|
SETMA’s three partners attended the MGMA meeting in Washington DC in October, 1997. At that time, SETMA finalized the decision to adopt the electronic medical record. In March, 1998, SETMA purchased the NextGen EMR and Enterprise Practice Management System (EPM). In May, 1999, SETMA would adopt the concept of Electronic Patient Management and use the acronym (EPM) for that function.
After ten months of development, on January 26, 1999, SETMA began using the EMR in the clinic. In May, 1999, SETMA experienced four seminal events which are described in the following link: http://jameslhollymd.com/Your-Life-Your-Health/pdfs/may-1999-four-seminal-events-in-setmas-history.pdf. One of those events which guided our development was the identification of ten principles of how to develop an EMR and a 21st Century medical practice. Those principles are:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to every patient encounter what is known, not what a particular provider knows
- Make it easier to do “it” right than not to do it at all
- Continually challenge providers to improve their performance
- Infuse new knowledge and decision-making tools throughout an organization instantly
- Promote continuity of care with patient education, information and plans of care
- Enlist patients as partners and collaborators in their own health improvement
- Evaluate the care of patients and populations of patients longitudinally
- Audit provider performance based on endorsed quality measurement sets
- Integrate electronic tools in an intuitive fashion giving patients the benefit of expert knowledge about specific conditions
Charge Posting by the Provider in the Examination Room -- 2002
In May, 1999, we began building clinical decision support and disease management tools which transformed the EMR from a documentation devise into a patient management tool. By 2002, SETMA realized that the value of the electronic functions of the EMR would be enhanced if we were able to complete the entire visit in the patient examination room including:
- Encounter
- Referrals
- Medications
- Charge posting
The idea of completing charge posting in the examination room was new. The association of ICD-9 codes with CPT codes by the provider in the examination room and the submission of that documentation to our Central Billing Office for brief review and electronic transmission through a clearing house to the insurance company was a major step forward. Coupling the ICD-9 and CPT with the ordering of testing or procedures with CPT codes meant that there was no additional work for the provider. They had to order the test from a laboratory and/or procedures anyway, now we just accomplish a charge posting function at the same time. When providers became familiar with this function, it essentially added no time to the providers’ workflow.
SETMA designed the function for charge posting but initially, it was not a huge success. Because the ICD-9 Code lists were in almost incomprehensible abbreviations and because most medical practices including SETMA were using a small number of ICD-9 Codes, the attempt to do this electronically was very frustrating. In January, 2003, both our providers and our central billing office were complaining that the new process was more time consuming because many diagnoses had to be type into the EMR eliminating the value of an electronic function. Rather than giving up, SETMA decided to build our own ICD-9 tool.
To solve this problem, I asked for an ICD-9 code book to be brought to me. As I look through it, marking all of the diagnoses which I thought we needed, I finished going through the entire book in one afternoon, evening and night. The following steps were included in the building of an intuitive (easy to access), complete and accessible code list for use in charge posting:
- Going through the entire ICD-9 Code book as above.
- Dividing the code book into 20-page sections and giving each section to a different provider. They then marked all of the codes, they wanted included in an ICD-9 Code list.
- Obtaining the specialty code lists from 29 specialty groups and marking all of those codes which we would need.
Because the organization of this list had to be consistent and intuitive, the entry of these codes into our EMR had to be done by one person. It took six months to complete the task but at the end of that time, and increasingly during that time, the charge posting function in the examination room by the provider became a superior way of eliminating “coding guesses” by our CBO. Charge posting became a reality and ALL patient care functions were completed and/or ordered in the examination room before the provider completed the encounter.
Hierarchical Code Categories (HCC) and Treatment HCC Codes (RxHCC) -- 2007
The next major step in the systematizing of our coding process was the identification and displaying of the diagnoses which were HCC and RxHCC so that the provider did not have to memorize them. (for the full description see: http://jameslhollymd.com/epm-tools/Tutorial-HCC-RxHCC-Risk) One Thursday in 2007, Jon Owens, SETMA’s Chief Clinical Systems Engineer, called me and said, “I think I know how to display the HCC/RxHCC in the EMR, but I’m afraid to show it to you.” I was at home and told him to bring it to me immediately. That was Thursday, on Monday all HCC and RxHCCs were identified in SETMA’s ICD-9 Code list.
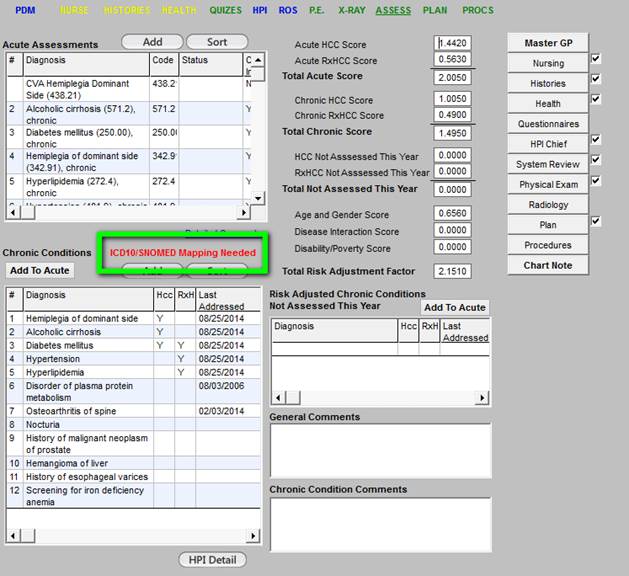
Eventually, as shown in the tutorial reference above, SETMA would display the Risk Stratification Coefficient Aggregate for the Acute Diagnosis, for the Chronic Diagnoses, for the Diagnoses which have not been evaluated that year, for the Demographic Diagnoses which includes Gender/Age, Disability/Poverty, Conditions Interaction and the Coefficient Aggregate summary for all of these. Almost all of the value-enhanced care options provided to our patients by SETMA are made possible by this work.
ICD-10 and its early effects - 2010
In 2009, it was anticipated that ICD-10 adoption would be required by 2011, but it would continue to be delayed. As news of ICD-10 continued to circulate, it was apparent to SETMA that what we had done in building our own list of 8,000 ICD-9 Codes would not be possible with the 150,000 ICD-10 Codes. In addition the complexity of the diagnostic requirements for ICD-10 would make a “home-grown” product impractical if not impossible. It was obvious we would have to adopt a commercial product. We previewed the Intelligent Medical Objects, Inc (IMO) and bought it immediately. Few times does a customer tell a vendor that their product is underpriced but that is what SETMA told IMO.
IMO had gone a step beyond SETMA in an intuitively designed ICD-9 product. One of the limitations of ICD-9 is that most codes had more than one description but our EMR did not allow assignment of the same code to different diagnoses. IMO expanded the ICD-9 code list (15,000) to almost 100,000 codes with their use of multiple names for the same code to allow for easy access through multiple descriptions.
Immediately, SETMA providers experienced the benefit of IMO and with the searching of 100,000 codes for their diagnoses, it prepared SETMA providers for the searching of 150,000 codes for ICD-10 codes. Having used IMO for over five years before making the transition to ICD-10 was a great benefit to SETMA. IMO had deployed not only ICD-9 but in the background had ICD-10 and SNOMED built into their system. This helped prepared us for October 1, 2015 and the switch to ICD-10.
Modifying SETMA’s Use of NextGen for Meaningful Use 2
In 2013, SETMA discovered that our deployment of NextGen, having been started in 1998, meant that our customized version did not qualify for the use of NextGen’s certification for Meaningful Use 2. All early adapters had this problem. Because we did not want to fall behind, SETMA determined to spend the money and to make the effort to modify our use of NextGen so we could use their EMR Certification.
This meant we had to make a number of decisions. Should we simply abandon our 15 years of customized development of clinical decision support and disease management tools and other electronic functions and start anew with NextGen’s data base which did not exist in 1998? Or, should we make the changes necessary to meeting Meaningful Use 2 standards - none of which enhanced our use of EMR -- but simply met the unique requirements of the Office of National Coordinator (ONC) for Meaningful Use 2? Should we adopt NextGen’s design of those tools or should be adapt them to our design but simply make them compatible with Meaningful Use 2 standards? The decision was not as easy as you might think.
Finally, in collaboration with NextGen and Ciscon, Inc., SETMA began this process. It took ten months and over $400,000 to make the changes, but we completed it in the early fall of 2014. The good news is that this process solved 80+% of the problems which faced SETMA in making the upgrade to ICD-10 for the many unique deployments of electronic patient management tools which we had developed. We still had work to do but this task made the remainder easier and possible.
Mapping ICD-10 Codes to ICD-9 Codes - 2014
When the upgrade of our use of NextGen was completed, the next major hurdle we faced was mapping ICD-10 to ICD-9. This means that we had to go through our entire 17-year-old data base and upgrade all ICD-9 codes to ICD-10 code descriptions. Our biggest problem had been created by the changes we made in 2003. While SETMA’s work with ICD-9 codes in 2003 had made it possible for us to complete charge posting in the examination room with an intuitively designed ICD-9 code list, it made the mapping of ICD-10 codes to ICD-9 more difficult.
Most of the mapping was done electronically. Initially, over 590,000 codes were electronically mapped, but that still left over 21,000 patient records and 41,000 diagnoses which needed to be mapped manually. The mapping process was time consuming and “back breaking” but SETMA’s entire team contributed to the effort. There were stars in the process and by March, 2015, it was done.
The following is the process which we used:
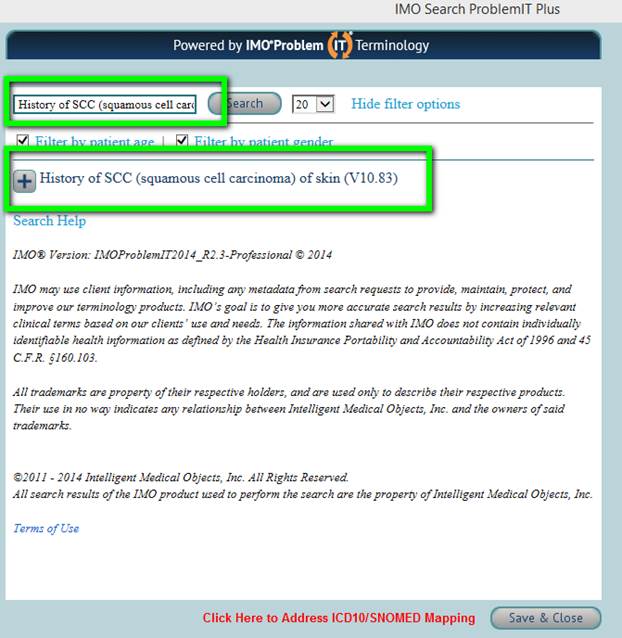
If the note “ICD10/SNOMED Mapping Needed” appeared on the Assessment template, the patient had one or more chronic problems that need to be manually mapped to ICD10/SNOMED. (see outlined in green below)
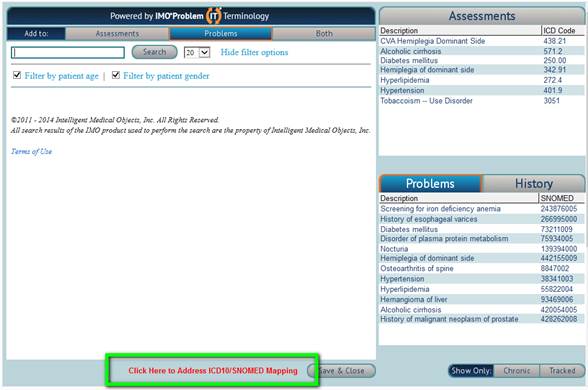
To map ICD-10, the provider would go into IMO as normal to add new diagnoses and then click on the link outlined in green entitled “Click Here to address ICD10/SNOMED mapping”. This link will only show on patients that require manual mapping.
Upon depressing the button entitled “Click Here to Address ICD10/SNOMED Mapping,” the screen below will appear. The list of diagnoses at the top are the ones that need mapping. You can see this because the grid at the top says “Not Mapped” next to the Show label.
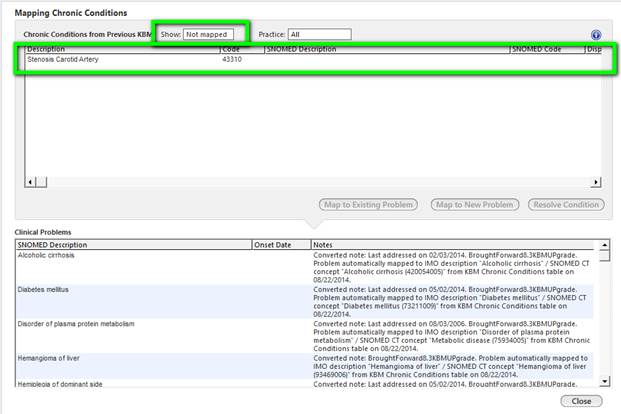
Next, highlight the diagnosis that you would like to map. Once you select a diagnosis, a button will appear below the grid that says “Map Using IMO.”
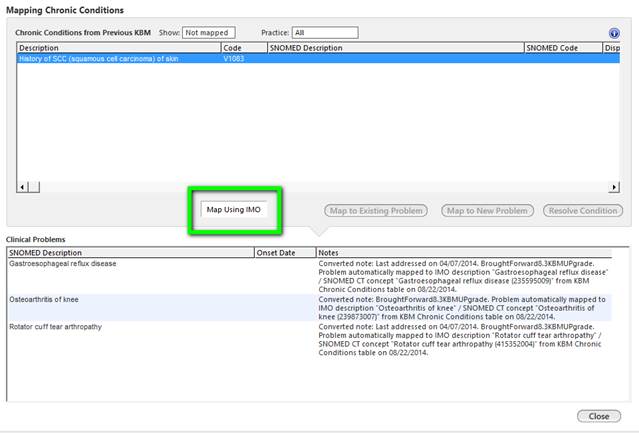
When you click the “Map Using IMO” button, a new IMO search window will appear with the text of the unmapped problem already pasted into the search window for you and, if possible, it will have already returned the results of possible matches for you.
If one of the results is the diagnosis that you want, just click the plus sign next the diagnosis and it will be mapped and updated on the patient’s problem list. Once you have click the plus sign you are done mapping the problem.
Note that you may have to modify the search text to get results or a better result for the problem you are trying to map.
By December, 2014, all charts for patients seen in the past 36 months had been mapped. We then started on the charts of patient seen between 36 months and 72 months and all of the charts for these pateints were mapped by the end of March, 2015.
Continuing Audit of Patients with Scheduled Appointments for ICD-10 Codes needed mapping
Every day, an automated audit is sent to a SETMA provider for patients who have appointments and who need to have ICD-10 Codes Mapped. Typically, there are one to five. These then have the mapping done before the pateint is seen.
SETMA’s Centeral Billing Office Continues to Test Interface,
Clearing House and Insurance Preparation
Beginning in 2014, SETMA’s CBO began testing their ability to transmit ICD-10 codes and charges through interfaces, clearing houses to insurance companys. This was done repetiively over the eighteen months before we transferred to ICD-10. Because of SETMA’s provider charge posting function, the transition for our CBO was easier. They are monitoring the progress but they do not have to go through every chart and every diagnoses to correct problems. As of today, March 5th, the CBO is experiencing no problems.
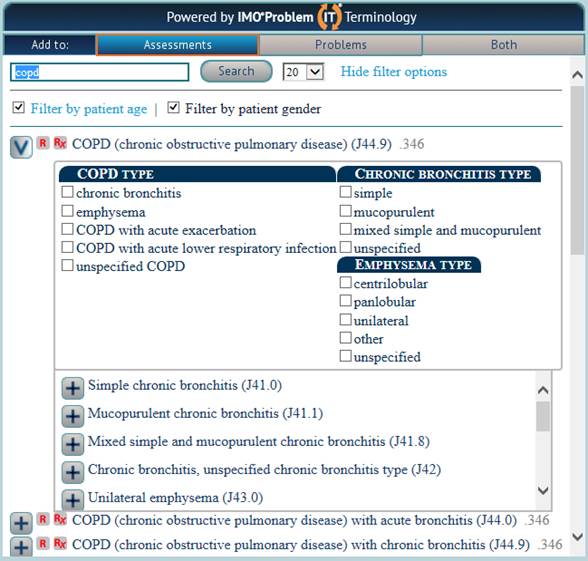
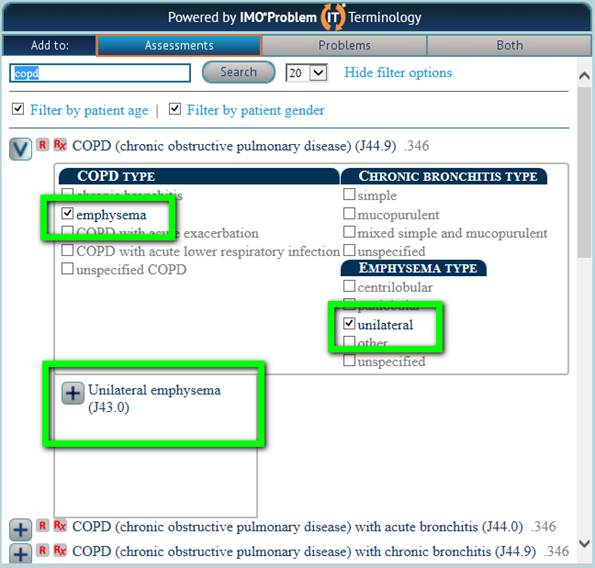
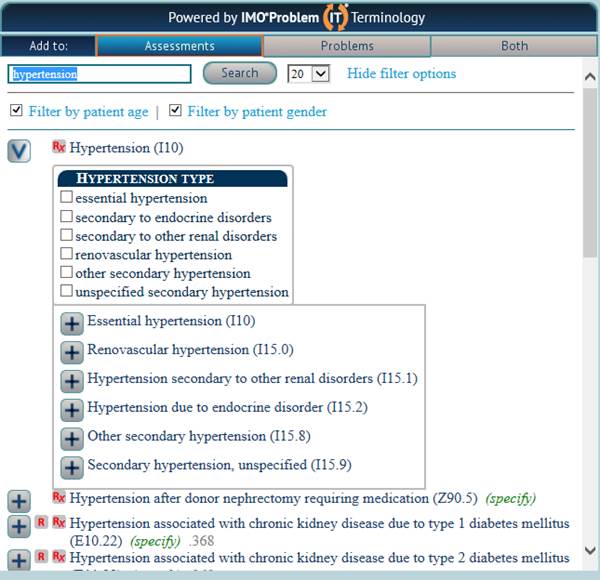
The Great Benefit of ICD-10 and IMO’s Solution
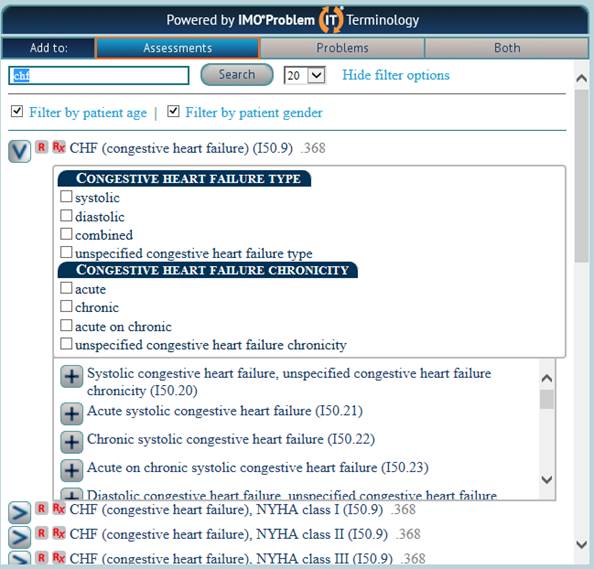
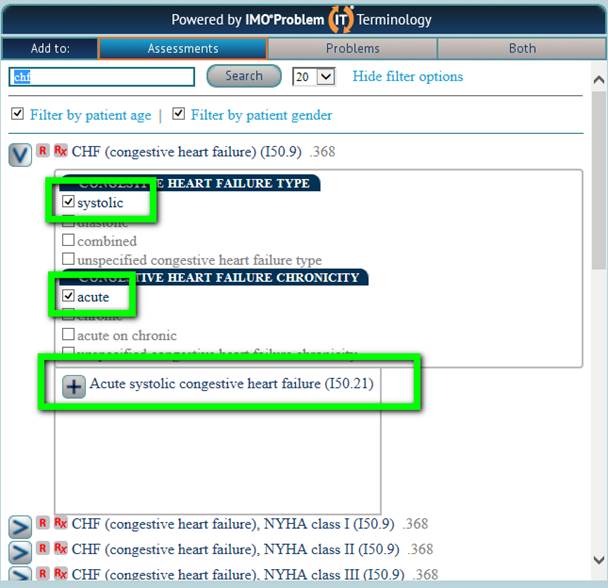
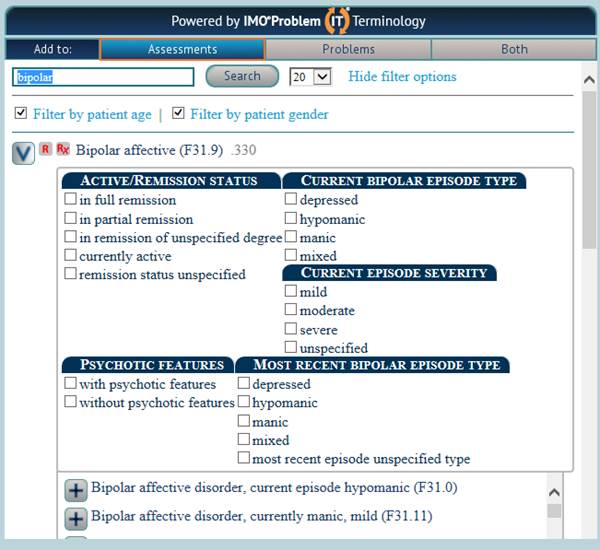
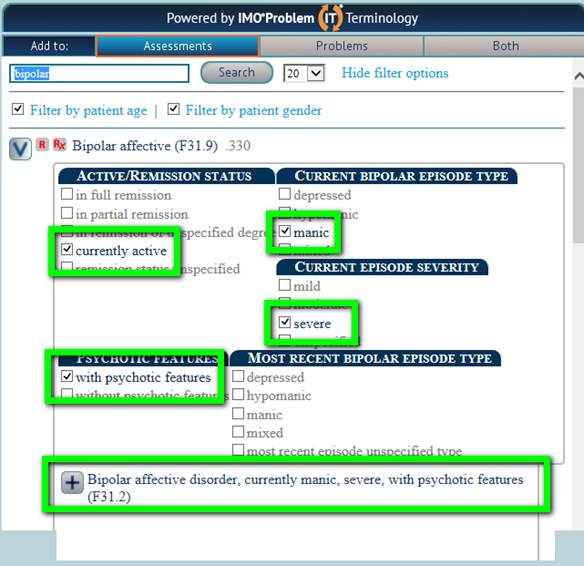
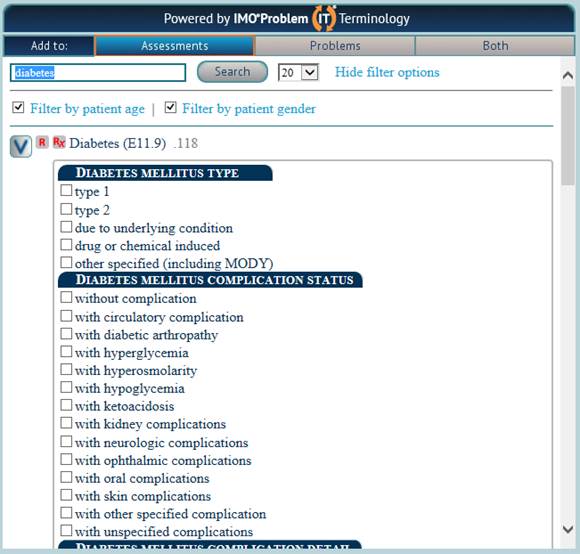
The following examples of diagnoses in the IMO solution. When a diagnoses is made and additional information is required for ICD-10, the system alerts you to what is needed and allows you, with the click of a button, to complete the task sucessfully and simply.


ICD-10 - Day 1 and following
As of 12:37 AM, October 1, 2015, SETMA was functioning with ICD-10 in all seven clinics, in all three hospitals, in all 29 nursing homes, and in every patient encounter. An explanation of ICD-10 can be quickly reviewed at the following link:
http://jameslhollymd.com/Your-Life-Your-Health/pdfs/icd-10-its-here-what-does-it-mean-and-why-does-it-matter.pdf
At 5:30 AM, Dr. Holly completed an encounter in a real patient well known to him with multiple complex diagnoses. The system works like a dream:
- When I diagnosed Diabetes Type 2 with Renal complications, the system alerted me to the need to designate specifically “renal disease,” the options appeared and with a click of a button, that was done.
- When I diagnosed Bipolar Disease, the system alerted me to the need to designate whether the patient was in full or partial remission, or not, and whether the patient was depressed or manic. With two clicks of a button, the correct ICD-10 Code was selected.
- When I diagnosed “Peripheral Neuropathy” options for mono or polyneuropathy was offered about 18 other options were presented and quickly the right choice was made.
- The diagnosis of “Hypertension” gave several options which were quickly specified.
- Moving from ICD-9 with 15,000 diagnoses and SETMA’s deployment of ICD-9 with 100,000 options created out of them, to ICD-10 with 150,000 diagnoses was simple and required only seconds of additional time.
After completing the diagnoses, I submitted the ICD-10 charges with associated CPT Codes where indicated - on a capitated patient no charges will be paid by the insurance company, The interface and the clearing house worked perfectly. As with ICD-9, all Hierarchical Conditional Codes (HCC) and Pharmaceutical HCC Codes (RxHCC) were displayed on the EMR and on the ICD-10 selection options, and they were all captured in the charge posting.
The switch to ICD-10 may cost you another 10 seconds on a complex case with multiple (4 or more) complicated diagnoses but you will like:
- The ease with which you create the specificity required for success with ICD-10
- The precision and the clarity of the diagnostic coding which appears on your chart note. The communication with other providers will be greatly improved.
- The value of all of the work which you and IT have done in the past two years to make this day simple and successful.
Soon we will be switching to SNOMED - no work required - and in several years we will make the transition to ICD-11 - again no work required and seamless updating to new versions and iterations of the ICD nomenclature.
Conclusion
You will like ICD-10 and you will be glad that we made this transition. And, it has been the case that all of SETMA’s providers and staff are pleased that we made the transition and are experiencing the benefit of this new tool.
|