|
Robert A. Berenson, MD
Institute Fellow
The Urban Institute
Dear Dr. Berenson:
I have read with interest the May, 2013 paper written by you, Dr. Pronovost and Dr. Krumholiz for the Robert Wood Johnson Foundation on Performance Measures. I have also read your February 2013 testimony before the Energy and Commerce Committee on SGR: Data, Measures and Models; Building a Future Medicare Physician Payment System. In Southeast Texas Medical Associates, LLP’s (SETMA, www.jameslhollymd.com) May Provider Training Session, I reviewed the Commonwealth Fund March 2013, Issue Brief. “Paying for Value: Replacing Medicare’s Sustainable Growth Rate Formula with Incentives to Improve Care ( by Stuart Guterman, Mark A. Zezza, and Cathy Schoen). My conclusion was that everything which the Commonwealth Fund recommended for the basis of future provider reimbursement, SETMA is currently doing. In our June training session, SETMA review your materials on Performance Measures, which I have today distributed to our providers and executive staff. These are the links to the Robert Wood Johnson Foundation sponsored paper written by you and others:
- http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf406195 Achieving the Potential of Health Care Performance Measures: Timely Analysis of Immediate health Policy Issues May 2013 Robert a Berenson, Peter J. Pronovost, and Harlan M. Krumholz
- http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf406195/subassets/rwjf406195_1 /Summary: Achieving the Potential of Health Care Performance Measures: Timely Analysis of Immediate health Policy Issues May 2013 Robert a Berenson, Peter J. Pronovost, and Harlan M. Krumholz
- http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf406195/subassets/rwjf406195_2 Policy Recommendations: Achieving the Potential of Health Care Performance Measures: Timely Analysis of Immediate health Policy Issues May 2013 Robert a Berenson, Peter J. Pronovost, and Harlan M. Krumholz
Who is SETMA?
SETMA is a medium-sized multispecialty practice in Beaumont, Texas which is about 80 miles east of Houston The attached is a presentation, I will make to IHI this Friday. The four links below are to:
- http://jameslhollymd.com/letters/Robert-Wood-Johnson-Foundation-PCT-LEAP -- SETMA’s submission to the RWJF in preparation for being selected for the LEAP Study conducted for RWJF by the MacColl Institute. This discusses SETMA’s philosophy of Quality Metrics which is also discussed below.
- http://jameslhollymd.com/the-setma-way/setma-model-of-care-pc-mh-healthcare-innovation-the-future-of-healthcare -- a discussion of SETMA’s five-point Model of Care which includes track, auditing, analyzing and public reporting over quality metrics.
- http://jameslhollymd.com/In-The-News/pdfs/Medical-Home-Feedback-Reports-SETMA-II-102011.pdf -- A summary of RTI International’s CMS’s sponsored study of 312 Medical Home Practices benchmarked against 312 non-coordinated practices. This shows SETMA II had a 37.4% lower cost than the practice against which it was benchmarked for fee-for-service beneficiaries..
- http://jameslhollymd.com/public-reporting/public-reports-by-type -- Link to SETMA’s public reporting by provider name on our website.
Performance Measures - Quality Metrics and Transformation of Healthcare
Efforts to reform healthcare may fail unless they employ four elements upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
At the core of these four principles is SETMA’s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery.
SETMA employs two definitions in this analysis:
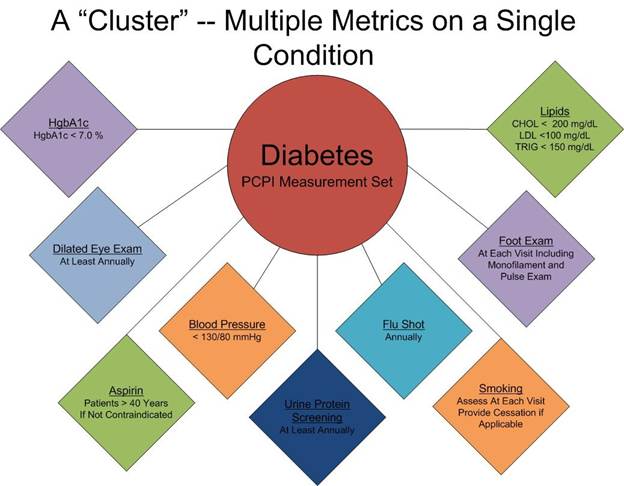
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics which are measurable at the point-of-care can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may have as many as 60 or more quality metrics fulfilled in his/her care which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And because of the improvement in care and health, the cost of that patient’s care will be decreased as well.

SETMA’s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intent of that care.
Quality Metrics Philosophy
SETMA’s approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
(I will have some additional things to say about your work about Performance Measures in subsequent notes)
The Limitations of Quality Metrics
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of the quote ascribed to Einstein, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
Technology Can Deal with Disease but Cannot Produce Health
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
Team Approach to Healthcare Delivery
The ideal setting in which to deliver and to receive healthcare is one in which all healthcare providers value the participation by all other members of the healthcare-delivery team. In fact, that is the imperative of Medical Home. Without an active team with team-consciousness and team-collegiality, Medical Home is just a name which is imposed upon the current means of caring for the needs of others. And, as we have seen in the past, the lack of a team approach at every level and in every department of medicine creates inefficiency, increased cost, potential for errors and it actually eviscerates the potential strength of the healthcare system.
Why is this? Typically, it is because healthcare providers in one discipline are trained in isolation from healthcare providers of a different discipline. Or, they are in the same buildings and often are seeing the same patients but they rarely interact. Even their medical record documentation is often done in compartmentalized paper records, which are rarely reviewed by anyone but members of their own discipline. This is where the first benefit of technology can help resolve some of this dysfunction. Electronic health records (EHR), or electronic medical records (EMR) help because everyone uses a common data base which is being built by every other member of the team regardless of discipline. While the use of EMR is not universal in academic medical centers, the growth of its use will enable the design and function of records to be more interactive between the various schools of the academic center.
And, why is that important? Principally, because more and more healthcare professionals are discovering that while their training often isolates them from other healthcare professionals, the science of their disciplines is crying for integration and communication. For instance, there was a time when physicians rarely gave much attention to the dental care of their patients, unless they had the most egregious deterioration of teeth. Today, however, in a growing number of clinical situations, such as the care of diabetes, physicians are inquiring as to whether the patient is receiving routine dental care as evidence-based medicine is indicating that the control of disease and the well-being of patients with diabetes is improved by routine dental care. Also, as the science of medicine is proving that more and more heart disease may have an infectious component, or even causation, the avoidance of gingivitis and periodontal disease have become of concern to physicians as well as dentist.
The SETMA Model of Care
- The tracking by each provider on each patient of the provider’s performance on preventive care, screening care and quality standards for acute and chronic care. SETMA’s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provide.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool “plans of care” and the medical-home- coordination document summarizes a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Permanence Improvement (QAPI) Initiatives - this year SETMA’s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a COGNOS Report which allows us to analyze our hospital care carefully.
If this work interests you, I would like to send you some of my thoughts about your recommendations for Performance Measures. I am also interested in why the Physician Consortium for Performance Improvement is not mentioned in your paper about developers of performance measures.
Sincerely yours,
Larry
James (Larry) Holly, M.D.
C.E.O. SETMA
www.jameslhollymd.com
Adjunct Professor
Family & Community Medicine
University of Texas Health Science Center
San Antonio School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
|