|
October 9, 2010
Larry Gamm, Ph.D
Director, Center for Health Organization Transformation
Professor and Head, Department of Health Policy and Management
School of Rural Public Health
Texas A&M Health Science Center
MS 1266
College Station, TX 77843
Dear Dr. Gamm:
This letter follows up on our conversations and review of your research plans for your grant submission titled: EHR and Patient-Centered Care Optimization in Healthcare Organizations. Southeast Texas Medical Associates, LLP (SETMA) looks forward to serving as a collaborative site for the research you propose.
SETMA is well-suited for the type of research you propose. Since 1998, SETMA has been involved in the transformation of healthcare delivery through an electronic health record (EHR). Early in that process, we realized that EHR was too expensive and too difficult if all we were to achieve in the process was an electronic methodology for documenting a patient encounter. As a result, in 1999, we adopted the goal of “electronic patient management (EPM),” which we define as the ability to leverage the power of EHR to improve healthcare processes and outcomes. SETMA has thirty healthcare providers in three clinical and seven non-clinical locations.
SETMA uses the NextGen EHR platform in a customized version. SETMA has achieved the following official recognitions:
- Become the first, multi-specialty affiliate of Diabetes Center of Excellence which is affiliated with Harvard Medical School in Boston, Massachusetts.
- NCQA recognition as a Tier III Patient-Centered Medical Home for each of our clinics.
- NCQA recognition in their Diabetes Recognition Program for all three clinics.
- Accreditation Association for Ambulatory Healthcare (AAAHC) accreditation for Ambulatory Care.
- AAAHC accreditation for Medical Home.
SETMA is currently engaged in expanding our electronic tools which will further our mission of providing coordinated, integrated, evidenced-based care to the population we serve, which is the most vulnerable in our community. We agree with the thrust of the proposal regarding the need to investigate more fully with your Center ‘s researchers how we can optimize the performance of both the EHR and patient-center care initiatives.
SETMA’s participation in the Center’s proposed study will be based on:
- SETMA’s idea of the future of healthcare
- SETMA’s Model of Care
- SETMA’s continued efforts to remodel healthcare delivery to fulfill the promise and ideal of patient-centered medical home
These are briefly described below.
The Future of Healthcare
Efforts to reform healthcare may fail unless they employ three elements upon which SETMA depends in its transformative efforts:
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of “Medicare Advantage”.
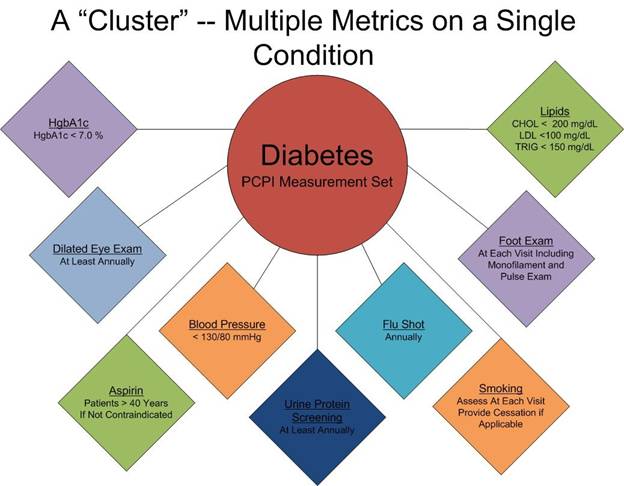
At the core of these principles is SETMA’s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery. SETMA employs two definitions in this analysis::
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that Fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics at the point-of-care can and will change outcomes.
The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may have as many as 60 or more quality metrics fulfilled in his/her care which WILL change the quality of outcomes.

SETMA’s model of care is based on these three principles and these concepts of “clusters” and “galaxies” of quality metrics. We are achieving significant results with them.
Contrasting SETMA’s “model of care” with the other organizations participating in the Center’s study will allow SETMA and the Center to understand the processes of healthcare transformation more fully.
The SETMA Model of Care
- The tracking by each provider on each patient of their performance on preventive care, screening care and quality standards for acute an chronic care. SETMA’s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provider.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool plans of care and the medical home coordination document summaries a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Permanence Improvement (QAPI) Initiatives – this year SETMA’s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a COGNOS Report which allows us to analyze our hospital care carefully.
The SETMA Model Detailed
The SETMA Model Step I -- Provider Performance Tracking
The Physician Consortium for Performance Improvement (PCPI) is an organization created by the AMA, CMS, Institute of Medicine and others to develop measurement sets for quality assessment. The intent is to allow healthcare providers to evaluate their own performance at the time they are seeing a patient. SETMA is tracking a number of these measurement sets including: Chronic Stable Angina, Congestive Heart Failure, Diabetes, Hypertension, and Chronic Renal Disease Stages IV through ESRD, Adult Weight Management, and Care Transitions. Others will be added overtime. The details of these measurement sets and
SETMA’s provider performance on each can be found at www.jameslhollymd.com under Public Reporting PCPI.
In addition to Provider Performance Tracking tools such as those produced by PCPI, the National Quality Foundation (see www.jameslhollymd.com under Public Reporting NQF), and National Committee for Quality Assurance (see www.jameslhollymd.com under Public Reporting HEDIS and/or NCQA), SETMA has designed a pre-visit quality measures screening and preventive care tool. This allows a SETMA provider and a patient to quickly and easily assess whether or not the patient has received all of the appropriate preventive health care and the appropriate screening health care which national standards establish as being needed by this patient. The following is the Pre-visit Preventive Screening tool. All measures in black apply to the current patient and are fulfilled. All measures in red apply to the current patient and have not been fulfilled and all measures in grey do not apply to the current patient. If a point of care is missing, it can be fulfilled with the single click of a single button.
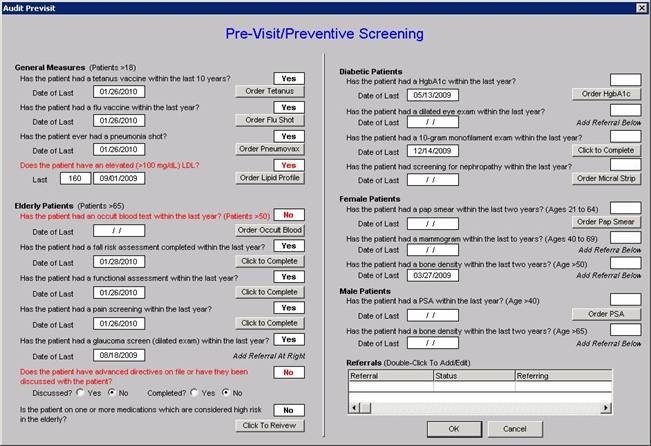
There are similar tracking tools for all of the quality metrics which SETMA providers track each day. The following is the tool for NQA measures:

The providers’ compliance with these measures are color coded for quick reference. The “view” button allows the provider to quickly review the content of the metric and to review the patient’s results.
Passing the Baton
While healthcare provider performance is important for excellent care of a patient’s health, there are 8,760 hours in a year. A patient who receives an enormous amount of care in a year is in a provider’s office or under the provider’s direct care less than 60 hours a year. This makes it clear that the patient is responsible for the overwhelming amount of their own care which includes compliance with formal healthcare initiatives and with lifestyle choices which support their health.
If responsibility for a patient’s healthcare is symbolized by a baton, the healthcare provider carries the baton for .68% of the time. That is less than 1% of the time. The patient carries the baton 99.22% of the time. The coordination of the patient’s care between healthcare providers is important but the coordination of the patient’s care between the healthcare providers and the patient is imperative. (For more on this concept see: Passing the Baton: Effective Transitions in Healthcare Delivery By James L. Holly, MD Your Life Your Health The Examiner March 12, 2010 at www.jameslhollymd.com). The following is a direct quote from this article. The emphasis and italics appear in the original:
“Often, it is forgotten that the member of the healthcare delivery team who carries the ‘baton’ for the majority of the time is the patient and/or the family member who is the principal caregiver. If the ‘baton’ is not effectively transferred to the patient or caregiver, then the patient’s care will suffer.”
The SETMA Model – Step 2 -- Auditing of Provider Performance – SETMA’s COGNOS Project
The creating of quality measures is a complex process. That is why it is important for agencies such as the Ambulatory Care Quality Alliance (AQA), the NCQA, the NQF, the Physician Quality Reporting Initiative (PQRI) and PCPI, among others, to identify, endorse and publish quality metrics. The provider’s ability to monitor their own performance and the making of those monitoring results available to the patient is important, but it only allows the provider to know how they have performed on one patient. However, the aggregation of provider performance over his/her entire panel of patients through an auditing tool carries the process of designing the future of healthcare delivery a further and a critical step. The problem with most auditing results, such as HEDIS, is that it is presented to the provider 12 to 18 months after the fact. SETMA believes that “real time” immediate auditing and giving of the audit results to providers can change provider behavior and can overcome “treatment inertia.”
Auditing of provider performance allows physicians and nurse practitioners to know how they are doing in the care of all of their patients. It allows them to know how they are doing in relationship to their colleagues in their clinic or organization, and also how they are performing in relationship to similar practices and providers around the country.
As a result, SETMA has designed auditing tools through the adaptation to healthcare of IBM’s business intelligence software, COGNOS. Multiple articles on SETMA’s COGNOS Project can be found at www.jameslhollymd.com under Your Life Your Health and the icon COGNOS. Those discussions will not be repeated here but auditing is an indispensable tool for the improvement of the quality of healthcare performance and for improvement in the design of healthcare delivery.
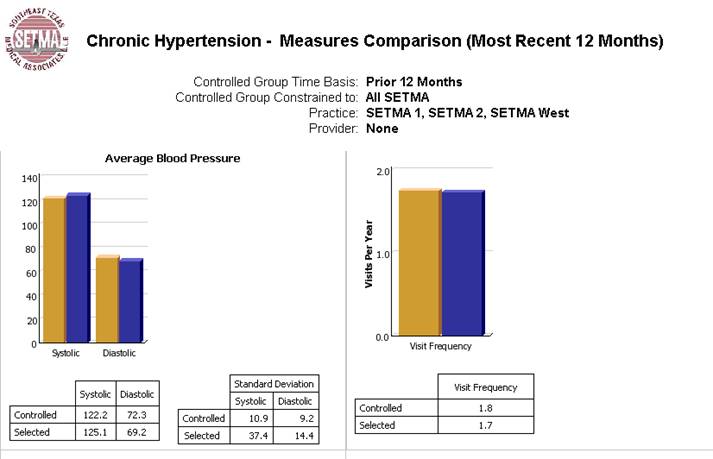
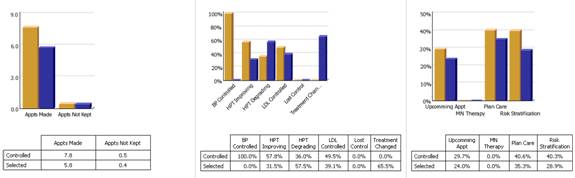
The following are a few examples of the auditing SETMA does of provider performance.
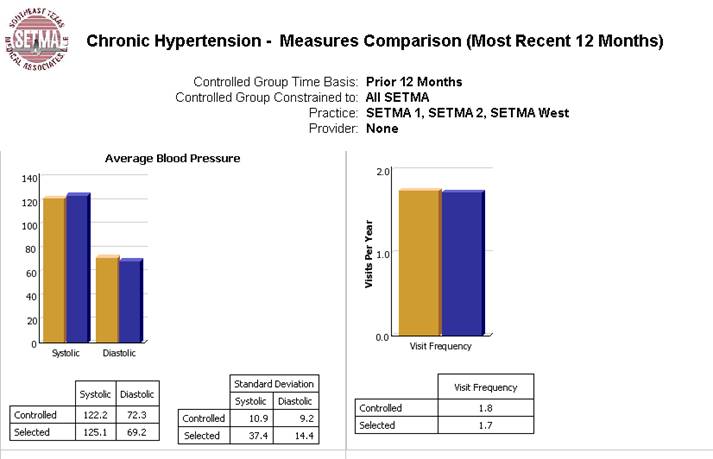
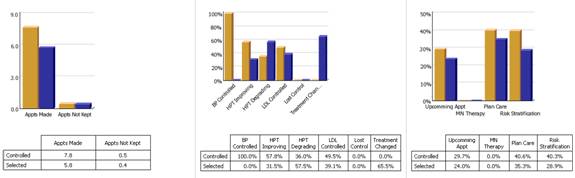
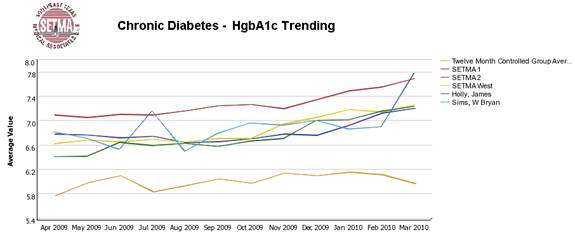
Through COGNOS, SETMA is able to display outcomes trending which can show seasonal patterns of care and trending comparing one provider with another. It is also possible to look at differences between the care of patients who are treated to goal and those who are not. Patients can be compared as to socio-economic characteristics, ethnicity, frequency of evaluation by visits and by laboratory analysis, numbers of medication, payer class, cultural, financial and other barriers to care, gender and other differences. This analysis can suggest ways in which to modify care in order to get all patients to goal.
Using digital dashboard technology, SETMA analysis provider and practice performance in order to find patterns which can result in improved outcomes practice wide for an entire population of patients. We analyze patient populations by:
- Provider Panel
- Practice Panel
- Financial Class – payer
- Ethic Group
- Socio-economic groups
We are able to analyze if there are patterns to explain why one population or one patient is not to goal and others are. WE can look at:
- Frequency of visits
- Frequency of testing
- Number of medications
- Change in treatment
- Education or not
- Many other metrics
We are able to present over-time patient results comparing:
- Provider to practice
- Provider to provider
- Provider current to provider over time
- Trending of results to see seasonal changes, etc.
The SETMA Model – Step 3 -- Analysis of Provider Performance through Statistics
Raw data can be misleading. It can cause you to think you are doing a good job when in fact many of your patients are not receiving optimal care. For instance the tracking of your average performance in the treatment of diabetes may obscure the fact that a large percentage of your patients are not getting the care they need. Provider Performance at the point of service is important for the individual patient. Provider Performance over an entire population of patients is important also. However, until you analyze your performance data statistically, a provider will not know how well he or she is doing or how to change to improve the care they are providing..
Each of the statistical measurements which SETMA tracks, the mean, the median, the mode and the standard deviation, tells us something about our performance. And, each measurement helps us design quality improvement initiatives for the future. Of particular, and often, of little known importance is the standard deviation.
From 2000 to 2010, SETMA has shown annual improvement in the mean (the average) and the median results for the treatment of diabetes. There has never been a year when we did not improve. Yet, our standard deviations revealed that there were still significant numbers of our patients who are not being treated successfully. Even here, however, we have improved. From 2008 to 2009, SETMA experience a 9.3% improvement in standard deviation. Some individual SETMA providers had an improvement of over 16% in their standard deviations. Our goal for 2010 is to have another annualized improvement in mean and in median, and also to improve our standard deviation. When our standard deviations are below 1 and as they approach .5, we can be increasingly confident that all of our patients with diabetes are being treated well.
An example of a statistical analysis of SETMA’s diabetes care in regard to the elimination of ethnic disparities of care is given in the article Eliminating Ethnic Disparities in Diabetes Care Your Life Your Life Your Health The Examiner May 13, 2010, which is posted on our website at www.jameslhollymd.com.
The SETMA Model – Step 4 -- Public Reporting of Provider Performance
One of the most insidious problems in healthcare delivery is reported in the medical literature as “treatment inertia.” This is caused by the natural inclination of human beings to resist change. Often, when patients’ care is not to goal, no change in treatment is made. As a result, one of the auditing elements in SETMA’s COGNOS Project is the assessment of whether a treatment change was made when a patient was not treated to goal. Overcoming “treatment inertia” requires the creating of an increased level of discomfort in the healthcare provider and in the patient so that both are more inclined to change their performance. SETMA believes that one of the ways to do this is the public reporting of provider performance. That is why we are publishing provider performance by provider name at www.jameslhollymd.com under Public Reporting.
A more complete explanation of SETMA’s philosophy and intent in “public reporting” of provider performance can be found in the following articles:
- Transforming Healthcare Public Reporting of Provider Performance on Quality Measures Your Life Your Health December 3, 2009;
- Patient-centered Medical Home SETMA’s COGNOS Project Changing Patient and Provider Behavior Your Life Your Health October 29, 2009.
- County Health Rankings – Part II Quality of Care – What Will Be Gained by Public Reporting Your Life Your Health March 4, 2010
The SETMA Model – Step 5 -- QAPI – Quality Assessment and Performance Improvement
Quality Improvement Initiatives based on tracking, auditing, statistical analysis and public reporting of provider performance are critical to the transformation of healthcare both as to quality of care and as to cost of care.
With the above described data in hand and with the analysis of that data, it is possible to design quality initiatives for future improvement in care. Currently SETMA is designing two major quality initiatives. One is for diabetes. It is an attempt to eliminate the last vestiges of ethnic disparity in the care of diabetes. This will require the use of additional internal resources and attention but it is our intent to do so and to permanently and totally eliminate ethnic disparities. The other is in regard to decreasing avoidable readmissions to the hospital.
The details of these two initiatives can be reviewed at www.jameslhollymd.com :
- Designing a Quality Initiative: How? Hospital Re-admissions Your Life Your Health April 22, 2010.
- Eliminating Ethnic Disparities in Diabetes Care Your Life Your Life Your Health May 13, 2010
Without a systems approach to healthcare, each of these steps are impossible; certainly, the analysis and transformation of healthcare is impossible. With a systems approach, this logical and sequential process is possible and rewarding for provider and patient. This process has set SETMA on a course for successful and excellent healthcare delivery. Our tracking, auditing, analysis, reporting and design will keep us on that course.
SETMA’s Model of Care has and is transforming our delivery of healthcare, allowing us to provide cost-effective, excellent care with high patient satisfaction. This Model is evolving and will certainly change over the years as will the quality metrics which are at its core.
SETMA’s Continuing Efforts to Leverage Electronic Patient Management Tools to Fulfill the Promise of Patient-Centered Medical Home
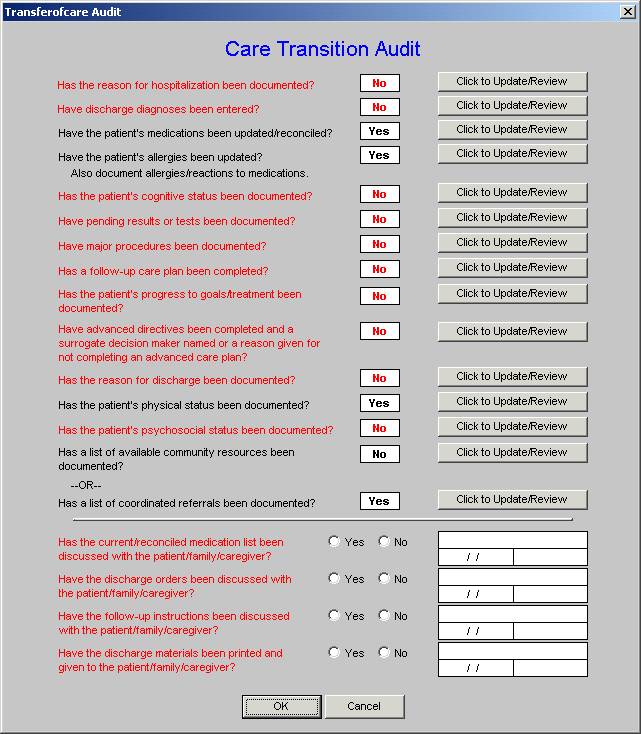
These are too numerous to include in this brief review but four will illustrate this effort. First, SETMA is collaborating with the National Quality Forum and others to identify quality measures in order to perform and then to evaluate the “care transitions” required to maintain quality care between hospital/outpatient, emergency department/community care, clinic/home and others.
The following is one example of the process and outcomes metrics in this area of patient-centered care. This is an auditing tool currently being used in the hospital when the patient is discharged.
The second, third and fourth of these efforts involved “follow-up call” scheduling:
- The day following discharge from the hospital – this goes to follow-up call nursing staff in our Care Coordination Department. These calls differ from the “administrative calls’ initiated by the hospital which may last for 30 seconds are less. These calls last from 12-30 minutes and involved detailed discussions of patient’s needs and conditions.
- At a provider-designated time following a clinic visit – these calls, scheduled by the provider at the time of care can be for any interval of time (1-60 days or more) and define what the call is for. The result of the call is reported back to the provider. These calls last for 12-30 minutes and additional follow-up calls or visits can be scheduled as needed
- A coordination of care call – at a clinic visit, telephone contact with a patient, hospital or emergency department visit, etc., a referral document allows for a notice to be sent to the Director of SETMA’s Department of Care Coordination when issues exist which will impact the patient’s care, such as financial needs, safety issues, adherence to treatment plan, etc.
The following is an illustration of these functions. This one relates to Hospital Discharge Follow-up Call.
Undergirding all of this is SETMA’s commitment to making certain that our patients have access to care and that they can afford that care. As a result, SETMA founded The SETMA Foundation through which care can be obtained for our patients are either uninsured or who cannot afford co-pays, medications, etc. To this end, the partners of SETMA have contributed $1,000,000 to the foundation in the past two years.
We expect that the proposed project will help us and other health systems understand how we might move more quickly and effectively in leveraging our EHR investment to advance patient-centered care.
We look forward to working with your research team on this very worthwhile project.
Sincerely
James L. Holly, MD
CEO, SETMA, LLP
www.jameslhollymd.com
PS: All of SETMA’s electronic patient management tools are displayed on SETMA’s website at www.jameslhollymd.com .
|