|
August 24,2010
Janet Corrigan, PhD
President and CEO
National Quality Forum
Dear Dr. Corrigan:
My CMO and I are registering to attend the NQF National Priorities Partnership on Care Transitions in Washington next week. I am a member of the HIMSS PS&CO committee and CEO of Southeast Texas Medical Associates, LLP, a medium size, multi-specialty practice in Beaumont, Texas. We have had experience with "care transitions" for the past 14 months and have designed a quality improvement initiative for decreasing avoidable readmissions to the hospital employing "care transitions" metrics, as well as other strategies (a preliminary description of this project is attached, entitled "Designing A Quality Initiative How? Hospital Re-admissions."
SEMTA's interest in "care transitions" resulted in our deploying PCPI's Care Transitions measurement set which was published in June, 2009. Our experience with "Care Transitions" has included the personal calling of every patient the day after they leave the hospital which is described below. Two attachments address our interest in NQF's work:
- The first is a copy of my power point presentation for a meeting in Philadelphia, August 25, 2010. It includes comments about SETMA's tracking, auditing, analyzing and public reporting at www.jameslhollymd.com of NQF's comprehensive diabetes measures. We also track numerous other NQF Endorsed Measures and have done an analysis of the seven published quality measure sets on diabetes: NCQA DRP (which SETMA was awarded), NQF, PCPI, AQA, NCQA HEDIS, Diabetes Center of Excellence (of which SEMTA is an affiliate organization), and Bridges to Excellence.
- The second attachment is an article entitled "Passing the Baton - Effective Transitions in Healthcare." The premise of this article is that if the "baton" represents the person responsible for the healthcare of an individual at any moment, in that there are 8,760 hours in a year, the patient will be carrying the "baton" of responsibility for their own healthcare for over 98% of the time. This article displays SETMA's deployment of PCPI's Care Transitions measurement set. SETMA's audit of our performance on PCPI's Care Transitions audit is posted on our website under PCPI Care Transitions. The following is a link to that posting PCPI - Care Transitions.
We also present tutorials for all of our "electronic patient management tools" on our website. The most relevant materials for the NQF conference September 1 & 2 are the tutorials for:
- Care Transitions - Found at www.jameslhollymd.com under Electronic Patient Management Tools/Hospital Based Tools/Care Transitions PCPI Data Set Tutorial. A copy of that tutorial is attached.
- Follow-up Telephone Calls - Found at www.jameslhollymd.com under Electronic Management Tools/Hospital Based Tools/Telephone Calls Follow of Hospital Care Tutorial. A copy of that tutorial is attached.
The attached article on "Passing the Baton" states in part:
. Care Transition - in June, 2009 the AMA released the "PCPI Care Transitions measurement set". Due to SETMA's having used the EMR for discharge summaries for ten years, it was apparent that with very slight modification, we were fulfilling all of these measures. We implemented this measurement set and are performing at 100%.
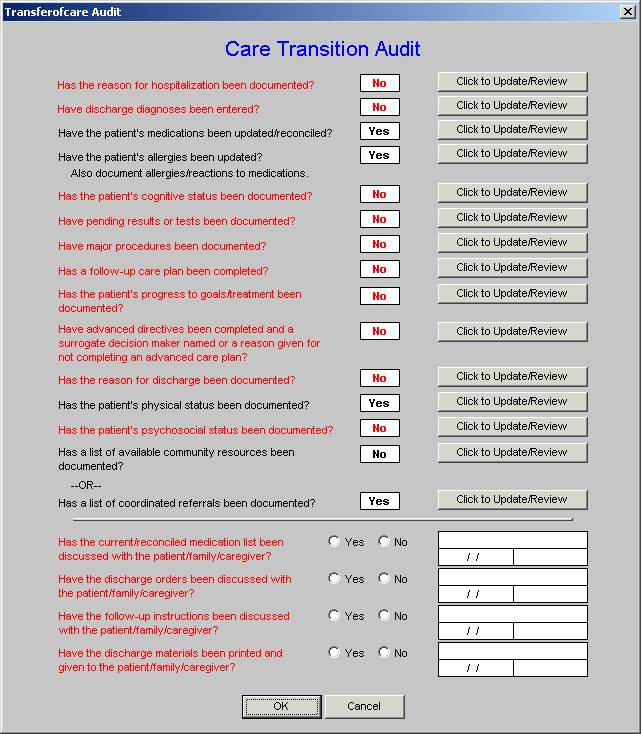
As can be seen by reviewing the 14 data points and the 4 actions required by the audit, when the elements of this audit are met and when the discharge summary and follow-up document are completed with this material and are given to the patient and/or family, almost all of the continuity of care issues are resolved. The legend is that everything in black is done and everything in red has not been done. For the elements which have not been done, the "Click to update/Review" button takes the provider back to the place in the Discharge Summary where the data point at issue should be documented.
This transition audit is one of the tools used to "build" the "baton" and then to make sure that the complete "baton" has been transferred to the next team member.
- Medication Reconciliation - it is imperative that careful medication reconciliation takes place at the end of any and every hospitalization and that a copy of the appropriate list of medications is given to the patient/family. In that SETMA completes the discharge summary in the EMR, the hospital medication reconciliation is automatically a part of the patient's outpatient record. Nevertheless, when the patient comes back to the office, a medication reconciliation is repeated each time.
- Telephone follow-up - Every patient discharged from the emergency department or inpatient status receives a telephone call the day following their discharges. Subsequent calls can be scheduled as indicated. The follow-up call addresses current condition, medications, reactions, special needs and follow-up appointments.
Since SETMA began this five months ago, it has increased patient satisfaction, patient safety and the quality of patient care. It is early yet, but we believe it will decrease our readmission rate which is already very low. "
We look forward to learning of NQF's plans in this area and contributing any of our experience which may be appropriate.
Sincerely yours,
James L. Holly, MD
CEO, SETMA, LLP
www.jameslhollymd.com
|