|
For SETMA, becoming a Patient-Centered medical Home (PC-MH) was an imperative of our principles and development. A brief history explains this statement. In October, 1997, three founding partners of SETMA attended the annual MGMA meeting in Washington, D.C. Having formed in August, 1995, we realized that the demands of 21st Century medicine required a different method of documenting patient encounters than the 19th Century method of pencil and paper, or the 20th Century method of dictation and transcription. At that meeting, SETMA looked at over 50 electronic health record systems (EHR). By the time we chose our current EHR and had signed our first $650,000 check on March 30, 1998, half of those fifty EHR vendors were out of business.
Over the next 14 months, we implemented the EHR. We saw our first patients with the EHR on January 26, 1999. By May, 1999, we realized that EHR was not an appropriate goal and it was not our goal. The ability to document a patient encounter electronically was inadequate for the cost and effort of implementing an EHR. In order to achieve the promise of EHR, we needed to leverage the power of electronics to improve the care our patients. Immediately, we change our goal from EHR to electronic patient management (EPM). We immediately began building disease management tools, clinical decision support tools and creating the ability to make the healthcare process easier.
Incorporating many ideas and ideals from Peter Senge’s The Fifth Discipline which defined a “systems approach” to business, in that month, SETMA defined and published the following principles of EHR and practice design:
- Pursue Electronic Patient Management rather than Electronic Patient Records.
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
After the 2005 meeting of the Healthcare Information and Management Systems Society (HIMSS), HIMSS published a statement about SETMA on their website under the title, "The SETMA Approach to patient care.” That statement was a recital of the above ten principles.
When SETMA first heard of the Patient-Centered Medical Home in a lecture on February 16, 2009, we realized that many of the principles of PC-MH were identical to the above ten principles, which we had defined ten years earlier. While many of the newest concepts of PC-MH were not part of our experience, the overall concept seemed to be a natural extension of SETMA’s growth and development.
Not having learned much in that lecture, beginning the following day, February 17, 2009, I began writing an article each week on Medical Home for sixteen weeks. Over the next five years, SETMA published over 100 articles about Medical Home. All of those articles can be found at http://jameslhollymd.com/your-life-your-health/medical-home.
During this five-year transformation effort, SETMA defined what we believe to be the key to the future of healthcare, which is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be the patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
All of these efforts gradually developed into SETMA’s Model of Care which is described in detail at: http://jameslhollymd.com/The-SETMA-Way/pdfs/setma-model-of-care-pc-mh-healthcare-innovation-the-future-of-healthcare.pdf.
PC-MH was not so much a choice for SETMA as it has been a logical imperative of our growth and development. SETMA was moving toward PC-MH before we ever heard the term and before we understood the concept.
SETMA did not so much “decide” to become a PC-MH as we arrived at a point in our development where it was the only logical next step for us. As EHR had transformed our approach to healthcare and to patient encounters, PC-MH provided a method for achieving the results we wanted. On August 24, 2000, I made a presentation to the Beaumont, Texas Chamber of Commerce on how to solve the healthcare challenges of the 21st Century and particularly how to solved the challenges of excellent healthcare for the indigent and uninsured. In part I said:
“Healthcare providers must never lose sight of the fact that they are providing care for people, who are unique individuals. These individuals deserve our respect and our best. Healthcare providers must also know that the model of healthcare delivery, where the provider was the constable attempting to impose health upon an unwilling subject, has changed. Healthcare providers progressively are becoming counselors to their patients, empowering the patient to achieve the health the patient has determined to have. This is the healthcare model for the 21st Century and the computerized patient record is the tool, which makes that model possible.”
After starting the process of PC-MH transformation in February, 2009, on April 14, 2009, I summarized some of our progress with the following note:
"Yesterday, I asked my assistant to tally the number of pages of materials which we have possessed in our Medical Home pilgrimage. I was amazed to learn that it is 2,280 pages, contained in 9 notebooks with material from NCQA, CMS, NQF, and PQRI, along with over 600 pages of materials which have been produced and written by SETMA staff. This has been a prodigious effort and a Herculean project. We are virtually at the end of the beginning.
"...by the end of this year, at the very latest, we expect to have incorporated into our EMR and into our work flow evidence-based standards and structure of healthcare , with the capacity for each provider to daily evaluate their own performance at the point-of-care, from:
- Healthcare Effectiveness Data and Information Set (HEDIS)
- National Committee on Quality Assurance (NCQA)
- National Quality Forum (NQF)
- Physician Consortium for Physician Performance Improvement (PCPPI)
- Physician Quality Reporting Initiative (PQRI)
- Patient Centered Medical Home (PCMM) - in process, application to be submitted in September
- E-prescribing
“As this is written, June 2, 2009, all of the above is complete and the data to support the NCQA application is being collected daily. The application for NCQA recognition will be completed in September, supported by the data which we began to collect on June 1, 2009”
Because of the requirement by the National Committee for Quality Assurance for medical home practices to report ten National Quality Forum endorsed quality metrics to providers internal to the practice and to an external organization, in August, 2009, SETMA adopted a business intelligence soft practice to fulfill that require. But, because it “fit” our model of care, actually, because it defined SETMA model of care, we determined to begin public reporting by provider name on our website, SETMA providers’ performance on hundreds of quality metrics.
In fact, the PC-MH not only helped define SETMA’s model of care, it also was virtually demanded by the SETMA Model of Care. The following is a brief description of that model:
- The tracking by each provider on each patient of the provider’s performance on preventive care, screening care and quality standards for acute and chronic care. SETMA"s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provide.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool “plans of care” and the medical-home-coordination document summarizes a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Permanence Improvement (QAPI) Initiatives - this year SETMA"s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a Business Intelligence (BI) Report which allows us to analyze our hospital care carefully.
This is a question too large for a brief discussion but the following are some of the differences. Each is defined largely by its history. NCQA depends upon data and the completion of extensive documentation about practice performance of principles and elements within those principles. NCQA focuses only on the activities, the structure and the dynamic of PC-MH. SETMA currently holds all of the recognitions provided by NCQA including PC-MH, Diabetes, and Cardiac/Stroke. In April, 2014, we will receive the Distinction in Patient Experience Reporting for our use of the Consumer Assessment of Healthcare Providers and Systems (CAHPS).
AAAHC, URAC and the Joint Commission each expand already existing accreditation activities to include medical home. Each requires extensive site visits and includes accreditation of ambulatory care as well as medical home. The ambulatory care accreditation involves quality and safety standards which form the infrastructure for excellence in medical home.
If a practice is very serious about Medical Home, SETMA’s current perspective would recommend that a practice take the following accreditation steps:
- Pursue and achieve NCQA Tier 3 recognition for PC-MH and deploy the CAPHS-PC-MH program. Our caution would be for an organization not to assume that this achievement is the end of the medical home pilgrimage but that it is a good beginning.
- Once this first step is achieved, SETMA would recommend that all groups choose one of the other accreditation bodies (AAAHC, URAC, Joint Commission) for evaluation of the practice. This assurances that the practice’s safety and quality measures required to achieve continuous quality improvement are in place.
- Once this second step is achieve, SETMA recommends that practices work with Planetree to achieve a Practice Culture assessment for maximum transformative purposes in patient-centered care.
Through SETMA’s experience over the past five years, we have developed an Accrediation Team made up of healthcare providers including physicians, NPs RNs, and LVNs, administration, and IT. This team’s expertise developed over time to allow the practice to continue to learn from the accrediting bodies without major disruption to the actual practice of PC-MH.
Currently, it is SETMA’s opinion that all five of the organizations make significant contributions to the transformation of practices into PC-MHs. No practice would be wasting time or resources to pursue accreditation by all organizations. In our judgment, any accreditation process should be educational as well as evaluation-al. So it is with accreditations, you will learn more and more about yourself from each of these. That is not to say that it is necessary to achieve all five accreditation, but it is to say that the process within itself contributes to practice transformation.
Increasingly, we are learning that all four domains of care are essential to excellence in care. Remember, in our judgment those domains are:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be the patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
Don’t be satisfied with the form and structure of medical home, but seek the true spirit and dynamic which will increase provider professional satisfaction and will increase the patient’s sense of being valued and of being a part of his/her own healthcare team.
Patient flow in the old “paternalistic” healthcare system (see http://jameslhollymd.com/your-life-your-health/paternalism-or-partnership-the-dynamic-of-the-patient-centered-transformation for more on this concept) was defined by “chief complaint,” “review of systems,” “history of present illness,” etc. These are still important but only in a secondary way. Medical Home employs a new vocabulary with words and concept like “activation,” “engagement,” “shared-decision making,” “patient-centered conversation.” Etc.
The new work flow now involves the “Passing the Baton”
While healthcare provider performance is important for excellent care of a patient’s health, there are 8,760 hours in a year. A patient who receives an enormous amount of care in a year is in a provider’s office or under the provider’s direct care less than 60 hours a year. This makes it clear that the patient is responsible for the overwhelming amount of their own care which includes compliance with formal healthcare initiatives and with lifestyle choices which support their health.
If responsibility for a patient’s healthcare is symbolized by a baton, the healthcare provider carries the baton for .68% of the time. That is less than 1% of the time. The patient carries the baton 99.32% of the time. The coordination of the patient’s care between healthcare providers is important but the coordination of the patient’s care between the healthcare providers and the patient is imperative.
Often, it is forgotten that the member of the healthcare delivery team who carries the “baton" for the majority of the time is the patient and/or the family member who is the principal caregiver. If the „baton" is not effectively transferred to the patient or caregiver, then the patient’s care will suffer.
Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient,
If change is to make a difference 8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home are symbolized by the “baton.” Its display will continually remind the provider and will inform the patient, that to be successful, the patient’s care must be coordinated, which must result in coordinated care. In 2011, as we expand the scope of SETMA"s Department of Care Coordination, we know that coordination begins at the points of “transitions of care,” and that the work of the healthcare team - patient and provider - is that together they evaluate, define and execute that care.
Yes, we did it by example in how we engaged our patients during office visits, in transitions of care, in coordination of care and in the written materials which we gave to the. We believed we were making progress when we began to hear our patients say in the community, “What has happened at SETMA, things have really changed.”
Through a weekly newspaper column, which SETMA has prepared weekly for the past fourteen years, through our website, through materials we distributed to the patient (see http://jameslhollymd.com/patients/what-does-patient-centered-medical-home-mean-to-you), we began to explain to patients what we were doing. We formed a Department of Care Coordination, in care coaching, and a Foundation through which we can help patients financially when they cannot afford their care.
We have now formed a Community Council which will meet monthly for three months and quarterly thereafter. We will have our first meeting on April 17, 2014. Members of the Council are patients of SETMA, community leaders, SETMA colleagues and employees. Patients have the majority vote on the Council and the majority vote will prevail with the only limitation being compliance with State and Federal statues and with Texas Medical Board rules.
We display throughout our practice framed copies of the Baton in all public areas and in every examination room a poster copy of the Baton. We display our accreditation certificates in multiple places. For URAC, throughout six clinical locations we have 29-framed copies of the accreditation certificate. This gives us an opportunity to engage our patients in a discussion of medical home when they ask about the meaning of the certificate.
SETMA has a monthly, half day meeting with all our healthcare providers. We have meetings with nurses and other staff. We have continual “electronic huddles” in which we discuss our vision and our goals. In that way, we also involve all staff and locations as a team. Everyone has their responsibilities. They are acknowledged and rewarded for excellence. Most of all, the patients’ response to the PC-MH motivates the employees and staff to interact with the patients in a patient-centric fashion.
We have taught all of our staff repeated the principle that “convenience is the new word for quality.” Initially, the idea of convenience in the scheduling of multiple appointments at the same time was the extent of SETMA's understanding of this element of coordination. Eventually, "convenience" was translated into the understanding that coordinated care means more than just making patients comfortable; it meant and it resulted in:
- Convenience for the patient, which
- Results in increased patient satisfaction, which contributes to
- The patient having confidence that the healthcare provider cares for the patient personally, which
- Increases the trust that the patient has in the provider, all of which
- Increases compliance (adherence) in the patient obtaining healthcare services recommended, which
- Promotes cost saving in travel, time and expense of care, which
- Results in increased safety, quality of care and cost saving for the patient.
Convenience is a process, not an outcome, of coordination of care. Therefore, SETMA formed a Department of Care Coordination and created a convenient method for enlisting that department in a patient’s care. It was only through this analysis that we accepted "convenience" as a worthy goal of quality care as opposed to it only being a means of "humoring" patients. This fulfilled SETMA's goal of ceasing to be the constable, attempting to impose healthcare on our patients; and, to our functionally becoming the consultant, the collaborator, the colleague to our patients, empowering them to achieve the health they have determined to have.
The transformation of SETMA into a PC-MH meant a significant change in our culture, attitudes, values and actions.
NCQA was the stimulus for our initial changes to become a medical home. We started this process in 2009. Being inexperienced, our first application to NCQA in 2010 resulted in a Tier 1 (the lowest) designation. Unwilling to accept this, we ask questions. It turned out that we had not completed the form correctly and when we changed that, we received a Tier III in 2010 and again in 2013.
When we applied to AAAHC in 2010, our first effort achieved only a one-year accreditation but when we reapplied in 2011, we received a full three-year accreditation. We reapply in June, 2014 for AAAHC renewal and are well prepared.
When we went through URAC and Joint Commission surveys we had experienced multiple accreditation and we did very well the first time. Now having gone through six accreditation experiences (NCQA twice, AAAHC twice and soon the third time, URAC and Joint Commission once), we have a systematic approach. We will renew all four at least two or three cycles and then we’ll make the decision of which ones to maintain permanently. It may be that we will maintain all four and also begin to work with Planetree as well.
The major benefit of multiple accreditations is that we have to go through our entire practice carefully. Our provider credentialing and privileging processes are excellent now. Our infection control processes are sound. Our provider and staff education and competency training are sound and in place. We have a true “continuous quality improvement” culture and environment.
While some resist and avoid the transparency of external evaluation, SETMA sees the benefit. Having “extra sets of eyes” on our practice, processes, safety and quality programs are both challenging and valuable.
As stated above, our recommendation is at a minimum three. The radical change required in a practice to become a “real” medical home will generally not be achieved with a single recognition or accreditation. Multiple site visits and the meeting of multiple standards will drive improvement to excellence.
The process is more interactive and dynamic. The preparation is more through and the potential for dramatic benefit to the practice is greater with a multi-day, multi-surveyor team evaluating your practice. There is greater learning on the part of the practice.
The attention they are given, the experience their healthcare provider is gaining in patient-centered conversations, the safety and quality of the care they are receiving is greater. The transparency of public reporting and of their representatives participating in the Community Council is providing addition benefits.
If we had stopped at one or two accreditations, we would not have been pressed and motivated to continue this transformative process. We would have been a medical home in name but not in reality. We believe that the process of transformation will continue forever. SETMA will move forward but each achievement suggests new ways in which we can improve the care our patient receive and the health which they can achieve.
Absolutely. This past week, while looking for another document, I came across the following note to SETMA’s staff. We set goals in February, 2009, all of which we have achieved and more.
From: James L. Holly
Sent: Wednesday, September 16, 2009 8:33 AM
To:
Subject: RE: Medical Home Initiative and the current and continuing projects undertaken by SETMA
-----Original Message-----
From: James L. Holly
Sent: Monday, February 16, 2009 6:44 AM
To: Providers; Executive Management; Nurses; IT
Subject: Medical Home Initiative and the current and continuing projects undertaken by SETMA
Preparatory to the introduction of the “medical home” concept and the adoption of this model by SETMA, the attached are in word form for you to print and read. The first and largest file is a 2004 article about the rethinking of healthcare delivery by family physicians, which equally applies to internal medicine and pediatrics. The second file is a comment about the concept of “medical home,” which was jointly announced by the AAFP, ACP and AOA in 2007, which is the third article above. On Tuesday evening, Jon, Rick, Margaret and I will be attending a Select Care meeting on medical home in Houston.
The following are initiatives which SETMA is simultaneously pursing. This is daunting but doable if we all contribute to the effort.
- NCQA certification of our diabetes treatment program
- e-prescribing €“ essentially done
- affiliation with Diabetes Center of Excellence €“ to be done by May 1st at the latest
- Reporting quality indicators for recognition and reimbursement by CMS
- Medical Home €“ first for our HMO patients and then for all of our patients
In the midst of all of this, we are maintaining our attention upon HCC and RxHCC documentation, LESS Initiative (Lose Weight, Exercise, Stop Smoking), diabetes center of excellence and our disease management programs, as well as the continuity of care between clinic, hospital, nursing home and home.
James L. Holly, MD
CEO, SETMA, LLP
These achievements have contributed to the improved care our patients have received and our participation in the national dialogue about healthcare improvement.
The national healthcare policy debate has been cast in terms of reforming of the system. I would argue that reforming is an inadequate goal, doomed to failure, and even if should succeed; reformation of the healthcare system will not produce the positive results which are legitimately desired by all participants in the debate. I would argue that if healthcare change is going to improve care, improve the quality of life, cover all Americans, and address the rising cost of care, we must have transformation of the healthcare system and not simply reformation.
Does the distinction between reformation and transformation of the system really make a difference? In order to examine this question, we must define our terms. The definition of "reformation" is "improvement (or an intended improvement) in the existing form or condition of institutions or practices etc.; intended to make a striking change for the better in social or political or religious affairs." Synonyms for "reformation" are "melioration" and "improvement." Another definition states, "The act of reforming, or the state of being reformed; change from worse to better."
On the other hand, "transformation" is defined as, "a marked change in appearance or character, especially for the better." "Metamorphosis," a synonym for "transformation," is the transliteration of a Greek word which is formed by the combination of the word "morphe" which means "form," and "meta" which means "change." "Metamorphosis" conveys the idea of a "noticeable change in character, appearance, function or condition." Metamorphosis is what happens when a caterpillar morphs into a butterfly.
In function, the distinction between these two concepts as applied to healthcare is that "reformation" comes from pressure from the outside, while "transformation" comes from an essential change of motivation and dynamic from the inside." Anything can be reformed - reshaped, made to conform to an external dimension - if enough pressure is brought to bear. Unfortunately, reshaping under pressure can fracture the object being confined to a new space. And, it can do so in such a way as to permanently alter the structural integrity of that which is being reformed. Also, once the external pressure is eliminated, redirected or lessened, the object often returns to its previous shape as nothing has fundamentally changed in its nature.
Being from within, transformation results in change which is not simply reflected in shape, structure, dimension or appearance, but transformation results in a change which is part of the nature of the organization being transformed. The process itself creates a dynamic which is generative, i.e., it not only changes that which is being transformed but it creates within the object of transformation the energy, the will and the necessity of continued and constant change and improvement. Transformation is not dependent upon external pressure but is sustained by an internal drive which is energized by the evolving nature of the organization.
While this may initially appear to be excessively abstract and unwieldy, it really begins to address the methods or tools needed for reformation or for transformation. They are significantly different. The tools of reformation, particularly in healthcare administration are rules, regulations, and restrictions. Reformation is focused upon establishing limits and boundaries rather than realizing possibilities. There is nothing generative - creative - about reformation. In fact, reformation has a "lethal gene" within its structure. That gene is the natural order of an organization, industry or system's ability and will to resist, circumvent and overcome the tools of reformation, requiring new tools, new rules, new regulations and new restrictions. This becomes a vicious cycle. While the nature of the system actually does change, where the goal was reformation, it is most often a dysfunctional change which does not produce the desired results and often makes things worse.
The tools of transformation may actually begin with the same ideals and goals as reformation, but now rather than attempting to impose the changes necessary to achieve those ideals and goals, a transformative process initiates behavioral changes which become self-sustaining, not because of rules, regulations and restrictions but because the images of the desired changes are internalized by the organization which then finds creative and novel ways of achieving those changes.
It is possible for an organization to meet rules, regulations and restrictions perfunctorily without ever experiencing the transformative power which was hoped for by those who fashioned the external pressure for change. In terms of healthcare administration, policy makers can begin reforms by restricting reimbursement for units of work, i.e., they can pay less for office visits or for procedures. While this would hopefully decrease the total cost of care, it would only do so per unit. As more people are added to the public guaranteed healthcare system, the increase in units of care will quickly outstrip any savings from the reduction of the cost of each unit.
Historically, this has proved to be the case. When Medicare was instituted in 1965, projections were made about the increase in cost. In 1995, it was determined that the actual utilization was 1000% more than the projections. No one had anticipated the appetite for care and the consequent costs which would be created by a system which made access to care universal for those over 65 and which eliminated most financial barriers to the accessing of that care.
Reformation of healthcare promises to decrease the cost of care by improving preventive care, lifestyles and quality of care. This ignores the initial cost of preventive care which has a payoff almost a generation later. It ignores the fact that people still have the right, which they often exercise, to adopt unhealthy lifestyles. Even the President of the United States continues to smoke.
The currently proposed reformation of the healthcare system does nothing to address the fact that the structure of our healthcare system is built upon a "patient" coming to a healthcare provider who is expected to do something "for" the patient. The expectation by the system and by the recipient of care is that something is going to be done "to" or "for" the patient in which process the patient is passive. There is little personal responsibility on the part of the patient for their own healthcare, whether as to content, cost or appropriateness. The healthcare provider is responsible for the health of the patient.
Transformation of healthcare would result in a radical change in relationship between patient and provider. The patient would no longer be a passive recipient of care given by the healthcare system. The patient and provider would become an active team where the provider would cease to be a constable attempting to impose health upon an unwilling or unwitting patient. The collaboration between the patient and the provider would be based on the rational accessing of care. There would no longer be a CAT scan done every time the patient has a headache. There would be a history and physical examination and an appropriate accessing of imaging studies based on need and not desire.
This transformation will require a great deal more communication between patient and provider which would not only take place face-to-face, but by electronic or written means. There was a time when healthcare providers looked askance at patients who wrote down their symptoms. The medical literature called this "la maladie du petit papier" or "the malady of the small piece of paper." Patients who came to the office with their symptoms written on a small piece of paper where thought to be neurotic.
No longer is that the case. Providers can read faster than a patient can talk and a well thought out description of symptoms and history is an extremely valuable starting point for accurately recording a patient's history. Many practices with electronic patient records are making it possible for a patient to record their chief complaint, history of present illness and review of systems, before they arrive for an office visit. This increases both the efficiency and the excellence of the medical record and it part of a transformation process in healthcare delivery.
This transformation will require patients becoming much more knowledgeable about their condition than ever before. It will be the fulfillment of Dr. Joslin's dictum, "The person with diabetes who knows the most will live the longest." It will require educational tools being made available to the patient in order for them to do self-study. Patients are already undertaking this responsibility as the most common use of the internet is the looking up of health information. It will require a transformative change by providers who will welcome input by the patient to their care rather seeing such input as obstructive.
This transformation will require the patient and the provider to rethink their common prejudice that technology - tests, procedures, and studies - are superior methods of maintaining health and avoiding illness than communication, vigilance and "watchful waiting." Both provider and patient must be committed to evidence-based medicine which has a proven scientific basis for medical-decision making. This transformation will require a community of patients and providers who are committed to science. This will eliminate "provider shopping" by patients who did not get what they want from one provider so they go to another.
This transformation will require the reestablishment of the trust which once existed between provider and patient to be regained. That cannot be done by fiat. It can only be done by the transformation of healthcare in to system which we had fifty to seventy-five years ago. The patient must be absolutely confident that they are the center of care but also they must know that they are principally responsible for their own health. The provider must be an extension of the family. This is the ultimate genius behind the concept of Medical Home and it cannot be achieved by regulations, restrictions and rules.
The transformation will require patient and provider losing their fear of death and surrendering their unspoken idea that death is the ultimate failure of healthcare. Death is a part of life and, in that, it cannot forever be postponed, it must not be seen as the ultimate negative outcome of healthcare delivery. While the foundation of healthcare is that we will do no harm, recognizing the limitations of our abilities and the inevitability of death can lead us to more rational end-of-life healthcare choices.
Public policy can determine whether healthcare is reformed or transformed
First, that policy must acknowledge that governmental policy created the current conditions. Payment by "piece work" put the government's check book in providers' hands. The Providers only benefited; they did not create the system which rewarded over-utilization and expansion of services.
Second, the healthcare system must reward what is valued and what the system wants to promote. In that all of the transformative issues in healthcare are relational rather than technological, the system must promote relationships by rewarding efforts to restore the provider/patient relationship as the basis of care. Even specialist reimbursement should be increased for personal patient management even while the payment for procedures is decreased. The expertise of the specialist benefits patient care without necessarily requiring expensive procedures.
Third, public policy must place the patient at the center of concern in the healthcare equation, but also must place the patient at the center of responsibility. Patients cannot be allowed to be passive in their care and they cannot transfer their responsibility for their own care to anyone else.
Fourth, healthcare policy must pay for educational medical services but not in such a way as to create a new industry. Providers who create educational opportunities for their patients should be rewarded for doing so.
Fifth, as patients cannot be passive in medical decision making, they cannot be passive in the utilization of resources. No one would argue that a sick person should be denied care unless they can pay for it. However, if a patient continues an activity which adversely affects their healthcare, there should be consequences and those should be partially financial.
Sixth, one side of the healthcare debate argues that improved preventive care will produce dramatic savings in healthcare cost. The other side argues that dramatic decreases in care will be produced by tort reform. Neither is likely to be true. The transformation of healthcare delivery will result in improved preventive care and will result in fewer instances of patient dissatisfaction with their care and/or instances of patient injury, thus decreasing legal actions against providers. Neither, as a primary initiative, will transform healthcare.
Seventh, SETMA and many physicians, nurse practitioners and other healthcare professionals with whom I have contact are working toward transforming their practices of medicine to fulfill the promise of the metamorphosis of healthcare. They each and they all illustrate the final principle of transformation. To be lasting and to be effective, it will be done one practice at a time. At some point, we will reach critical mass and we will see the impact upon our community and upon our country.
Public policy will require some action to make changes in our healthcare system. What is imperative is that those changes which are directed at reforming the system do not ultimately prevent the transforming of the system.
From: Susan Schooleman [mailto:sschooleman@mgma.org]
Sent: Wednesday, April 16, 2014 9:53 AM
To: James L. Holly
Cc: Dave Gans; Kristina Ziehler
Subject: Thank you so much for your response
Dr. Holly,
This is really amazing. You not only see patients, oversee this revolutionary group, but you also took the time to answer all of the questions in writing.
Thank you so much for your great attention to detail and obvious intelligence/expertise! I am going to read through this and follow-up with anything during our interview scheduled for today. Judging by the thoroughness of your comments, the interview will probably will not require much of your valuable time.
Again, thank you. You are a true pioneer €“ and it will be a genuine honor to finish this with you.
Sincerely yours,
Susan Schooleman
Staff Writer, MGMA
From: James L. Holly [mailto:jholly@jameslhollymd.com]
Sent: Wednesday, April 16, 2014 9:10 AM
To: Susan Schooleman
Cc: Dave Gans; Kristina Ziehler
Subject: RE: Thank you so much for your response
By the way, lest you think too much of me, I read your questions last night and I came to the office at 1:45 AM this morning and spent 5 hours thinking further and writing the answers. Several reasons why I do this:
- It gives me the opportunity to think about how best to address the issues.
- It makes your task a little easier and you don’t have to record the interview and the listen to it €“ you can read faster than I can talk.
- Invariable, it preparing for an interview I will organize things in a new and creative and will be able to not only post your article on our website (under In-The-New there are over 210 articles which have been written about our practice, but from many of those articles have come new and innovative ideas.
Your extremely kind words below are great appreciated although their fulsomeness causes me to question your judgment as I don’t recognize the person of which you are talking! Smile
James (Larry) Holly, M.D.
From: Susan Schooleman [mailto:sschooleman@mgma.org]
Sent: Wednesday, April 16, 2014 10:39 AM
To: James L. Holly
Subject: RE: Thank you so much for your response
Dr. Holly,
I appreciate your answers so much. Thank you again and again. Not surprised about your sleeping hours. Successful people don’t require much shut-eye. (:
And thanks so much for crediting MGMA. I notice the entire story began after the annual MGMA meeting, so I will stress that. Just read through the initial document. Love the baton analogy €“ and your “constable or counselor” discussion.
I am just getting ready to read the addendums, so you may have already covered this, but is there a way to “quantify” the ROI? For example, with the improved quality from this, is there a way to say that X percent patients have reduced their complications by X percent? Also, is there a way to quantify the cost-savings? We’ve heard a lot of practices are STILL reluctant to do this because of the cost of certification and even EHRs.
Again, you may well cover this on the addendums, which I am getting ready to read right now.
Look forward to speaking with you! Susan
From: James L. Holly
Sent: Wednesday, April 16, 2014 11:42 AM
To: 'Susan Schooleman'
Cc: David Gann (dgans@mgma.org); Kristina Ziehler
Subject: RE: Thank you so much for your response ROI
SETMA, as an organization and as a Medical Home, is deeply committed to The Triple Aim as defined by IHI. In May, 2012, I made a presentation to the Large-User’s Group Meeting for the EMR Vendor whose product SETMA purchased in 1998. The only deficient in this presentation is that it names our vendor as it was presented to their existing clients. I have a rigid principle not to identify the vendor at meetings.
The following is the link to that presentation: http://jameslhollymd.com/Presentations/NextGen-As-A-Tool-For-Redesigning-Primary-Care-To-Fulfill-IHI-Triple-Aim. I had three-hours to make the presentation. In this presentation, I said: “(IHI’s)€¦concept design (included)€¦an initial set of components of a system that would fulfill the Triple Aim. Five of the components are:
- Focus on individuals and families
- Redesign of primary care services and structures
- Population health management
- Cost control platform
- System integration and execution”
“Improving U.S. health care system requires simultaneous pursuit of three aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care. Preconditions for this include: enrollment of identified population, a commitment to universality for its members, and the existence of an organization (an “integrator”) that accepts responsibility for all three aims for that population.”
From the healthcare provider’s perspective, the Triple Aim Integrators are:
- Medicare Advantage
- Medical Home
- Accountable Care Organizations
Each of these “structures” requires primary care redesign in order to be successful.
SETMA has worked in Medicare Advantage and its predecessors since 1996. Our systems approach to our patient’s care has helped us be successful financially. As a result, SETMA has spent over $8,000,000 on IT integration across all hospitals, nursing homes, clinics, emergency departments, etc. And, we have been able over this period of time to have excessive review where the partners of SETMA have been able to give $500,000 a year to The SETMA Foundation. This money cannot profit SETMA or the partners of SETMA but is used to provide access to care by our patients who cannot afford care. It has allowed SETMA to build an organization where we monthly spend over $190,000 of uncompensated and unreimbursed funds to provide care and benefits to our patients. Without what is commonly called Return on Investment (ROI), which is positive, SETMA partners and Executive Staff would not be able to sustain these efforts for our patients benefit.
So as not to mislead, I quickly add that SETMA providers are well compensated , but to the credit of the partners and staff, they could have made a great deal more money if they did not have a commitment to excellent care for all of our patients.
The scope of the Triple Aim was defined by Senator Hubert Humphrey in 1977; he said:
“The moral test of government is how it treats those who are In the dawn of life, the children; those who are in the twilight of life, the aged; and those in the shadows of life, the sick, the needy and the handicapped.” (November 4, 1977, Senator Humphrey, Inscribed on the entrance of the Hubert Humphrey building, HHS Headquarters; Donald Berwick, “The Moral Test” Keynote Presentation, December 7, 2011 IHI 23rd Annual National Forum on Quality Improvement in Health Care)
SETMA is not a government but has adopted the values of Senator Humphrey’s philosophy in the allocation of revenue for he benefit of our patients.
This is our ROI.
For an analysis of ethnic disparities, our data for the treatment of diabetes for the past twelve months is as follows:
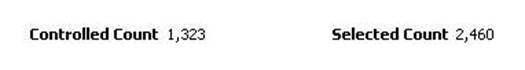
Before the judgment is made that Caucasians receive significantly better healthcare, the bar graph must be described.
- 3783 patients seen by SETMA providers in the past twelve months had diabetes.
- As a percentage of the 3783 patients with diabetes 1,323 were controlled. (For this audit, "controlled" is defined as the patient having had a HgbA1C below 6.5 % for the entire year.) If, as in the case of the National Quality Forum (NQF) Comprehensive Diabetes Measurement Set, "controlled" were defined as below 7% and the measure called for an examination only of the most recent HgbA1C, the percentage of those designated as "controlled" would rise to 59.9%.
- 60.9% of the patients who had diabetes and who were seen in the past twelve months and whose HgbA1c was below 6.5% for the entire year, were Caucasians
- 32.7% of African American treated by SETMA who had diabetes, who were seen in the past twelve months and who had HgbA1C done had a HgbA1C continuously below 6.5%.
- The second classification on this graph is entitled "selected." In the case of the above bar graph, "selected" refers to all patients whose diabetes, at any point in the year, was above 6.5%. There were 2460 of them.
At first glace, it might be assumed that the care of Caucasians was twice as good as that of African Americans. But note that the percentage of "controlled" and "Selected" is not of a subset but a percentage of the same whole. As a percent of the whole, SETMA treats twice as many Caucasians as African Americans. As a percent of those who exhibited continuous control of their diabetes, it is the same proportion of African American as Caucasian. Their treatment judged by process measures or by outcomes measures is identical. The conclusion is that the ethnic distribution of all of SETMA's patients with controlled diabetes is nearly identical to the ethnic distribution of SETMA's patients with uncontrolled diabetes.
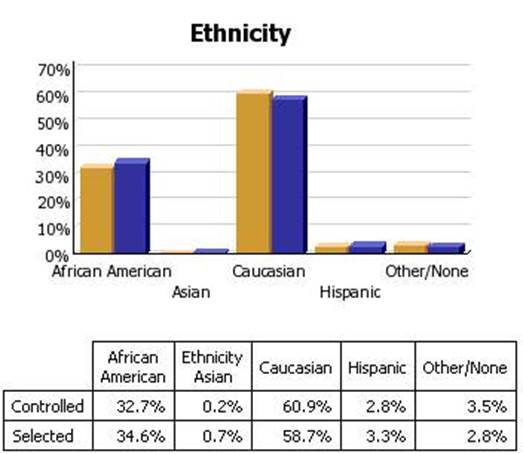
For an analysis of ethnic disparities, our data for the treatment of diabetes for the past twelve months is as follows:

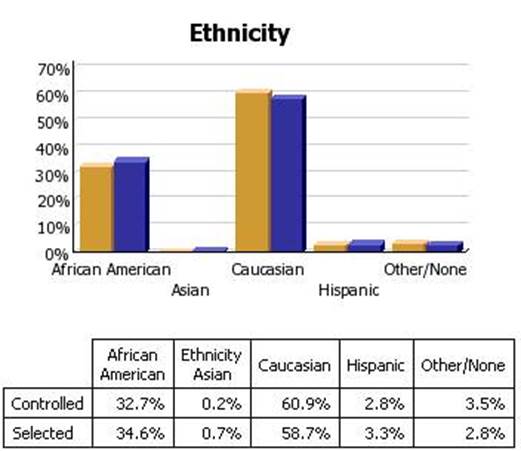
Before the judgment is made that Caucasians receive significantly better healthcare, the bar graph must be described.
- 3783 patients seen by SETMA providers in the past twelve months had diabetes.
- As a percentage of the 3783 patients with diabetes 1,323 were controlled. (For this audit, "controlled" is defined as the patient having had a HgbA1C below 6.5 % for the entire year.) If, as in the case of the National Quality Forum (NQF) Comprehensive Diabetes Measurement Set, "controlled" were defined as below 7% and the measure called for an examination only of the most recent HgbA1C, the percentage of those designated as "controlled" would rise to 59.9%.
- 60.9% of the patients who had diabetes and who were seen in the past twelve months and whose HgbA1c was below 6.5% for the entire year, were Caucasians
- 32.7% of African American treated by SETMA who had diabetes, who were seen in the past twelve months and who had HgbA1C done had a HgbA1C continuously below 6.5%.
- The second classification on this graph is entitled "selected." In the case of the above bar graph, "selected" refers to all patients whose diabetes, at any point in the year, was above 6.5%. There were 2460 of them.
At first glace, it might be assumed that the care of Caucasians was twice as good as that of African Americans. But note that the percentage of "controlled" and "Selected" is not of a subset but a percentage of the same whole. As a percent of the whole, SETMA treats twice as many Caucasians as African Americans. As a percent of those who exhibited continuous control of their diabetes, it is the same proportion of African American as Caucasian. Their treatment judged by process measures or by outcomes measures is identical. The conclusion is that the ethnic distribution of all of SETMA's patients with controlled diabetes is nearly identical to the ethnic distribution of SETMA's patients with uncontrolled diabetes.
|