|
July 30, 2014
By James L. Holly, MD
Basics:
- Who are you nominating for the Texas Health Champion Award?
- Name of nominee
Southeast Texas Medical Associates, LLP (SETMA, LLP)
- Nominee Information (name/org, phone number, e-mail, mailing address, website)
- Region the nominee served to reduce the burden and/or raise awareness of obesity.
Region/Multiple Cities or counties (Golden Triangle: Jefferson, Hardin, Orange, Liberty and Chambers Counties)
- How long has the nominee served to reduce the burden and/or raise awareness of the obesity epidemic in Texas?
- What categories of obesity prevention/awareness does the nominee focus on in his/her work? Check all that apply.
- Obesity Prevention for children and youth
- Obesity Prevention for adults
- Physical Activity
- Your (nominator) name and contact information (name/org. phone number, email, mailing address, website - please also indicate if this is a self-nomination)
James L. Holly MD, Contact information - all the same as above; self nomination
- How do you rate the nominee’s efforts to mobilize and/or collaborate with the community to promote health living?
Please provide support with specific examples for how the nominee has mobilized and/or collaborated with the community to promote healthy living.
Southeast Texas Medical Associates, LLP (www.jameslhollymd.com) is a multi-specialty medical group with offices in Beaumont, Orange, Port Arthur and Lumberton, Texas. The following is a pictorial description of SETMA’s six locations and information about our use of Electronic Patient Management, Patient-Centered Medical Home, Health Information Exchange, National Quality Standards, Secure Patient Web Portal, and Transparency at www.jameslhollymd.com.

Founded in August, 1995, SETMA was formed from four practices which had been in Southeast Texas since 1976. In 1997, SETMA determined to purchase and deploy an electronic medical record (EMR) system, which was purchased in 1998. It was deployed in January, 1999.
By May, 1999, SETMA realized that EMR was an inadequate goal. If all the EMR provided was the ability to document a patient encounter electronically, it was too expensive and too hard to justify the cost and effort. SETMA changed its goal to an electronic patient management (EPM) system and began developing clinical decision support, disease management tools and electronic analytics capacity. We began to emulate Abraham Lincolns famous state, “If we first know where we are and know whither we are tending, we can better know where we want to go and how to get there.
As we developed disease management tools, we realized that at the root of every illness and at the root of excellent health were three disciplines. They were: “lose weight,” “exercise,” and “stop smoking.” Therefore, SETMA developed The LESS Initiative, which is described and explained in SETMA's LESS Tutorial. Published on our website, this and all of SETMA’s information is free to all healthcare providers.
In 1998, SETMA began using our weekly newspaper column, which has been published for the past sixteen years to promote healthy living, focusing on the elements of The LESS Initiative. Those articles can be found at LESS Initiative. After a critical, peer-reviewed examination of The LESS Initiative, in 2007, the Agency for Healthcare Research and Quality published SETMA’s LESS Initiative on the AHRQ Innovation Exchange recommending its adoption by other medical practices across the nation.
The AHRA deployment can be reviewed at: Multispecialty Practice Uses Electronic Templates to Provide Customized Support at Every Visit, Contributing to Improved Patient Behaviors and Outcomes. There is also extensive evidence in the medical literature in support of The LESS Initiative; the following link offers some of that evidence: Less Initiative: SETMA's Initiative Confirmed by Medical Journals. SETMA’s LESS Initiative was also awarded eHealth’s Innovator Award of the year in 2012.
Childhood Nutrition for a Lifetime of Health
In addition to an adult weight management assessment and education, SETMA focused on childhood nutrition as a foundation for a life-time of health. (See Childhood Nutrition: The Foundation for a Lifetime of Health).
Increasingly, SETMA focused on weight management as an integral part of primary care healthcare practice.
The following is a link to many of the articles SETMA published on weight loss. Early in this work, the following were published and used in the education of our patients:
In February, 2001, SETMA published an article which identified seven principles for weight management, those principles can be found at: Obesity: Weight Reduction In 2004, the American Medical Association published a 220-page program for adult weight management. They sent SETMA the first 30 copies of this. While the content was excellent, the format was awkward to use. For ease of use, SETMA reduced the 220-page work to an electronic version which can be used in daily medical practice. SETMA’s tutorial for using this clinical decision support and disease management tool is entitled, Adult Weight Management, and can be reviewed at Adult Weight Management Tutorial. One year after developing the electronic version, SETMA made a two-hour presentation to the seven AMA staff who developed the Adult Weight Management tool. Their response to our work was amazement; they said, “This is incredible, but it is obvious that this would have to be used in a tertiary medical center which focuses on obesity. We responded, we use it every day with every patient.
In addition to the tools for weight management and for The LESS Initiative, SETMA has developed the following tools which are published on our website and which are free for any practice to adopt. They are:
Dietary Education
SETMA also operates an American Diabetes Association accredited Diabetes Self-Management Diabetes Education (DSME) department which also operates a Medical Nutrition Therapy (MNT) section. That section has classes for Dietary Approach to Stop Hypertension (DASH), Renal Disease Diet and weight management education.
- How do you rate the nominee’s efforts to include underserved populations in their programming and decision making?
Excellent
Please provide support with specific examples for how the nominee has included underserved populations in their work.
All patients seen at SETMA have The LESS Initiative completed at each visit and this particularly includes weight management evaluations. This includes all patients who are insured by:
- Medicare Advantage -- HMO Medicare patients. In 2002, we requested that the HMO reduce the co-payment for primary care to zero. The reason was that we have many patients who could not afford a $15, $10 or $5 co-pay. This represented a significant barrier to access to care for these patients which represent about one-third of SETMA’s patients.
- Medicare Fee-For-Service - These patients have traditional, fee-for-service Medicare.
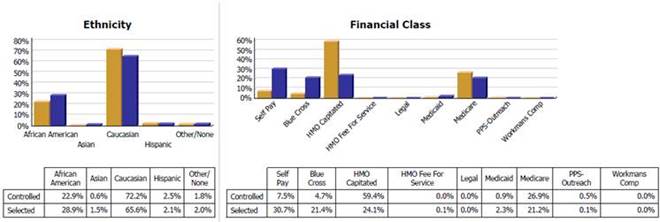
In our data analytics, as shown below, we found that our HMO patients with a zero co-pay and therefore no economic barriers to access to care are actually getting better care than our Fee-for-Service Medicare patients
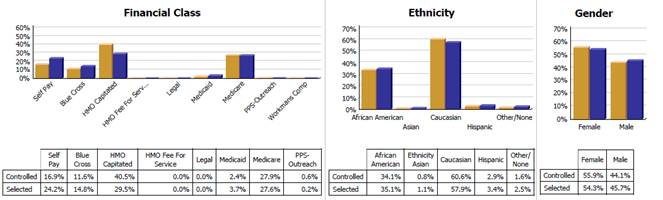
From the above, we found that our HMO capitated patients, who have zero co-pays for office visit are treated more effectively than Fee-for-Service Medicare, allowing the inference that the our-of-pocket cost for the FFS Medicare patients is a barrier to effective care, in that, when that barrier is removed in a similar population the care improves.
Our data also shows that we have eliminated ethnic disparities for patients with diabetes. The LESS Initiative is critical in this process.
Analytics in Primary Health Care
Population Health
The following audit shows that we have not eliminate ethnic disparities in care of patients with dyslipidemia. We believe this is cultural and we are working on it. We see once again that our Medicare Advantage patients (HMO) are better treated that our Medicare FFS patients.
- Medicaid
- Uninsured Patients
SETMA’s partners annually contribute $500,000 to The SETMA Foundation through which we provide financial support for our patients who cannot afford care. None of that money can benefit SETMA. All patients receiving Foundation support are treated free by SETMA. The money is used to pay for care from physicians who will not see our patients without being paid and/or for medications and other services.
As a Patient-Centered Medical Home (PC-MH), accredited by NCQA (2010-2016), AAAHC (2010-2017), URAC (2014-2017) and The Joint Commission (2014-2017), our care for under-insured, uninsured, and indigent patients is part of our mission statement. The following stories and ideals show our care for patients who are otherwise unable to obtain care.
The Story and the Ideals of PC-MH
- How do you rate the nominee’s ability to create a model or process for healthy living that can be replicated elsewhere in Texas or the rest of the country?
Please provide support with specific examples for how the nominee
has created a model or process for healthy living that can be replicated.
Everything SETMA does is based upon philosophical principles and foundations
In March, 2014, SETMA underwent a three-day survey by The Joint Commission in SETMA’s pursuit of Joint Commission accreditation for ambulatory care and for patient-centered medical home. One of their observations relates to our creation of a model for healthy living which can be replicated and which is sustainable. That observation is that both surveyors and one of the executives at The Joint Commission commented about the philosophical foundation of SETMA’s work.
On Wednesday afternoon (March 5, 2014) I called my executive contact at The Joint Commission, he said “I was just talking to one of my colleagues and showing him SETMA’s Leadership notebook (Prepared in response to the Commission’s Standards and Requirements Chapter Seven o leadership).” The executive said, “Look at this; everything they do is founded upon a philosophical foundation. They know ‘what they are doing,’ but more importantly, they know why they are doing it.’”
SETMA is not the result of random efforts but of innovations and advances which are consistent with a structured set of ideals, principles and goals. This foundation is one of the strengths of SETMA and it is one of the principle guides to SETMA’s development history, i.e., what caused SETMA to become what it is.
The Conclusion of the Robert Wood Johnson Foundation Team
In October, 2012, a team from the MacColl Institute visited SETMA. This visit was part of a Robert Wood Johnson Foundation funded research project entitled Learning from Exemplary Ambulatory Practices. At the conclusion of a three-day visit, two of the conclusions of the team relate to SETMA’s creation of a model for the replication of healthy living which is sustainable.
“Learning Team - they believe that the spontaneous and structured learning of SETMA allows us to continually and almost unintentionally learn and grow. They understand that learning, as Senge says, is only distantly related “to taking in more information.” They believe that we have incorporated “systems thinking” and “systems structures” into SETMA extremely well. They think this is one of the most value aspects of SETMA’s work force and work flow innovations. They were able to attend one of SETMA’s monthly training meetings and were intrigued by the enthusiastic and engaged participation by all of SETMA’s healthcare providers.
The fifth area of uniqueness of SETMA identified by the RWJF team was a surprise to them; it was SETMA’s IT Department. The team felt that SETMA has approached healthcare transformation differently than anyone they have seen. They related that uniqueness to the decision we made in 1999 to morph from the pursuit of “electronic patient records” to the pursuit of “electronic patient management.” They were surprised to see how centrally and essentially electronics are positioned into SETMA and how all other things are driven by the power of electronics. They marveled at the wedding of the technology of IT with clinical excellence and knowledge. The communication and integration of the healthcare team through the power of IT is novel, they concluded.
An Inconvenient Reality - without Humanity Science is Helpless
It may be an inconvenient reality but science is not the foundation of transformation. The tension which exists between technology and humanity is why technology must always be subservient to humanity. Yet, that subservience does not emasculate or eliminate the power of technology. Through acknowledging truth, privately and publicly, we empower sustainable change, making analytics a critical aspect of healthcare transformation. But the balance which humanity brings to the equation is that in the midst of health information technology innovation, we must never forget that the foundations of healthcare change are ‘trust’ and ‘hope.’ Without these, science is helpless!
Transformation will require the reestablishment of the trust which once existed between provider and patient. That cannot be done by fiat. Patients must be absolutely confident that they are the center of concern and of care. Patients must also know that they are principally responsible for their own health. These concepts are the genius behind Patient-Centered Medical Home and this trust cannot be achieved by regulations, restrictions and rules.
The tools of transformation may actually begin with the same ideals and goals as reformation, but now rather than attempting to impose the changes necessary to achieve those ideals and goals, a transformative process initiates behavioral changes which become self-sustaining, not because of rules, regulations and restrictions but because the images of the desired changes are internalized by the organization which then finds creative and novel ways of achieving those changes.
The currently proposed reformation of the healthcare system does nothing to address the fact that the structure of our system is built upon a "patient" coming to a healthcare provider who is expected to do something "for" the patient. The expectation by the system and by the recipient of care is that something is going to be done "to" or "for" the patient in which process the patient is passive. There is little personal responsibility on the part of the patient for their own healthcare, whether as to content, cost or appropriateness. The healthcare provider is responsible for the health of the patient.
Transformation of healthcare would result in a radical change in relationship between patient and provider. The patient would no longer be a passive recipient of care given by the healthcare system. The patient and provider would become an active team where the provider would cease to be a constable attempting to impose health upon an unwilling or unwitting patient. The collaboration between the patient and the provider would be based on the rational accessing of care. There would no longer be a CAT scan done every time the patient has a headache. There would be a history and physical examination and an appropriate accessing of imaging studies based on need and not desire.
This transformation will require a great deal more communication between patient and provider which would not only take place face-to-face, but by electronic or written means. There was a time when healthcare providers looked askance at patients who wrote down their symptoms. The medical literature called this la maladie du petit papier or "the malady of the small piece of paper." Patients who came to the office with their symptoms written on a small piece of paper where thought to be neurotic. No longer is that the case. Providers can read faster than a patient can talk and a well thought out description of symptoms and history is an extremely valuable starting point for accurately recording a patient's history. Many practices with electronic patient records are making it possible for a patient to record their chief complaint, history of present illness and review of systems, before they arrive for an office visit. This increases both the efficiency and the excellence of the medical record and it part of a transformation process in healthcare delivery.
Common Prejudice of Technology
This transformation will require patients becoming much more knowledgeable about their condition than ever before. It will be the fulfillment of Dr. Joslin's dictum, "The person with diabetes who knows the most will live the longest." It will require educational tools being made available to the patient in order for them to do self-study. Patients are already undertaking this responsibility as the most common use of the internet is the looking up of health information. It will require a transformative change by providers who will welcome input by the patient to their care rather seeing such input as obstructive.
This transformation will require the patient and the provider to rethink their common prejudice that technology - tests, procedures, and studies - are superior methods of maintaining health and avoiding illness than communication, vigilance and "watchful waiting." Both provider and patient must be committed to evidence-based medicine which has a proven scientific basis for medical-decision making. This transformation will require a community of patients and providers who are committed to science. This will eliminate "provider shopping" by patients who did not get what they want from one provider so they go to another.
The Critical Balance in 21st Century Healthcare is that technology must never blind us to the human€¦In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology.
Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the ‘health problems’ we face. It is my judgment that the major issue facing healthcare delivery today is that men and women, boys and girls have replaced the trust they once had in their physician with a trust in technology.
The challenge for our new generation of healthcare providers and for those of us who are finishing our careers is that we must be technologically competent while at the same time being personally compassionate and engaged with our patients. This is not easy because of the efficiency (excellence divided by time) of applied technology. A referral or a procedure is often faster and more quantifiable than is a conversation or counseling.
As we move deeper into the 21st Century, we do so knowing that the technological advances we face are astounding. Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to true healthcare.”
The uniqueness of SETMA’s team approach may be that we recognize, respect and welcome the collegial partnership with nurses, nurse practitioners and others who traditionally worked “for” physicians rather than working “with” them in a collegial, collaborative, team approach to healthcare.
The Model
Combining technology and humanity, each patient is treated as an individual but with standards and elements which are universally applied to all who are seen by SETMA, i.e., an entire population. The elements of the patient’s evaluation in regard to weight management are based on the philosophy that:
- Every encounter with a patient should be evaluational and educational, i.e., the patient’s current health status should be evaluated and established and the patient should learn how to participate in their healthcare. These are expressions of the PC-MH principles of patient activation, patient engagement and shared-decision making.
- The tool of this process is the “Baton,” which is a written, personalized, statement of the patient’s plan of care and treatment plan. This recognizes that while the patient may be seen by a healthcare provider for twenty hours a year, and that is a great deal of care, there are 8,760 hours in a year. That means that the patient is responsible for their care for the overwhelming majority of the time.
The following is the patient vital sign template; all of the above named measurements are captured in these structured fields. A green box is placed around the BMR which is automatically calculated for the provider and patient.
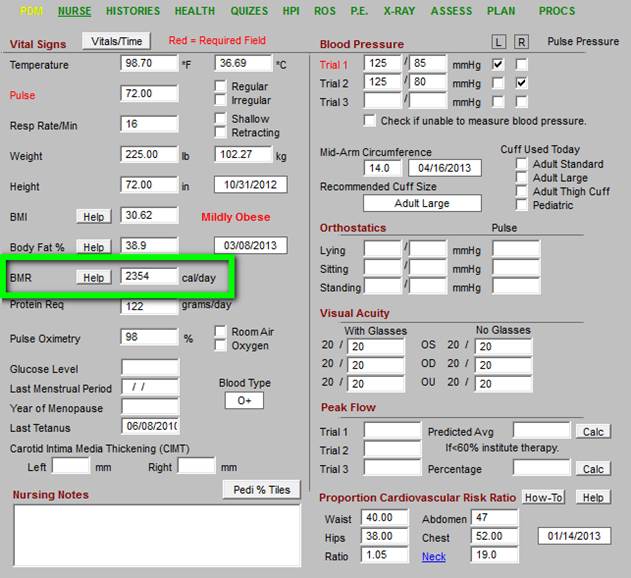
The above is the evaluation of the patients. The following is the education of the patient concerning how they can change their BMR. As will be seen below in a discussion of SETMA’s weight management tool, caloric intake is an important part of weight management. However, because of the very low number of calories required daily to maintain a pound of fat, the majority of patients cannot not lose weight and maintain weight loss without changing their activity.
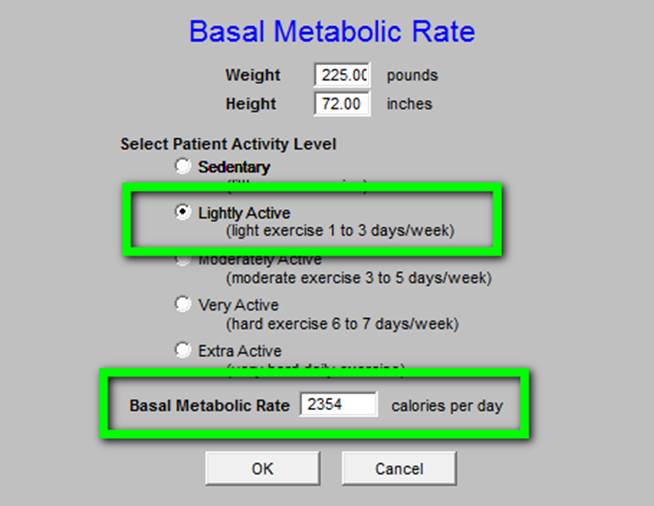
SETMA patients are taught that the BMR is a calculation based on three things: height, weight and activity. In the patient example given below a patient who is 72 inches tall and who weighs 225 pounds and who is physically inactive or sedentary, has a BMR of 2054 daily caloric requirements. In that a pound of fat has approximately 3,500 calories of energy in that pound, in order to lose that pound of fat, the patient has to decrease their energy intake by a total of 3,500 calories. However, it only takes about 4 calories a day to maintain a pound of fat. Therefore, if you are overweight by 100 pounds of fat, it only takes 400 calories a day to sustain those 100 pounds of weight. The disheartening thing is that two large apples provide 400 calories. Therefore, simply by decreasing intake, which is part of weight management, it is hard to lose weight.
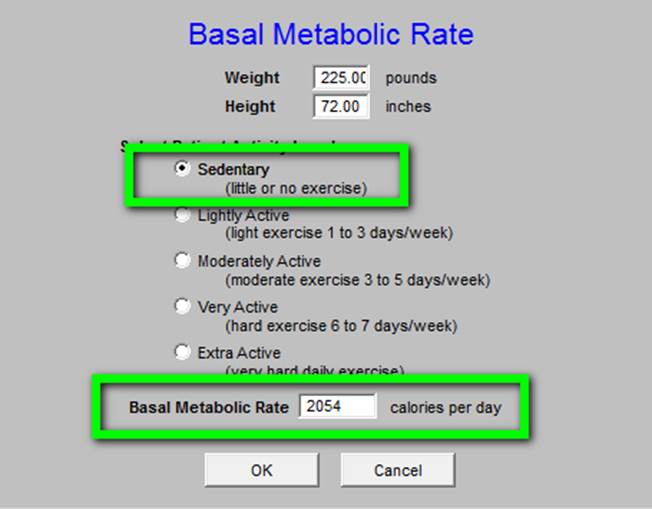
But, if a patient begins “light activity,” which is defined as 1-3 days a week of walking for 30 minutes, their BMR goes up by 300 calories a day.
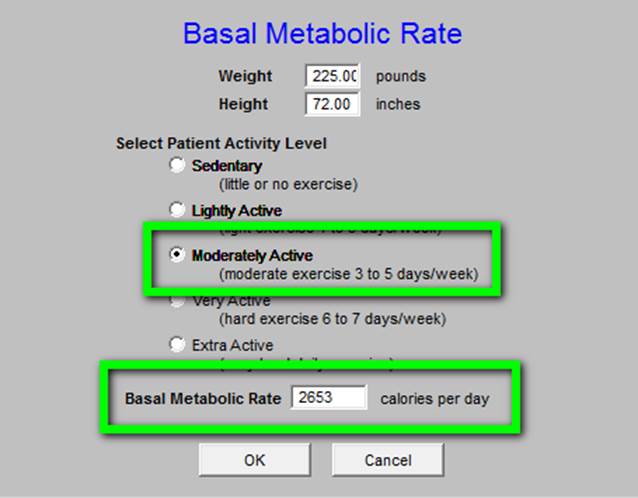
“Moderate activity” increases the BMR by 500 calories a day. Walking three miles a day in 45 minutes 3-5 days is moderate activity.
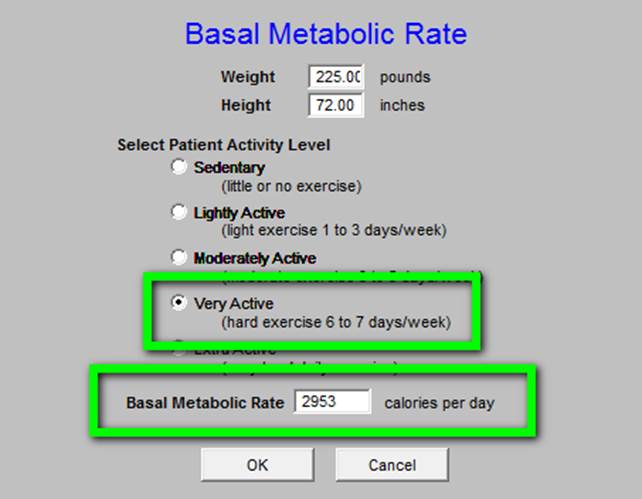
“Very active” lifestyle would increase the BMR by 900 calories a day. At SETMA patients are encouraged to begin an exercise program which is sustainable, i.e., being a tortoise rather than a hare. Few patients will maintain a very active or extra active level of activity, but if they did the energy metabolism benefits are enormous.
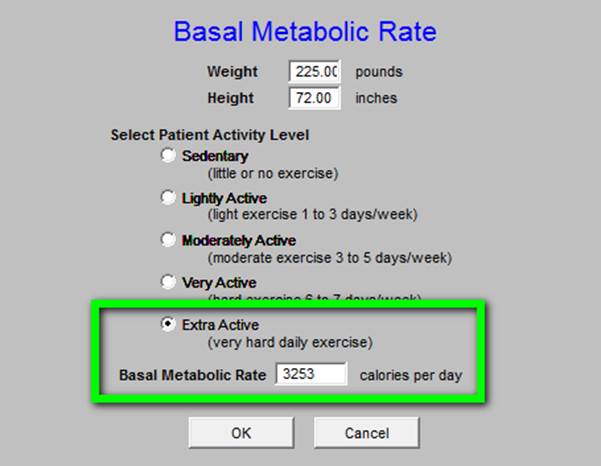
As can be seen with this educational tool “extra active” levels of exercise, while rigorous, have a big payoff, i.e., 1200 calories a day.
Once individual begin to learn that daily energy consumption is a function of their weight and height and of their activity, they are able to determine what their weight reduction plan should be. Couple with weight management and a personalized exercise prescription which is also part of The LESS Initiative; patients can sustain a weight management program of their own.
The above tool is a part of the routine medical examination. The second part of SETMA’s weight management program is the completion of The LESS Initiative program itself. The tutorial for The LESS can be found at http://jameslhollymd.com/epm-tools/Tutorial-LESS.
The below template is the master Less Initiative template.
While it may appear to be complex, it actually takes about thirty seconds for the nurse to complete. The LESS document is then printed on laser printers in each examination room. It takes two seconds to create the LESS Document and another few seconds to print the document. The length of the document is:
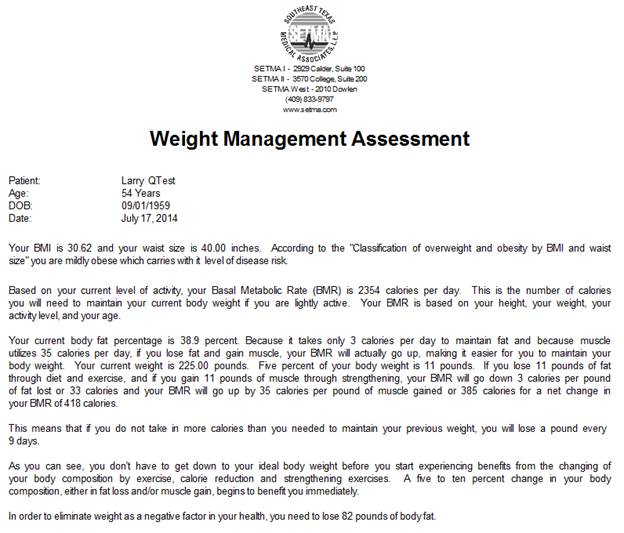
- Weight Management Assessment - one page. The complete Weight Management took can be found at Adult Weight Management Tutorial.
- Personalized Exercise Prescription - eight pages. While Exercise is a part of the LESS a specific tutorial for exercise can be found at Exercise Prescription Tutorial.
- Stop Smoking (only given to patients who smoke or chew tobacco or who are expose to secondary or tertiary tobacco) - six pages. While Stop Smoking is a part of The LESS, a specifi tutorial for Smoking Cessation can be found at Smoking Cessation Tutorial.
A reviewer may think, this is too much material for a patient to read and understand, but SETMA’s experience is that if you give patient’s education material which has their data on each page and their name on each page, i.e. it is personalized, no matter how long, they read it.
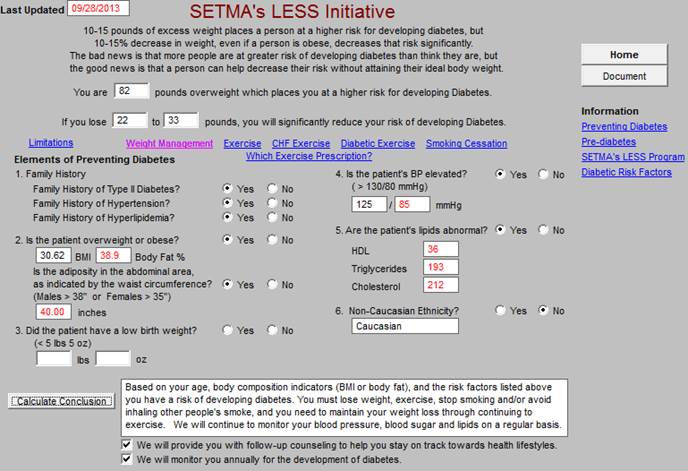
Perhaps the key to the success of the LESS Initiative as far as Weight Management is the bad news and the good news at the top which stats:
- BAD NEWS: there is reason for concern -- 10-15 pounds of excess weight places a patient at higher disease risk.
- GOOD NEWS: there is reason for hope -- 10-15% decrease in weight, no matter how overweight or obese a patient is, significantly decreases their risk.
All of the data and all of the information in the data and information boxes on the template above are automatically populated.
The weight management part of The LESS Initiative comprises only this template. The entire weight management disease management tool can be review on the link above. It is use often by SETMA but not on every patient seen, as is The LESS. The co-morbidities of obesity which are denoted on the template below are done automatically and contribute to the disease risk. The Class of Weight, the Disease Risk Level, the Assessment and the Treatment recommended are populated automatically.
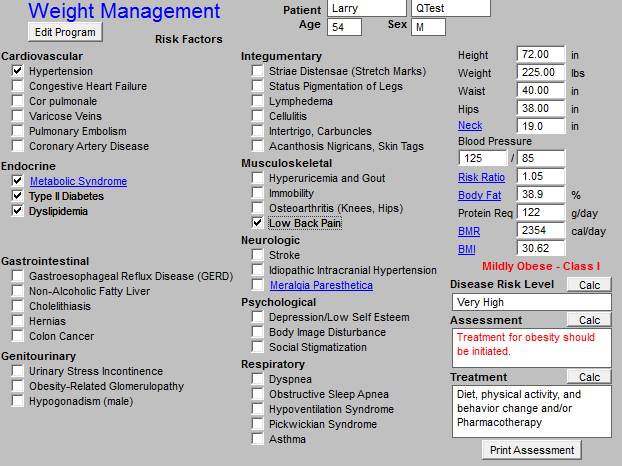
The following is the Weight Management Assessment and the Teaching Tool created as a result of the completion of the master weight management template.
The principles which have guided Southeast Texas Medical Associates’ development of a data base which supports these requirements are:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
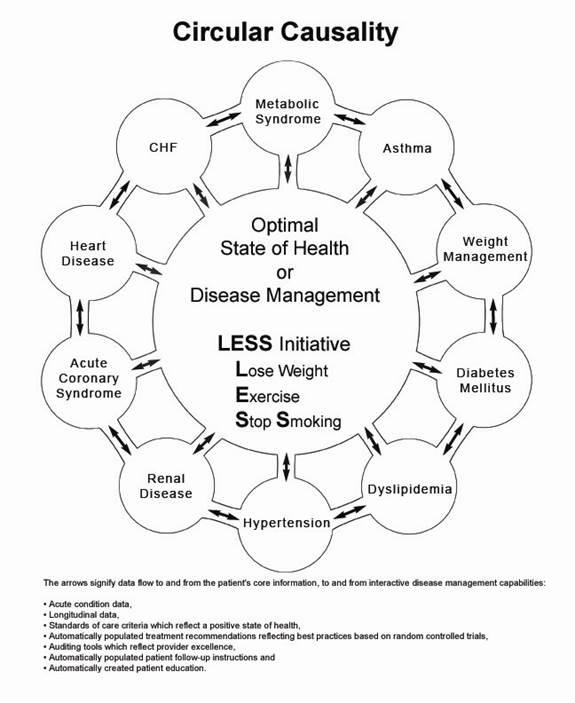
Reality in a biological system can only be effectively approached from a circular- causality platform which is designed to encourage and facilitate the dealing with complex, interrelated problem solving for maximal effectiveness. Schematically, this would be represented as follows.
- How do you rate the nominee’s efforts to use proven strategies (based on research or other evidence) to promote health and sustain their obesity prevention programming?
Please Provide Support with specific Examples for how the nominee has used proven strategies to promote and sustain their efforts.
- Identify and cultivate a passionate champion: Getting the program off the ground requires the relentless commitment of a respected individual who will not be satisfied until the program becomes a part of everyday practice.
- Leverage existing resources: Would-be adopters can build the program based on existing materials created by Southeast Texas Medical Associates, all of which can be obtained by contacting the program developer.
- Make public commitment: Southeast Texas Medical Associates leaders told patients, staff, and the community at large that the practice was committed to using its EMR to promote health-related behavior changes, thus creating accountability among key stakeholders.
- Ensure content focuses on realistic improvements: When creating content for the templates, emphasize the benefits of making modest, achievable changes. For example, make sure the templates are designed to urge a previously sedentary, obese individual to set realistic goals, such as exercising a few minutes a day (gradually increasing over time) and losing a few pounds. Telling this patient to strive for his or her ideal body weight or to exercise an hour a day would likely backfire because these goals will seem impossible to achieve.
- Set up system to personalize documents: The effectiveness of the written document depends in large part on the degree to which it is personalized for the patient. To that end, design the system to print the patient's first and last name and to incorporate patient-specific data and information on every page. (See the Story section for an anecdote that demonstrates the power of this personalized approach.)
- Constantly reinforce key messages: The key to effectively promoting behavior change lies in repetition. To that end, providers should complete the templates and provide an updated document at virtually every visit, and generally use each visit as an opportunity to educate and influence the patient.
- Audit and share data on provider adherence: To promote the repetition outlined above, monitor the degree to which nurses and physicians use the LESS templates at each visit. Southeast Texas Medical Associates regularly monitors and publicly shares clinician-specific adherence rates. This strategy has led to the templates being used more than 97 percent of the time, meaning that organizational leaders have achieved their goal of making LESS a routine, accepted part of everyday practice.
- How do you rate the nominee’s evaluation process to determine the impact of their personal or organizational work?
Please Provide support with specific examples for how the nominee
has evaluated the impact of their work or taken steps toward an evaluation
to assess their impact.
The program has contributed to a leveling off in the prevalence of overweight/obesity, above-average quit rates among smokers, better blood glucose control in those with diabetes, and fewer racial disparities in the care of some chronic conditions.
- No increase in overweight/obesity: An analysis of more than 32,000 patients seen by the clinic at least 6 times in the past 10 years found that average BMI has remained stable (rising only slightly, from 28.15 to 28.56). Similarly, the percentage of these patients with a BMI above 25 (the cutoff for being considered overweight) also remained stable, rising by only 0.49 percentage points (from 63.13 to 63.52 percent). This stabilization suggests the program has had a positive impact on weight management because it occurred as these individuals got older (BMI often increases with age), and during a time when rates of overweight/obesity rose for the nation as a whole. Although the LESS initiative cannot be considered solely responsible for this stabilization, program leaders believe it has been a major contributor due to its systematic, consistent focus on weight management and related behaviors at virtually every visit.
- Above-average quit rates: In the past 10 years, the LESS initiative has helped at least 2,767 patients quit smoking. In addition, at least 15 percent of the 3,209 smokers who have visited the practice at least twice in the last 2 years have quit permanently. (Actual quit rates are likely higher, as documentation of those who quit does not always occur.) This rate is well above the 7-percent or lower average quit rate among smokers who want to stop smoking but receive little or no assistance in doing so.8,9
- Better blood glucose control: Median hemoglobin A1c levels in patients with diabetes dropped from 7.78 percent in 2000 to 6.50 percent in 2008. Multiple initiatives (including disease management tools, a self-management education program, and an endocrinologist joining the practice) likely account for this decline, with the LESS initiative playing a supporting role.
- Fewer disparities in chronic care: The practice has virtually eliminated disparities in diabetes outcomes, with similar percentages of African-American and white diabetes patients having their blood glucose levels under control. The practice has made some (but less substantial) progress in reducing racial disparities in managing hypertension and high cholesterol. The LESS initiative has played a supporting role in reducing these disparities, primarily through its systematic emphasis on addressing health-related behaviors for every patient (regardless of race) at virtually every visit.
- How do you rate the nominee’s overall impact on obesity prevention?
Please Provide support with specific examples for how the nominee has made an impact on obesity or obesity risk factors in the larger community
SETMA was actively involved in the passing of a Beaumont City ordinance stopping the use of tobacco in any and all public places in Beaumont City limits. Other than dozens of newspaper articles, it is hard to attribute specific impacts on obesity and/or exercise to SETMA’s efforts.
- Please use the space below for additional comments or to provide links or citations for materials or publications that show evidence of the nominee’s success.
Please use the space below for additional comments, or to provide links or citations for materials or publications that show evidence of the nominee’s success
|