with the patient’s lab results and the patient’s name on each page. The plan is updated at each visit and it can be reviewed at: Medical Home Series Two: Part XII - National Quality Forum and Care Coordination. The eighth level of safety and quality is SETMA’s auditing which involves the above mentioned “missed appointments” and includes an audit of provider work flow where notices of laboratory results, procedure reports, or patient contacts are posted. The goal is “every call from every patient answered every day,” and that every laboratory result is reviewed and analyzed every day. Auditing is also done on referrals to make sure that they were completed and that the referral report was received and reviewed.
The ninth level of safety and quality is communication. Follow-up calls are initiated by the practice. And, SETMA’s HIE coordinates the sharing of information with all providers participating in the care of patients. SETMA’s secure web portal allows additional patient and provider communication. It also allows the patient to receive electronic copies of medications, lab results and treatment plans. In SETMA’s Diabetes Center of Excellence and in the entrance to all SETMA clinics, Seven Stations for Success in diabetes care are displayed in framed posters. Station 5 addresses the physician/patient collaboration, declaring:
- TOGETHER, set goals of blood glucose, blood pressure and cholesterol.
- TOGETHER, determine your risk of complications.
- TOGETHER, plan for preventing complications.
- TOGETHER, review and agree on treatment plan.
The tenth level of safety and quality is SETMA’s EHR, declared by AHRQ to be one of thirty exemplary deployments of Clinical Decision Support. Care coordination is seamless through the EHR and continuity of care is maintained by it.
Patients are involved in the care coordination process by the completion of “patient satisfaction surveys” at the end of each visit. These surveys have been collected for more than ten years and the results have been posted on our website at Public Reporting - Patient Satisfaction Survey for the past two years. The patient satisfaction survey results are publicly reported as an aggregate of each clinic and not by provider name. In 2012, SETMA is will adopt the NQF-endorsed, Clinician-Group -- Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS). Patient-satisfaction results are distributed to all healthcare providers and executive management staff.
The patient’s personal plan of care and treatment plan, along with their PC-MH Care Coordination Review document are given to the patient and reviewed with them. They are asked to continue their review at home and to bring the documents to their next visit for discussion. When serious issues are involved, the Care Coordination Department will call the patient to discuss specific patient needs. At all points of care, patient feedback is invited. With the plan of care and treatment plan, the patient is given a summary of the compliance standards and of the patient’s adherence to those standards.
The most creative care coordination and patient involvement is when the patient returns for the follow-up visit with the plan of care in hand and announces, “This information is wrong!” The creative aspect is generated by the fact that the patient is engaged in their own analysis of their care. Over 99% of the time, the information is correct, but even when it is not, we are happy to make sure that our data and that our “portrait” of our patients are correct. As the patient’s concerns are addressed, they learn and our relationship is strengthened, as is their control of their care.
A public member is on the Diabetes Self-Management Education Program oversight committee. The non-healthcare-provider member meets with the team and is invited to comment on the care given. Significant process alterations have been made through this method, particularly in what information is available to the patient through the secure web portal. Patient complaints are an important part of care coordination. When a patient files a complaint with SETMA’s staff, it is investigated by the Care Coordination Director, reviewed with the CEO and Managing Partner, and a formal and personal response is made to the patient filing the complaint. When the complaint involves a process, modifications are made to the process as appropriate.
All of SETMA’s team – nurses, nurse managers, unit clerks, healthcare providers, management and other staff – are involved in the care of patients. Feedback is given to multiple personnel about patients’ responses to their care. This information is shared via secure e-mail to all providers involved and an analysis is made as to how we can improve our communication and interaction with patients outside of the examination room.
Laser Printers
One of the most effective changes in SETMA’s processes came from simply putting a laser printer in each examination room. Because our plans of care are personalized, before the laser printers, providers had to leave the exam room to retrieve documents. Sometimes, they forgot and sometimes the patient felt that the provider was a jack-in-the-box, popping in and out of the exam room. With multiple providers using the same printer, it was a task to hunt through several documents to find your patient’s materials. After the laser printers were placed in the exam room, the provider did not have to leave the room until the visit was over and could easily give the patient their plan of care and treatment plan. This left ample time to discuss the plan of care with them in the context of the visit rather than as an “add on” in the hallway.
Tele-monitoring
One of the most effective means of engaging patients in their care is in assigning specific tasks for them to perform and then to follow-up to make sure the tasks were performed, such as, daily weights for patients with congestive heart failure; blood glucose logs for patients with diabetes; blood pressure measurements for patients with hypertension; exercise and dietary logs for inactive and/or overweight patients. Tele-monitoring of patients offers effective, real-time potential for these tasks. The deployment of methodologies for capturing this data in real-time, longitudinal and structured data fields gives the patient an indication of how important their participation is.
Best Practices – eAG versus Mean Plasma Glucose
Best Practices are identified via evidence-based literature and published and endorsed quality standards. For example, annually the American Diabetes Association publishes a monograph on the standard of care in diabetes. SETMA’s staff reads this and updates our Diabetes-Disease- Management tool with any new developments. Even when all providers do not read the monograph, new knowledge can be infused into their practice as if they had read it.
A recent improvement in our diabetes disease management tool was the adoption of the “estimated average glucose” (eAG) for Self-Monitoring of Blood Glucose (SMBG) by the patient. Previously, SETMA used the “mean plasma glucose” (MPG), but the formula for interpreting the MPG relationship to hemoglobin A1c (HbA1c) understates the severity of the patient’s risk. For instance, if a patient does his/her blood glucose monitoring and has a result of 165 mg/dl, the MPG formula would suggest that the HbA1c is 6.8%, while the eAG computation would correlate with a HbA1c of 7.5% for the same glucose value. For the MPG to correlate with a HbA1c of 7.5%, the blood glucose reading would have to be 190 mg/dl; the eAG for a glucose of 190mg/dl would correlate with a HbA1c of 8.5%. Using the MPG makes the patient think they are “doing better” than they are. Teaching the patient to use the eAG allows him/her to accurately estimate their HbA1c, which accurately reflects their cardiovascular risk.
With the patient understanding that their treatment goal is a HbA1c of 7.0%, or below, and with a glucometer result of 190 mg/dl, the patient can know that they are not at, or near their goal. With the knowledge gained from Diabetes Self Management Education (DSME) classes and refresher courses, patients are able to determine when they need to exercise more, eat less and monitor their blood glucose more carefully.
With glucometers which automatically report results to a web portal, patients will be able to see the graphic display of their blood glucose over time. This will allow patients to see if their blood glucose is always high, only high in the morning or high after meals. Each pattern will allow an adjustment of medication based on a treatment algorithm, which can be taught to the patient. Communicating through a secure web portal, it is possible to do this in real-time between visits which both enhances quality, safety and controls cost.
SETMA’s Medical Home and Care Coordination “Poster Child”
In February, 2009, SETMA saw a patient in the hospital for the first time. He was angry, hostile, bitter and depressed, and it was impossible to coax him out of his mood. When he left the hospital, he was given an appointment to the clinic. In his follow-up visit, his affect had not changed, but we discovered he was only taking four of nine medications because of expense. He could not afford gas to get the diabetes education he needed. He was disabled and could not work. He was losing his eyesight and could not afford to see an ophthalmologist. He did not know how to apply for disability. His diabetes had never been treated to goal. When he left that clinic visit, he had: an appointment to SETMA’s DSME program, with the fees waived; a gas card for the fuel to get to education classes; all medications paid for by the SETMA Foundation; assistance in applying for Social Security disability. He had a visit that day with SETMA’s ophthalmologist who arranged a referral to an experimental eye-preservation program in Houston, which is free.
Six weeks later, he returned with something which could not be prescribed for him; he had hope. He was smiling and happy. Without anti-depressants, he was no longer depressed. He now believed there was life after a ten-year diagnosis of diabetes. For the first time, his diabetes was treated to goal. Eighteen months later, he was in for a scheduled visit and he was sad. Asked why; he said that he was afraid that SETMA would get tired of helping him. He had applied for and had received disability but he would not be eligible for Medicare for two years. In two years, without care, he would be blind, in kidney failure, or dead. He asked if we would stop helping him. The answer was, “Yes, we will. Absolutely, the day after we go bankrupt.”
SETMA’s Less Initiative
In 2011, AHRQ accepted SETMA’s LESS Initiative for display on their Innovation Exchange under (Innovation Profile: Multispecialty Practice Uses Electronic Templates to Provide Customized Support at Every Visit, Contributing to Improved Patient Behaviors and Outcomes ). In 2001, after developing several disease management tools – Diabetes, Hypertension, CHF, Chronic Stable Angina, Lipids, Cardiometabolic Risk Syndrome and others – SETMA realized there were three life-style changes which were common to the treatment of all illnesses and which were important even to those who did not have chronic disease. They are: Weight Loss, Exercise, Smoking cessation; from this came the name, LESS Initiative. The LESS includes: a weight management assessment, with a BMI, BMR, protein requirement, assessment of weight class and disease risk, which was built on the AMA’s Adult Weight Management program; a personalized exercise program based on the patient’s age and gender with explanations of stretching, aerobics and strength training, which was built on the Cooper Clinic Model, and an assessment of tobacco use.
In 2002, a mother brought her five-year-old son to SETMA’s pediatric clinic and The LESS evaluation was completed on the child. When the mother returned home, she inadvertently left the LESS document on the truck seat. Shortly, the father left home to buy cigarettes and saw the document. What attracted him to it was that his son’s name was on it. The father began reading, seeing firsthand the very specific risks and damage that he was causing by exposing his son on a regular basis to secondhand smoke in the home. He sat in the truck and cried for 45-minutes. Still in the driveway, he returned to the house and discarded all the cigarettes in his possession. He hasn’t smoked since that day.
|