- What are the key factors for physician practices to consider when weighing involvement in value-based payment models?
- Industry-wide, gauge the trend for physician-practice uptake of value-based payment models?
- How do you organize physician practices to embrace value-based payment models? At physician practices, are there particularly daunting hurdles to adoption of value-based payment models?
- At SETMA, how have your clinical models of care changed to match value-based payment models?
- At SETMA, have value-based payment models driven down service volume? If utilization rates have declined, what impact has that had on the practice? If there has been a negative impact, did you find ways to offset that impact?
- At SETMA, what are the prime ways you are using data in conjunction with value-based payment models?
- How does changing from “volume” to “value” payment models affect measurement of patient experience of care?
- What are the essentials of value-based payment reform?
- Do they have the infrastructure to measure value?
- Have they begun a cultural change to focus on value measurement?
- Have they achieved or are they working toward achieving PC-MH recognition or accreditation and preferably are they committed to gaining both NCQA Tier III recognition and accreditation by one or more of the following: AAAHC, URAC, The Joint Commission and/or Planetree.
- Do they recognize and accept the inevitability of value-based payment models as the future of healthcare. At the TEPR Conference, May 11, 2000, in San Francisco, California, addressed the reality, responsibilities and rights of healthcare providers. The following link is to the entire address: Managed Care and Electronic Patient Records.
In that address, I said:
“In the past five years, Southeast Texas Medical Associates has committed its future to two beliefs:
- “Managed Care strategies can provided excellent care to my patients while helping control the cost of that care.
- “Electronic Medical Records is the only methodology and/or technology, which can make this happen at the provider level. “
To the point of reality, responsibility and rights, I said:
“Managed Care and the Computerized Patient Record: Realities, Rights & Responsibilities
“Managed Care is the free-market's response to the realities of the healthcare industry. The first reality is that there is no possibility of healthcare financing and management ever returning to the laizze faire style practiced up until twenty years ago. Someone is going to control and manage healthcare. The only real question is, "Who?" The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the question of "Who is going to pay for the services?"
“Second, because of the expense of technology and of increasing access to healthcare by a larger population, it is possible for healthcare alone to bankrupt the United States government. Unchecked, the cost of healthcare delivery can prevent the balancing of the Federal budget. The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the questions of, "How much is a service worth and how much is society willing to pay for it?"
“Third, this means there are limited resources to continue to provide the excellent healthcare, which the citizens of this country presently receive. Someone has to allocate those resources. Who? The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the question of, "What is society's responsibility to its most vulnerable citizens as far as access to affordable healthcare is concerned?"
“Fourth, the government has assumed, by law, the responsibility of providing healthcare to a certain segment of our population, and the government is not going to surrender that responsibility. The facts of this reality are explained by the AAPCC - the Actual Average Per Capita Cost. This is a calculated figure based on HCFA (Health Care Finance Administration) payments for healthcare in the United States. It is calculated on a county-by-county basis for every county in America.
“In the private sector, the principle is the same. While there is no Trust Fund, private companies have budgets and must meet them. Managed care allows industry to budget its healthcare costs by transferring the "risk" to another company. In order to remain competitive, private industry must control healthcare "risk."
“The second relevant issue is "responsibility."
Each "player" in healthcare delivery today is in an unspoken partnership, which has actual and implied responsibilities.
- “Payers (managed-care companies),
- “Providers (physicians and other deliverers of health services) and the
- “Patients (insured).
“Each "player" has its peculiar responsibilities. The payers, of course, have responsibility for operating within the "realities" of the AAPCC and/or contract, and for making sure that access to healthcare is maintained. Balancing these responsibilities is a function of the core values and integrity of the managed-care company and of HCFA regulations.
“Providers are responsible for providing outstanding care. In managed care, healthcare is more directed toward preventative healthcare than to treating a problem, which has already developed. Physician must be aware of the differences in cost for care. The reality is that care obtained at one place, which is equal to the quality of care obtained at another, can be three times as expensive. To conserve the healthcare resources for the benefit of everyone, the physician's responsibility is now, not only to assure quality, but cost-effectiveness as well.
“The patient has responsibilities in the managed-care system as well. In order to get the expanded benefits and cost decrease of managed-care, the patient is responsible for utilizing physicians who have contracted with the managed-care company and who are committed to complying with utilization management guidelines, pre-certification of procedures and review of care. The patient also has a responsibility to avoid habits, which cause increased health problems when and where possible, and to cooperate in obtaining preventive care, which can decrease the cost of maintaining health before serious and costly problems develop.
“The Third Relevant Issue is Rights:
“Within these "realities" and "responsibilities," what are the patients' and providers' rights? The patient has the "right" to excellent healthcare and to access to needed care. However, the rights of the patient must be balanced with the rights of the managed-care company and with the rights of the healthcare providers who provide care. Likewise, the rights of these latter two groups must be balanced against and with the rights of the patient. The patient has the "right" to choose any PCP (Primary Care Provider) who is in the contracted network of the managed-care company and/or for the IPA (Independent Physician Association). And, the patient has the right to go to any specialist who has agreed to cooperate with the managed-care company.
“But, the patient's right to choose his physician cannot interfere with the right of the managed-care company to manage the "risk," which it has assumed. The patient has the right to request that their favorite physician contract with the managed-care company. But, the physician has the right to refuse. And, the managed-care company has the right to expect the patients and providers to comply with the utilization management guidelines and standards required to manage effectively the "risk" the company has assumed.
“Providers have rights also. Most physicians have resorted to demanding their right to lead health care management. The new realities result in that demand being rejected. If providers wish to exert influence over the delivery of healthcare, they will have to accept their responsibilities and collaborate with payers and patients.
“Managed Care and the Computerized Patient Record
“In the context of these realities, rights and responsibilities - and in the context of physicians and other healthcare providers have a "change of mind," how can CPR help us? The standards to which healthcare providers are going to be held in the future are much higher, more rigorous and more enforceable than ever before. For the previous generation of physicians, the question of a Medicare audit was "If"; for the next generation, the question is "When?"
“New standards of care are being enunciated by:
- “HEDIS, The Health Plan Employer Data and Information Set, which is the National Committee on Quality Assurance's standardized set of about sixty performance measures for managed care plans. It has become the industry standard and is at the core of most health plan report cards being developed all across the United States. It is the standard against which all healthcare providers are going to be judged.
- “The National Committee for Quality Assurance (NCQA) is an independent, not-for-profit organization dedicated to assessing and reporting on the quality of managed care plans, including health maintenance organizations (HMOs). It is governed by a Board of Directors that includes employers, consumer and labor representatives, health plans, quality experts, regulators, and representatives from organized medicine. The NCQA indicates that within two years, they are going to be offering NCQA certification to individual medical groups as well as to health plans. The time will come when NCQA certification will be a critical component for success in the emerging medical marketplace.
- “National Standards of Care are going to apply - not only in lawsuits, as they are now - but in provider evaluation and contracting decisions. More and more, in addition to board certification, clinic performance as measured by these standards is going to be the entree to participating in heath plans, as well as board certification.
“Critical performance indicators, such as HEDIS, national standards of care and NCQA certification are going to be increasingly used as measures of clinical performance.
“Computerized Patient Records can be utilized not only to meet these standards of care, but also to prove that they are being met. In the thirteen months that SETMA has been using EMR, we have had five HEDIS audits, all of which have resulted in a superior rating. We are gradually building national standards of care guidelines into the database of our EMR, NextGen. In all of these areas:
- “NCQA Certification
- “HEDIS audits and/or compliance
- “Medicare audits and/or compliance
- “National Standards of Care
“CPR is the only record keeping and patient management tool, which can solve the complex problems facing healthcare providers in the 21st Century.”
This trend is most clearly indicated by the adoption of the PC-MH Model of care In primary care. While this is an assumption, the degree of quality assessment of performance and the emphasis upon cultural changes suggest the validity of the judgment In addition the PC-MH model anticipates value-based payment. This is the link to an article I wrote on PC-MH penetration in Primary Care: Penetration of PC-MH as of September 30, 2014. This article written in September, 2014 states:
“PC-MH Penetration as a Percent of Primary Care Physicians Working in PC-MHs: 18.33%
With NCQA and The Joint Commission numbers and with the estimation of the numbers of physicians working in AAAHC accredited medical homes, there are 45,107 physicians active in medical homes. Agency for Healthcare Research and Quality (AHRQ, a part of Health and Human Services) states that there are 246,090 primary care physicians in the USA: http://www.ahrq.gov/research/findings/factsheets/primary/pcwork1/index.html (From the AMA Physician Master file 2010).
There are appropriately 661,400 physicians practicing in the USA. With 246,090 in primary care and 45,107 working in PC-MH practices, 18.33% of primary care physicians are participating in Patient-Centered Medical Homes.”
The above was updated in January, 2015 with the following results:
“Penetration of PC-MH as of January, 2015
As of the first of this year, the following numbers are reported by the acceding organizations:
- AAAHC
|
Nationally |
433 organizations Accredited for PC-MH that are also Accredited for Ambulatory care - These are probably practice sites rather than individual practices |
|
Texas |
18 organizations accredited for both |
- Joint Commission
|
Nationally |
136 organizations accredited for PC-MH that are also accredited for ambulatory care |
|
Texas |
13 organizations accredited for both |
- NCQA
|
Nationally |
8,112 practice sites |
|
Texas |
Precise numbers not available |
- URAC
|
Nationally |
1 organization and one in progress |
|
Texas |
1 origination -- SETMA |
Critical Concept
With this review, I would judge that 18-40% of Primary Care Practices are prepared to participate successfully in value-based payment models. For specialty care, I would judge that percent to be much lower and I may be overly optimistic about primary care. What I fear is that the easy of quality metric measures, being chosed not by their validating but by the ease of their measurement, will result in an inadequate measure of value.
The only organization of a practice for value-based care is a Patient-Centered Medical Home. This link is to a discussion of how to organize a practice to embrace value-based payment models. SETMA€™s Model of Care Patient-Centered Medical Home: The Future of Healthcare Innovation and Change. This article states in part:
“Transformation
“SETMA believes that the key to the future of healthcare is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- “The methodology of healthcare must be electronic patient management.
- “The content and standards of healthcare delivery must be evidenced-based medicine.
- “The structure and organization of healthcare delivery must be patient-centered medical home.
- “The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
“At the core of these four principles is SETMA"s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery. In the Centers for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS), healthcare providers are required to report on at least three quality metrics. This is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality. PQRS allows for the reporting of additional metrics and SETMA reports on 28 PQRS measures.
“SETMA employs two definitions in our transformative approach to healthcare:
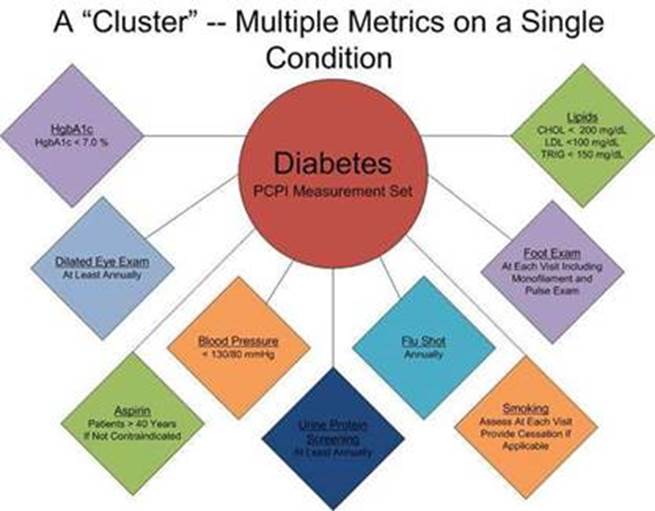
- “A ‘cluster’ is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
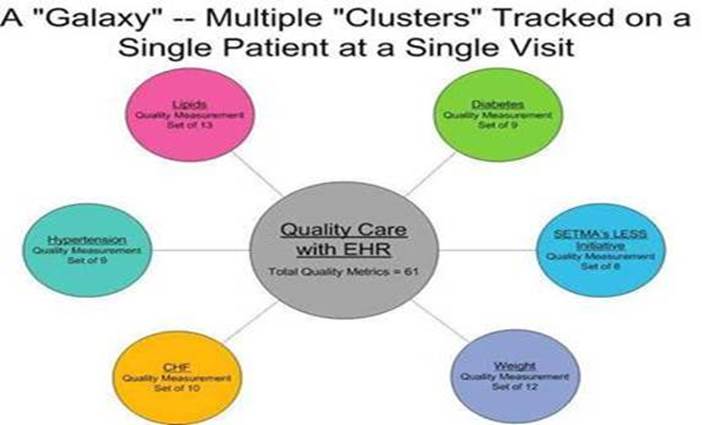
- “A ‘galaxy is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
“SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics, which are measurable at the point-of-care, can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
“The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may multiple “clusters” surrounding multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will decrease as well.
“SETMA"s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
Quality Metrics Philosophy
“SETMA's approach to quality metrics and public reporting is driven by these assumptions:
- “Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care.
- “Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- “The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- “Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient- population data.
- “There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- “The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- “The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- “Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- “Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
“The Limitations of Quality Metrics
“The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
“Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
“Technology Can Deal with Disease but Cannot Produce Health
“In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
“Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
“It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.”
As you will see below, we designed our model of care, which among over 300 published models of care is unique, to produce quality outcomes. Value-based payment models will have no impact on our practice, except that we can easily modify our model to meet any standard which is established. For example, some of the quality metrics and quality measures we track are designed by the Accountable Care Organization design and by the Medicare Advantage STARS program quality metrics. Again, incidental to excellent care and as an expression of our healthcare delivery culture we meet those standards without significant changes to our model.
In May, 1999, we designed and described our model and culture with ten principles. These principles were greatly influenced by Dr. Peter Senge’s (MIT) work in The Fifth Discipline. Ten years later we discovered that those principles are very similar to the medical home philosophy and culture. They are:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
In 2001, we added the following description to our model of care:
“Seeing Circles of Causality
"Reality is made up of circles, but we see straight lines...Western languages...are biased toward a linear view. If we want to see system-wide interrelationships, we need a language of interrelationships, a language of circles." (The Fifth Disciple)
“It is here that we see the application of The Fifth Discipline to medical information technology most clearly. The following concepts derive from Senge's systems principles:
- “Healthcare delivery is not improved simply by the providing of more information to the healthcare provider at the point of care.
- “Healthcare delivery is improved when the organization of that information is such that there is a dynamic interaction between the provider, the patient, the consultant and all other members of the healthcare equation, as well as the simultaneous integration of that data across disease processes and across provider perspectives, i.e., specialties.
- “Healthcare delivery is not necessarily improved when an algorithm for every disease process is produced and made available on a handheld, pocket-computer device but it is improved when the data and decision-making tools are structured and displayed in a fashion which dynamically change as the patient's situation and need change.
- “Healthcare delivery also improves when data and information processed in one clinical setting is simultaneously available in all settings. This improvement does not only result from efficiency but from the impact the elements contained in that data set exert upon multiple aspects of a patient's health. In this way, the data reflects the dynamic within the system under analysis, which in the case of healthcare is a living organism which is constantly changing.
- “Healthcare is improved when there is simultaneous evaluation of the quality of care as measured by evidenced based criteria is automatically determined at the point of and at the time of care. Healthcare is improved when the data display makes it simple for the provider to comply with the standards of care, if the evaluation demonstrates a failure to do so.
- “Healthcare is also improved when data can be displayed longitudinally, demonstrating to the patient over time how their efforts have affected their global well-being. This is circular rather than linear thinking. A person begins at health. Aging and habits result in the relative lack of health. Preventive care and positive steps preserve, or restore health.
- “Healthcare improvement via systems will require dynamic auditing tools which give the provider and the patient immediate feedback on the effectiveness of the care being provided and received.
We have worked with Medicare Advantage (the name has changed through the years) for 19 years. Though Medicare Advantage, where we are paid by capitation reimbursement, we can earn quality and performance payments based on risk stratification and outcomes.
Our experience has been that this has enhanced our reimbursement allowing us to spend $190,000 a month in uncompensated, unreimbursed services for our patients and for us to maintain a Foundation which supports services to those who are uninsured, underinsured or indigent.
Rather than driving down service volumes, SETMA has designed a model which encourages appropriate and quality utilization principally by eliminating economic barriers to care such as co-pays. This allows us to improve quality of care and outcomes while achieving a debt-free status while spending over $9 million on healthcare IT to support the continuity of care and with other funds being used to support care coordination and other measures of quality.
We also receive payments for quality and value through Bridges to Excellence. Being accredited and/or recognized as a Patient-Centered Medical Home by NCQA Tier III, AAAHC, URAC and The Joint Commission, we anticipate the new value-based payment models to take that into consideration in future payments. Again, we achieve these benchmarks not in anticipation of payments but to transform our culture, health-care delivery model and quality. Incidental to that, we expect that someday we will be compensated for that. Because of the proper order of our motivations, if we don’t receive such compensation, it will not affect our commitment to excellence in practice and in measurement.
Perhaps the most critical issue in quality improvement and cultural transformation is the principle that quality metrics should be fulfilled incidental to excellent care and not as the intention of care. The meeting of quality standards should never the object of but quality data production and aggregation is a by-product of quality care. SETMA’s model of care which includes:
- Tracking of 300 quality metrics on each patient we see each day.
- Auditing of provider performance on populations and/or panels of patients.
- Analysis of data with statistical methods to discover needs and opportunities for treating everyone well.
- Pubic reporting by provider name on our website of our performance. We are in our seventh year of this.
- Designing quality improvement initiatives based on these first four steps.
- Establish relative risk for patients and determining treatment algorithms.
- Measuring performance improvement and outcomes for patients.
This process does not identify or address payments but quality and safety. Payments are incidental to excellent care.
As our Medical Home grew, SETMA started a patient-centered council from which we could get feedback about how to improve our services. As the idea of this project grew, we realized that more than “feedback” on what we had decided to do, we wanted our patients and community to give us guidance on what we should do and/or what they wanted us to do.
For many years, we have asked patients to complete “patient satisfaction surveys.” Those are helpful and we shall continue to collect that information. In addition, SETMA has two other tools with which to “hear’ from our patients about the care they are receiving. These are completed by external auditing agencies to maintain objectivity; they are:
- Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS, hospital care)
- Consumer Assessment of Healthcare Providers and Systems (CAHPS, ambulatory care)
Yet, even these tools, which ask the patient to “assess” their care, still are very similar to patient satisfaction surveys. In 2013, in one of SETMA’s monthly provider training sessions, we studied the Institute for Healthcare Improvement’s paper entitled, “High-Impact Leadership Improve Care, Improve the Health of Populations and Reduce Cost.” That paper encouraged the adoption of new “mental models,” which functionally are different ideals about healthcare delivery. Fundamentally, the change in mental models which is needed in healthcare is the move from a focus on “volume” to a focus on “value.”
The significance of this difference is that value and quality, when focused on “volume,” are measured with patient satisfaction, while quality when focused on “value” is measured by patient-centeredness with patients as partners in their care. The following table contrasts the elements of the mental models of “volume” and “value.”

In that HCAHPS and CAHPS use the word “consumer,” SETMA initially determine to name the Council, the Consumer Council. The following critique from the holder of the Dr. and Mrs. James L. Holly Distinguished Chair of Patient-Centered Medical Home at the University of Texas Health Science Center in San Antonio resulted in the changing of that name. Dr. Carlos Jaen said: “My only concern is with the term ‘consumer.’ Knowing what I know about SETMA, I know that you are more about partnerships and healing relationships than selling goods and services. How about ‘Patient and Community Partners Council’? I try to avoid using medical care as a commodity since it cheapens and devalues what we do in primary care.”
With this very good advice, the name became Community Council. The intent is that the Council is comprised of patients of SETMA, community leaders and SETMA colleagues with the majority voting membership of the Council being patients. All SETMA Partners and Executive Management are ex officio members of the Council and can attend the meetings but will not have voting rights except for two who are specifically designated with that responsibility. Any actions taken by the Community Council will be binding on SETMA with the limitation that anything which violates SETMA’s published principles, the rules of the Texas Medical Board or State or Federal statutes, will be disallowed.
The Council’s purpose is to increase SETMA’s sensitivity to the needs and desires of those who entrust us with their care. The purpose is to facilitate patient use of SETMA’s patient portal and health information exchange as well as for patients to help SETMA learn how to get patients more involved in their own medical decision making and in their adhering to the decisions made by them in collaboration with their healthcare provider. The Council is asked to review patient complaints (with identifying information removed) and to give advice on how to respond. The Council also works to expand SETMA’s Medical Home to a functioning and effective Medical Neighborhood in Southeast Texas.
The majority of the Council’s time is spent with patients and community leaders giving SETMA feedback on how we can meet patient needs and for SETMA to listen to the Council about what services they would like for SETMA so pursue and to offer in the future.
We sincerely want the Community Council’s active participation in SETMA. While their personal health information will never be disclosed, we ask permission to use patient and community leader names in public acknowledgment of the Council and in periodic reports of the Council’s work. If we should want to quote a person personally, we ask their permission before doing so.
Thus far, SETMA’s experience with the Council has been outstanding. It is amazing the insights patients have about their experience and the good ideas they have in improving that experience. In our first meeting, patients complained about the length of time it took for them to get their blood drawn in the laboratory. And, not surprisingly, they knew what the problem was. It turns out that without our knowing it, the laboratory re-entered all lab requests into the computer which added a great deal of time for each venopuncture. The changes we made to comply with patient ideas has improved the process significantly.
The experience with the Council led SETMA to invite patients to travel to the 7th Annual Medical Home Summit where they were a big hit. The loudest applause and the most glowing responses were in relationship to the contribution of SETMA’s Medical Home Council, patient members.
At the suggestion of Ms. Christine Bechtel of Bechtel Health Advisory Group, SETMA will expand its efforts to “understand and respond efficiently to the priorities of patients, families and consumers.” At the 7th Annual Medical Home Summit, Christine collaborated with Mrs. Brenda Kerl of SETMA’s Community Council in the session entitled “PC-MH from the Patient Perspective.” The highest audience assessment scores of the week were garnered by Mrs. Kerl which reinforced our commitment to expand the role of the Council and of the participation of other patients in this effort to improve our practice.
As SETMA understands more about Kaizen, the Japanese concept of continuous quality improvement, we will involve all patients and particularly the Council in that process. In most cases Kaizen is based on making little changes on a regular basis: always improving productivity, safety and effectiveness while reducing waste. Suggestions are not limited to a specific area such as production or marketing. Kaizen is based on making changes anywhere that improvements can be made. Western philosophy may be summarized as, ‘if it ain't broke, don't fix it.’ The Kaizen philosophy is to ‘do it better, make it better, and improve it even if it isn't broken, because if we don't, we can't compete with those who do.”
This is the intent and goal of SETMA’s Patient-Centered Community Council.
- Capitation - 50% of the expected reimbursement under value-based payment reform should be received by a practice as a fixed payment which is distributed monthly. This is a forced economy of care as only one payment is made each month no matter how often the patient is seen.
- Patient-Centered Care - this includes patient activation, patient engagement and shared decision making with a personalized plan of care and treatment plan. The achievement of recognition and are accreditation for Patient-Centered Medical Home, when associated with other evidences of coordinated care should be an independent variable for enhanced, value-based payment. The highest credit for this element of value-based payment should be gained by having both NCQA Tier III PC-MH Recognition and one other of the accrediting agencies certificates (URAC, AAAHC, and The Joint Commission).
- Evidenced-Based Performance Metrics - this includes a standard set of NQF, PCPI or NCQA quality metrics which are fulfilled incidental to excellent care and not as the intention of care.
- Hierarchical Code Categories (HCC) and RxHCC - this designation attempts to balance the complexity of diagnoses in order to reward providers for caring for patients with more complex illnesses which cost more to care for. This system should be used to balance both the capitation payment and other payments made in the value-based payment system.
- Preventive Healthcare - as improved preventive care is one of the foundations of hope for controlling escalating healthcare costs, excellence in evidenced-based preventive care should be used in making value-based payment decisions.
- Screening Healthcare - as early detection mitigates the costliness of chronic disease particularly in cancer treatment; excellence in screening care should be used in making value-based payment decisions.
- Benchmarking - value-based payment must include the contrasting of high-performing practices with other practices in rewarding those who perform excellently as judged by comparison with evidenced-based standards and performance standards.
- Coordination of Care - efficiency of care, coordination of care and consistency of care contribute to the management of the cost of care and thus should be calculated in value-based reimbursement.
- Transitions of Care - the use of effective tools of transitions of care enhancing the continuity of care with improved patient safety and care quality should be measured and rewarded.
- Patient Communication - provider/patient communication through secure texting, patient portal or other electronic means should be a part of value-based payment reform.
- Patient Experience Reporting - as one of the elements of the Institute of Healthcare Improvement’s Triple Aim and as a proved element of efficiency and economy of care, the measurement of patient experience should be a part of the calculus of value-based payment reform.
- Global Cost of Care - as providers drive down the cost of care while maintaining the quality of that care, they should be rewarded.
- The Power of Electronics - innovative and creative uses of the power of electronics to improve healthcare with electronic patient management, including the use of clinical decision support, disease management tools and electronic measurements of risk should be rewarded.
- Risk Stratification - the calculation and the sharing with patients of their cardiovascular, cerebrovascular and other disease risk scores with plans of care for mitigating those risks should be a part of the payment reform.
- Behavior and Mental Health - the integration of behavior health into the medical home should contribute to payment reform. The use of depression, stress, and wellness questionnaires should be included in this element of payment reform.
- Weight, Exercise and Smoking Counseling - basic to all health improvement the ability to and the practice of evaluation and intervention in these areas should be a part of value-based payment reform.
James (Larry) Holly, M.D.
C.E.O. SETMA
www.jameslhollymd.com
Adjunct Professor
Family & Community Medicine
University of Texas Health Science Center
San Antonio School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
|