|
March 3, 2010
Ms. Linda M. Magno
Medicare Demonstrations Program Group
Centers for Medicare and Medicaid Services
Office of Research, Development and Information
7500 Security Boulevard
Mail Stop CA-17-27
Baltimore, MD 21244-1850
Via e-mail Linda.magno@cma.hhs.gov
Dear Ms. Magno :
Your presentation at the National Medical home Summit was helpful. If you recall, I asked you a question based on one of the points in your presentation. You said that one of the questions CMS will ask is, “What Medical Home services are delivered?” I asked for a succinct summary of what CMS would consider to be “medical home services.” The reason is that I thought the concept contain in this CMS’ question was novel. It occurred to me that in addition to the “transformation” of our practice – Southeast Texas Medical Services, LLP (SETMA, LLP. www.jameslhollymd.com) – into a Patient-Centered Medical Home, there will be discreet, identifiable services related to that process. We should be able to describe, enumerate and prove that those services are being performed on all patients in our patient-centered medical home.
In response to your answer, Ms. Magno, I asked if the fulfillment of PCPI’s Care Transition measurement set would fulfill CMS’ requirements for the transition from inpatient care to outpatient care. I promised to send you that measurement set and do so below. However, I would like to take this opportunity to go further in discussing the implications of your presentation and of my question.
On February 16, 2009, I attended a presentation by Transformed on the Patient-Centered Medical Home. At that time, I did not have any idea what that name meant, or the implications for SETMA and the people we serve. After that meeting, I was still in the dark, as at that meeting, I asked the questions, “If we are doing everything you say that a practice should be doing in order to be a medical home, and we are; and, if we are confident that we are not a medical home; what is missing?” There was no good answer to my question.
The next day, I initiated an analysis of our practice, based on the 28 CMS requirements for Medical Home certification. On March 14, 2009, SETMA completed a thorough analysis of our practice and distributed to all of our staff a 420-page summary of that analysis. entitled, “Center for Medicare and Medicaid Services’ (CMS) Twenty-eight Requirements for Medical Home Certification Documentation of Southeast Texas Medical Associates, LLP (SETMA) Fulfillment of all 28.” All of our healthcare providers, executive management staff and team members were involved in this process. On February 19, SETMA published the first of an eleven-part series on the concept, content and promise of Patient-Centered Medical Home. These articles and subsequent articles on healthcare policy and reform are posted on SETMA’s website at “Your Life Your Health” under links entitled “Medical Home” and “Healthcare Reform and Public Policy.” This material reflects the evolution of our understanding of Patient-Centered Medical Home and of our remodeling our practice to become a Patient-Centered Medical Home.
Subsequently, we reviewed NCQA’s 9 Standards, 30 Elements and 184 data points required for recognition as a patient-centered medical home. We believe that we will be prepared on April 1 to submit our application for recognition. We have posted all of the tools we have developed for Patient-Centered Medical Home including our Public Reporting of Provider Performance on all currently published quality measures on our website under “Public Reporting’ and “Medical Home.” All of our Electronic Patient Management tools (EPM Tools) are also published on the website.
General Principles -- If we fulfill all of the quality measures, which we are tracking, will we thereby transform our healthcare delivery?
The banner on SETMA’s Website states: "Healthcare improvement will result from transformation, not reformation. Reform comes from external pressure; transformation comes from internalized values and energy.” This statement is a hyperlink which takes you to an article entitled, “Healthcare Policy Issues Part III - Reforming or Transforming Healthcare.” If transparency is one of the methods of transformation – and we believe that it is, with our public reporting, we have begun. Yet, we continue to ask ourselves important question:
- If we perform excellently on the several hundred quality measures which we are tracking, can we be confident that weare “practicing good medicine”?
- If we perform excellently on these quality measures will that be transformative of our healthcare delivery?
- What other functions, measures, processes, activities or data should we be examining in order to move us toward our goal of excellence in the practice of medicine?
- Are we closer to being a Patient-Centered Medical Home than we were on February 16, 2009?
These and many other questions will occupy our attention over the next several years. On February 22, 2010, one year from when we started our pilgrimage toward being a patient-centered medical home, I sent the following note to our providers and staff:
“These are SETMA’s 2009 results for the PCPI Diabetes Measures Set. The best way to use all of the measure sets is to:
- Review your performance on the above and on all the other 2009 measurement sets which you have received today.
- Note where you need to improve and take steps to do so including reviewing the Pre-visit Preventive/Screening Audit on every patient you see at the time of your visit and reviewing the AQA (HEDIS) audit in the same way.
- Discuss with your staff the things which need to be done in order to improve your performance and put those steps into your personal workflow.
- Relentlessly pursue your personal objective of excellence.
“I believe everyone’s results are going to be dramatically improved by the end of the first quarter of this year. You will get your January-March 2010 performance results on April 1st. Via our COGNOS Project, we now have the ability to get reports done that quickly. Soon, you will be able to compare your performance from quarter to quarter on your entire patient panel, but more importantly, you will be able to look at how individuals are improving toward their goal or whether they are at goal.
“We will also have a report which will tell you what percent of your patients are at goal and what percent are not, and then, in the latter group, we will be able to tell you what percent are improving and what percent are not. This latter group, the one which is not improving, is the one for which we will then design new interventions to improve their outcomes and to move them toward their goals. In order to address “treatment inertia,” for those patients who are not a goal, we will be able to report to you if a change in treatment, life style or other intervention has been made in order to move the patient toward their goal.
“Also, remember that we want to continue to examine the question: If we fulfill all of the quality measures, which we are tracking, will we thereby transform our healthcare delivery? My answer: I think we will not; but, if we:
- Fulfill all of the quality measures
- Fulfill all 184 data points for NCQA recognition as a Patient-Centered Medical Home.
- Fulfill the 28 CMS Requirements.
- Continue and expand the clinic and inpatient follow-up calls and the care transitions from the inpatient and ER settings
- Expand our commitment to evidence-based medicine
- Engage our patients’ active participation in their care through education and training
- Expand our communications with our patients with multi-media methods
- Continue to let our patients know that we care what they think and how they are doing, actively engaging them in decisions about their care and in the execution of strategies to improve their health...
“I believe, in time, we will see our outcomes improve and we will wake up one day and suddenly realize that we are practicing a style, quality and excellence of healthcare with which we previously were not familiar. This will not happen night but it will happen.”
What about PCPI Transitions of Care Measurement Set?
Integrated – Coordinated -- Continuous; these are the words used to describe Patient-Centered Medical Home, but to give definition to these concepts CMS asks, “What Medical Home Services are delivered?” It may be that within each patient encounter, the level of care is “fairly good.” When a patient is seen by a family physician, internist, or nurse practitioner, the quality of the visit as measured by the content is good. The same is the case with procedures, labs, specialty referrals, and other points of care. The deficiencies seem to come at the transition points, or at the interface of care, i.e., when the patient is leaving the clinic, emergency department, inpatient hospital or other point of care and moving into another sphere of care.
The most common transition of care for a patient is the moving into the sphere of personal care, family care, home care or however you wish to define, describe or denote that the patient is ‘going home.” Often instructions, training or understanding is inadequate or absent in these transitions. Whether the interface is between the inpatient/home, clinic/home, laboratory/home, procedure/home, specialist/home or a number of others, the patient’s vulnerability and the decreasing of the quality of their care most often happens at these points. In an imperfect but useful metaphor, it is as if the caregivers and care receivers are on a relay team. At the point of exchange of the baton, it is often, if not almost always dropped, making the successful completion of the race impossible.
In transitioning through transforming our patient-care delivery into a Patient-Centered Medical Home, SETMA has attempted to create methods for improving these transitions (interfaces) with the following tools:
- Patient attends clinic
- A “previsit preventive care and screening care audit” is performed on the patient via SETMA’s COGNOS Project before the visit, empowering the healthcare team to fulfill the “precision” (Innovator’s Prescription concept) healthcare interventions immediately and easily. A sample previsit audit report which is the result of a real audit is displayed on SETMA’s website at Medical Home under “Previsit Evaluation.” The same audit function is also displayed in SETMA’s EMR. It is the first thing nurses and healthcares providers review at the beginning of a visit.
The following is the template which automatically tracks the status of these issues in the patient care. Everything is black applies to the patient and has been completed. Everything in grey does not apply to the patient. Everything in red applies to the patient and has not been done. If a needed intervention has not been done, the clicking of the “order” button, orders the test, posts it to the patient’s chart, sends it to the nurse, lab, etc and documents that it has been done.
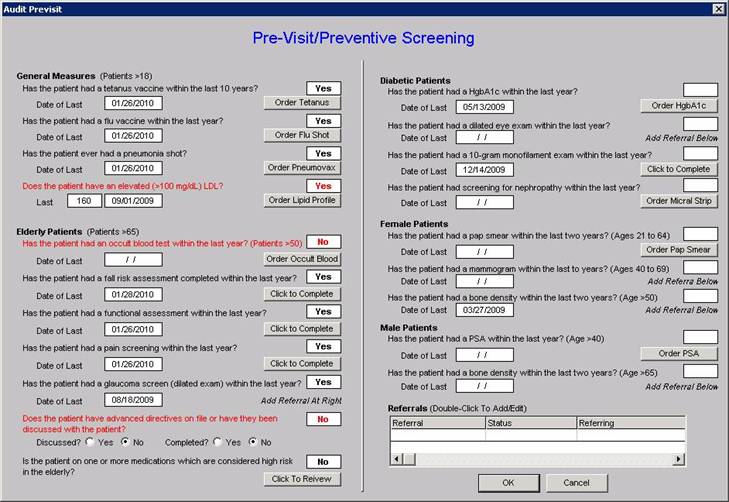
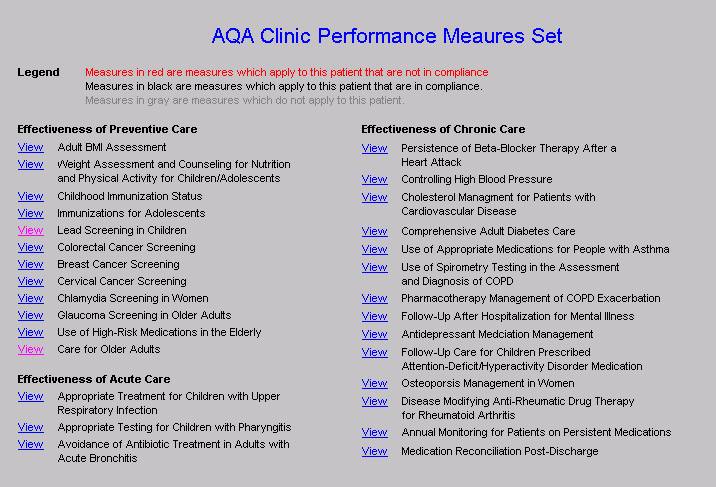
The following template displays the “ambulatory care quality measurement set” endorsed by the Ambulatory Care Quality Alliance (AQA). The AQA measurement set is identical to the HEDIS audit. The AQA Measurement Set is reviewed by every nurse and every provider at every visit. The legend is the same as for the above template: all that applies to the patient and which is up-to-date is in black; all that does not apply to the patient is in grey; all that applies to the patient and ahs not been done is in red.
- “Coordination of Care Review” is done of the patient’s “stage of care” which includes identification of care givers with contact information, medical power of attorney, emergency care instructions such as if evacuation is called for, etc., code status, evaluation of barriers of care, readiness to change evaluations, patient instructions for end-of-life management, status of multiple quality measures standards including HEDIS, AQA, NQF, PCPI, and PQRI. A Coordination of Care Review document is then given to the patient with instructions:
“Please review this document. Identify the information which is missing from your chart, such as power-of-attorney, etc. Please bring that with you to your next visit, e-mail your provider with the information or call your health care provider and give them this information. Also, please review the quality measures listed. If any apply to you and are NOT completed, please ask your provider to address these issues the next time you come to the office.”
Both the content of the Coordination of Care Review template and the note which is given to the patient is displayed on SETMA’s website at “Medical Home” under “Coordination of Care” and “Patient Document for Coordination of Care.”
- Plan of Care and Treatment Plan -- The patient is seen. All acute problems or complaints are dealt with and all chronic disease conditions are addressed such as diabetes, hypertension, dyslipidemia, chronic renal disease, CHF, asthma, cardiometabolic risk syndrome, chronic stable angina, etc. It is here that a major interface occurs and where the baton is often dropped. As a result, SETMA has designed disease management “plans of care’ and “treatment plans” which are created easily through the use of disease-management programs which aggregate treatment standards, goals, status, treatments and planned interventions. These tools include personalized, written recommendations to patients and often include appointments to care coordinators and SETMA’s education department. These evaluations always included extensive “risk stratification” which allows the provider to recommend precise, evidenced-based treatment to the patient. The details of SETMA’s ‘risk stratification” analysis is detailed on the “Plan of Care and Treatment Plan” tutorial under “Medical Home” on our website and also under “EPM Tools” under “Framingham Cardiovascular Risk”.
The disease-management tools are described in detail and the “plan of care” and “treatment plan” for each disease management tool are displayed on SETMA’s website at “Medical Home” under “Plan of Care/Treatment.” Also all disease management tools are displayed at “EPM Tools.” NOTE: SETMA has placed printers in every examination room to make the preparing of personalized healthcare information for each patient easy to produce and to give to the patient.
- Follow-up telephone calls – SETMA does not think that every patient seen in the clinic will benefit significantly from a follow-up contact via telephone but for those who are vulnerable, at risk, fragile or alone, each provider can schedule a nurse follow-up call via a follow-up telephone-call function built into our EMR. Nurses who work full-time only contacting patients will make the call when the provider designates (1 day; 3 days, 1 week; 1 month, any interval noted). The result of the call will be communicated back to the provider and further follow-up contact or intervention can be recommended.
The timing of these calls is done via an “electronic tickler file” which is described and explained on our website under “EPM Tools” or under “Medical Home” under “Telephone calls”. Also, home visits can be scheduled by the provider for safety evaluation, skilled nursing needs, or other concerns. These are done through our EMR Referral template. (All of SETMA’s agencies including Hospice and Home Health are connected via EMR.)
- Laboratory, procedure and other reports – via a template entitled “Provider Response to lab Results” the provider is able to give a precise evaluation to the patient concerning the results of their laboratory.
- Telephone Inquiry Response – via a “Telephone Inquiry template” every telephone contact is responded to via provider generate instruction. The standard is “every call from every patient answered every day.”
- Medication Reconciliation – another major interface is between the medication the patient has been prescribed, the medication the provider thinks the patient is taking and the medication the patient is actually taking. At every clinic visit, a medication reconciliation is completed and an accurate, personalized medication lists is given to the patient with the date of the visit on the list.
There are other issues related to Medical Home in regard to the clinic patient encounter but these principally fulfill the need for continuity, integration and continuousness of care.
- Patient is in the hospital
- The patient-care interface with the hospital is seamless because SETMA uses the EMR in the hospital for Admission History and Physical, Daily Progress Notes and Discharge summaries. All of these functions are described and illustrated under “EPM Tools” on SETMA’s website under the heading “Hospital Based Tools.”
When the patient leaves the hospital they are given “hospital follow-up instructions” which includes an accurate, reconciled medical list, follow-up instructions with appointments and follow-up procedures, tests, etc., already made. Any tests results not reported at the time of discharge are noted and are automatically follow-up on two days later.
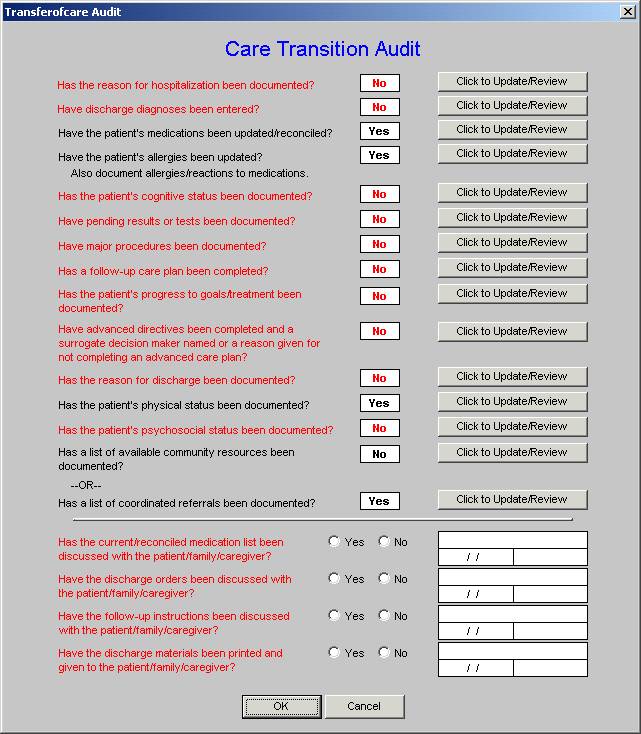
- Care Transition – in June, 2009 the AMA released the “PCPI Care Transitions measurement set”. Due to SETMA’s having used the EMR for discharge summaries for ten years, it was apparent that with very slight modification, we were fulfilling all of these measures. We immediately implemented this measurement set and are performing at 100%. As can be seen by reviewing the 14 data points and the 4 actions required by the audit, when the elements of this audit are met and when the discharge summary and follow-up document are completed with this material and are given to the patient and/or family, almost all of the continuity of care issues are resolved. The legend is that everything in black is done and everything in red has not been done. For the elements which have not been done, the “Click to updateReview” button takes the provider back to the place in the Discharge Summary where the data point at issue should be documented.
- Medication Reconciliation – it is imperative that careful medication reconciliation takes place at the end of any and every hospitalization and that a copy of the appropriate list of medications is given to the patient/family. In that SETMA completes the discharge summary in the EMR, the hospital medication reconciliation is automatically a part of the patient’s outpatient record. Nevertheless, when the patient comes back to the office, a medication reconciliation is repeated each time.
- Telephone follow-up – Every patient discharged from the emergency department or inpatient status receives a telephone call the day following their discharges. Subsequent calls can be scheduled as indicated. The follow-up call addresses current condition, medications, reactions, special needs and follow-up appointments. Since this began, five months ago, it has increased patient satisfaction, patient safety and the quality of patient care. It is early yet, but we believe it will decrease our readmission rate which is already very low. The “Hospital Follow-up Call” template which is different from the “Clinic Follow-up Call” template can be reviewed on SETMA’s website at “EPM Tools: under “Hospital Based Tools” or “Medical Home” under “Follow-up Call”.
There are other transitions and/or interfaces for which SETMA has designed equally robust solutions such as inpatient to nursing home, nursing home to home, inpatient to hospice, inpatient to home heath, etc.
Ms. Magno, I would be interested in your judgment as to whether these tools fulfill CMS’ expectations concerning care transitions and whether they would quality as delivered Medical Home services?
One last thought, at the Summit, we had a number of presentations by what I would refer to as “boutique” healthcare delivery models. They seem designed to capture market share and to yield profit but did not seem to address the issues of disparity of care, costs of care or lack of coordination or integration of care. No doubt that the “retail clinics’ are a “disruptive intervention,” which will drive all of us to answer the value of their model while avoiding the deficiencies of it. Unfortunately, some of the “medical home” solutions will, I think, even with their intent, be more kin to the “boutiques” than to a true coordinated, integrated, comprehensive and continual care. Healthsprings’ Living Well model may suffer from that deficiency. The Guided Care model of Hopkins may not be sustainable in the “real world,” while it certainly gives us all ideas about how to proceed with some of the most complex problems we face.
Thank you for your kind attention.
Sincerely yours,
James L. Holly, MD
CEO, SETMA, LLP
www.jameslhollymd.com
PS: As part of our “Public Reporting” initiative, via COGNOS, we are developing digital dashboards. The following is a brief introduction to that process.
Pubic Reporting of Provider Performance
All of the elements of quality defined by the IOM and employed by the Robert Woods Johnson Foundation for the County Health Rankings are fulfilled by Public Reporting of provider performance and by the following of the National Committee for Quality Assurance’s (NCQA) Standards and Elements for recognition as a Patient-Centered Medical Home. SETMA’s efforts toward both of these can be seen at www.jameslhollymd.com under the headings “Your Life Your Health,” Public Reporting,” and “Medical Home.”
The following is SETMA’s HgbA1C peformance by provider for January 1 – December 31, 2009.
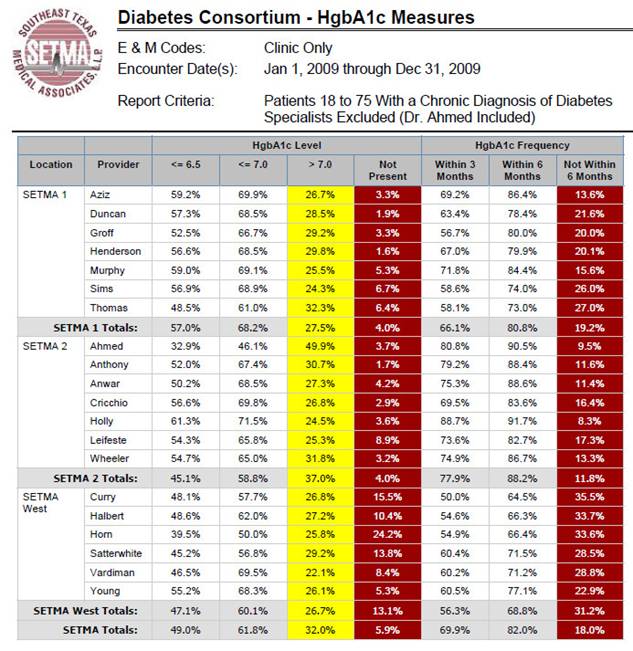
The quarterly report for October 1 – December 31, 2009 is posted on our website. Going forward the quarterly performance will be placed on the website. This transparency empowers patients with knowledge that their provider is, or is not keeping them up to date and it challenges providers to keep them up to date. In addition to hemoglobin A1Cs, SETMA tracts over 200 quality metrics, all of which are, or will be posted to our website. The community will be able to see if we SETMA providers improve over the course of this year. If I understand human nature, the above figures while very good, will dramatically improve.
What Will Be Gained by Public Reporting
In that SETMA has begun “public reporting of provider performance”, and in that we hope to:
- Improve provider performance on quality measures and on treatment to target.
- Increase patient review of our public reports
- Encourage more physician-led public reporting
I have begun to look at the medical literature on this subject. The below is a response from my inquire to one of the authors of an article entitled “Motivating Public Use of Physician-Level Performance Data,” which appeared in the Medical Care Research and Review, Vol. 66, No. 1, 68-81 (2009). (I have removed her name and address as I have not sought permission to share her comment publicly.) I am intrigued by her statement, “The short answer to your question, though, is that I do not know any other practices that are doing what you have done. The only thing I know of that comes close is the reporting being done by Beth Israel Deaconess Medical Center (Boston, MA) under the leadership of Paul Levy (CEO).”
On Wednesday, February 24, 2010, SETMA held the second of six three-hour training sessions for all of SETMA’s primary care providers on the fulfillment of quality measures and the meeting of NCQA’s 183 data points for recognition as a Patient-Centered Medical Home. All of our staff is beginning to “get it.” The recognition of the value to our patients and practice of these quality measures and of the NCQA’s PC-MH standards, and the resolution on the part of our providers to excel in the meeting of these standards is infectious.
The evidence of their enthusiasm is the fact that with only one five-minute break, they were all alert, attentive and actively engaged in the training session. Another evidence of enthusiasm came from two suggestions for improving our training sessions:
- Have different members of our staff show how they incorporate performance measures into their workflow each day.
- Send out weekly notes about where the greatest need for improve is. The recommendation of this was giving in a colloquial but communicative metaphor by a provider who said, “Send out a note telling where we are screwing up.”
Digital Dashboard
Perhaps the most exciting part of our discussion was the review of SETMA’s “diabetes digital dashboard.” Most of our COGNOS Project (for details see www.jameslhollymd.com under Public Reporting/COGNOS Project) consists of static reports which show provider compliance with NCQA Hedis, AQA Ambulatory Care, NQF, PQRI, PCPI (multiple measures) and SETMA-developed quality measurement sets.
“Digital dashboards” allow providers to contrast their performance on quality measures for diabetes with the entire clinic, multiple clinic locations, individual or selected groups of providers. The display can be by graph or bar. It contrasts patient who are treated to goal with patients who are not. It allows the provider to analyze the differences between the two groups and to see if those differences provide opportunities for improving the care of those who are not to goal.
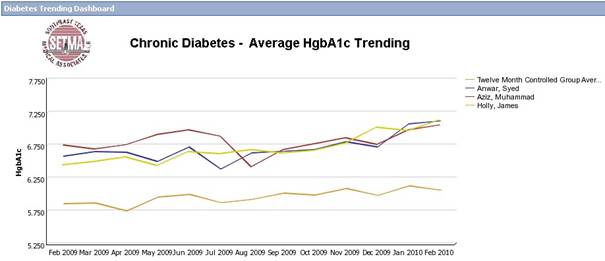
For instance, several things are obvious when we review the over-time graph of our HgbA1Cs results for all of 2009 and for several other years as well.
- Patients at goal are typically seen 2-3 times as often as those who are not.
- Patients at goal are typically tested 2 times as often as those who are not.
- SETMA’s patients with diabetes show striking patterns of gradual but significant increases in HgbA1Cs from January to December. This pattern is evident for multiple years.
As we looked at these preliminary dashboards, we began to see some patterns:
- Holidays are a real challenge to maintaining goals.
- The insurance medication “doughnut hole” may be contributing to these changes.
- The frequency of visits decreases toward the end of the year for patients not at goal.
There are other observations but these are illustrative. We are already creating strategies for improving care and compliance based on these preliminary observations.
In addition to the above-referenced article, we have looked at:
- “The American College of Cardiology Foundation’s 2008 Health Policy Statement on Principe for Public Reporting of Physician Performance Data”, published in the JACC, Vol. xx, No. X, 2008.
- “Provider Attitudes Associated with Adherence to Evidenced-Based Clinical Guidelines in a Managed Care Setting, published in the Medical Care Research and Review Volume 67 Number 1 February 2010, pp. 93-116.”
Peter Senge at MIT
The idea of using a business-intelligence software program in medicine, what we call the COGNOS Report, came from Peter Senge’s Fifth Discipline. He uses the parable of the “boiling frog” to show that in order to change behavior\, you have to create a motive for change which most often will result from a degree of discomfort. With medicine everywhere being confronted by “treatment inertia,” the motivation to change comes from external pressure. “Public Reporting” done for quality and not punitive purposes helps create that discomfort in providers who then will change their behavior. Once those changes are internalized, they become transformational with generative, self-sustaining energy, which no longer require reformational, external pressure.
Whatever the patients use of our public reporting, we believe that is will be one of the principle elements to the transformation of our practice and of our healthcare delivery model.
This is a summary of the discussion we had about “What Medical Home Services are delivered?” I will appreciate your response.
Sincerely yours
James L. Holly, MD
CEO, SETMA, LLP
www.jameslhollymd.com
|