|
Value-based Payments are expected to focus more on outcomes - improvement in health - than process - doing “things” to or for patients. For instance value-based payments will focus more on whether patients with diabetes’ treatments are resulting in improved care rather than just whether patients with diabetes are receiving certain tests.
To promote this change, Health and Human Services (HHS) is designing new programs for payment which focus on outcomes even when they measure a process. One of those is the new Chronic Care Management (CCM) program. If patients who are treated through fee-for-service Medicare, as opposed to Medicare Advantage, and if healthcare providers can meet the rigorous standards, they can participate in the CCM program and be paid for it.
The Chronic Care Management payment is offered by CMS for the care of patients who have more than two chronic conditions and who are contacted each month for complex care management. The contact must result in an aggregate of 20 minutes of time spend in counseling with the patient by telephone or in person including time spent preparing a plan of care and treatment plan.
It is expected that this program will reduce the utilization of other services and decrease the cost of care for patients on Medicare while improving the quality of care they are receiving. The difficulty for providers is that the requires for payment are rigorous and the potential for healthcare providers being audit to determine if they are meeting the standards of care required is significant.
To participate in this program and to make sure that we comply with all standards, SETMA is designing a clinic decision support tool for documentation and auditing of the requirements. The following is the beginning of a tutorial for SETMA’s preparation for this task which includes documentation for:
- Performed - to prove that the monthly contact with patients has been completed
- Documented -- to prove that the patients included in the program meet all standards
- Compared - each patient is compared to prove that exclusions are met, such as nursing home admission, home healthcare and transitions of care charges being submitted during same period.
- Audited -- to prove to ourselves that all elements of the Chronic Care Management are being done and to be prepared to prove that all elements have consistently been met if we are audited.
- Patient agreement for being involved in the CCM program.
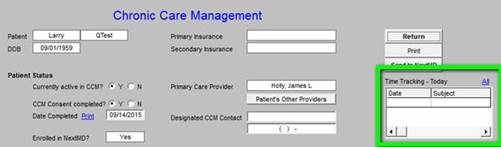
The Chronic Care Management documentation will be launched from SETMA’s AAA Home Template as seen below outlined in green:
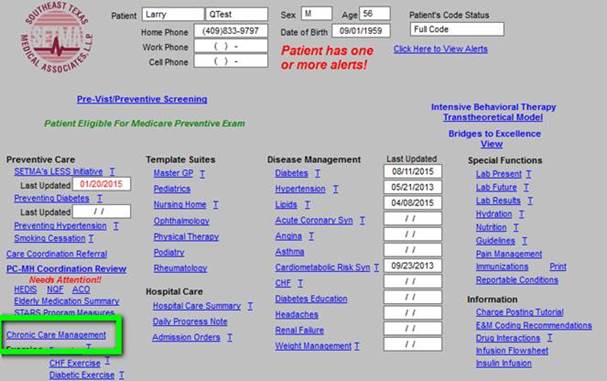
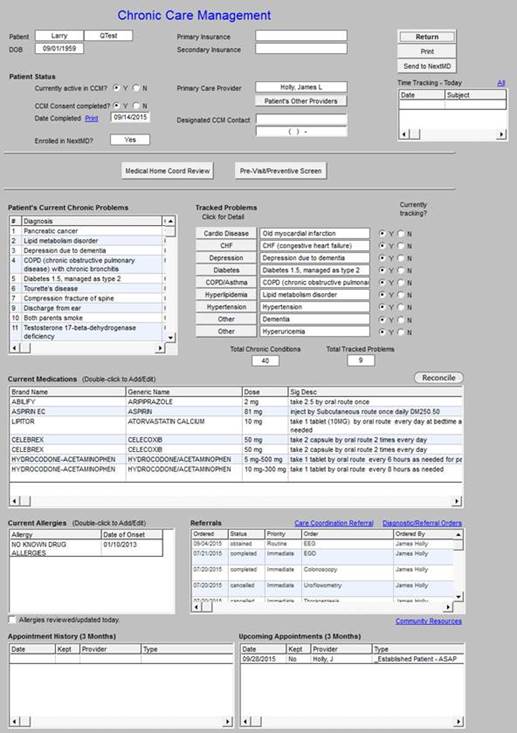
The CCM is found at the link surround in green above. The Chronic Care Management Master template is shown below. It includes:
- Primary and Secondary Insurance Designation -- The primary insurance will be Medicare Fee-for-Service. Because the patient will be responsible for the 20% which Medicare does not pay and because many of the patients who need this service cannot afford to pay their part which is $8.60, it is important for us to know that they are insurance for this to be paid. Medicare doses not allow providers simply to “forgive” the 20% required payment. In order to excuse patients from paying that amount, Medicare requires that three, registered letters be sent to the patient, requesting payment. For the Chronic Care Management services, the patient’s 20% is less than the cost of the collection-effort requirement.
- Patient Status in regard to CCM participation
- Primary Care Provider and Designated CCM contact
- Time Tracing function to document time spent monthly on CCM
- Patient’s Current Chronic Problems
- Tracked Problems and whether or not they are currently being tracked.
- Current Medications and whether or not they have been reconciled
- Current Allergies
- Referrals
- Appointment History and Upcoming Appointments.
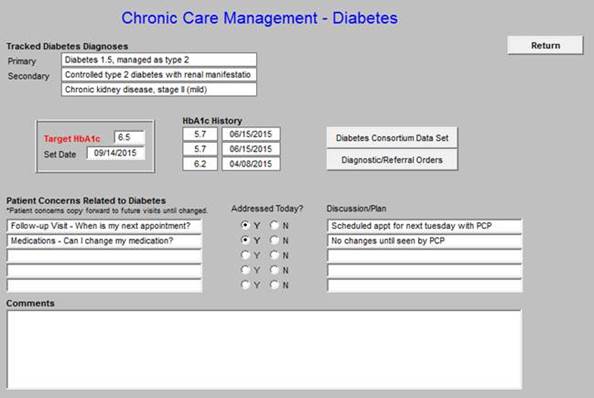
The CCM requires the patient to have at least two chronic conditions and documentation for each condition being tracked is required. The following is taken from the above template and shows what conditions are being tracked. The example used is outlined in green and shows that this patient is being “tracked” for diabetes.
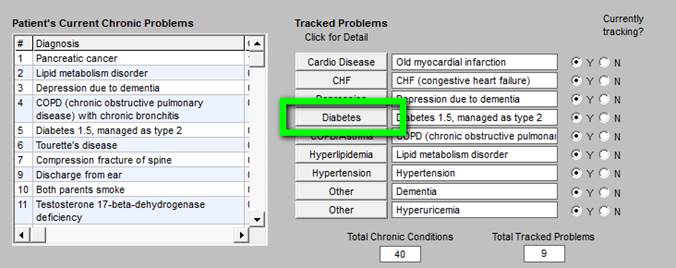
When the Diabetes button outlined in green above is clicked the following pick list will be deployed: This allows the person calling the patient to efficiently document concerns the patient has with their care for the chronic condition involved.
There are seven structured data fields for Chronic Conditions for SETMA’s deployment of the CCM function; they are:
- Cardiac Disease
- CHF
- Depression
- Diabetes
- COPD/Asthma
- Hyperlipdemia
- Hypertension
There are several non-designated fields to be used for other chronic conditions.
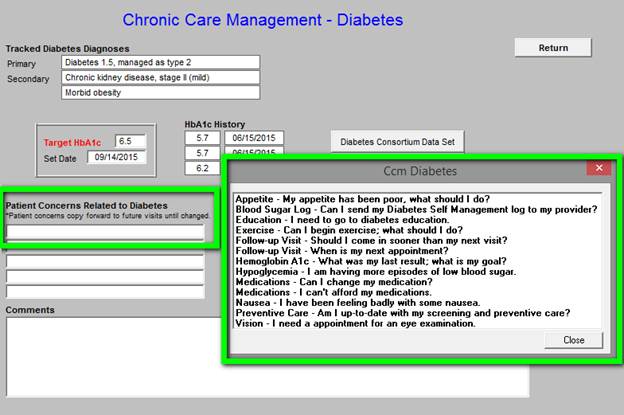
When completed, each Tracked Problem will have a CCM template similar to the one below for diabetes. When the Diabetes tab above is clicked the CCM tool shown below will be deployed. For diabetes, there will be a HbA1c target with a date for that being achieved. The last three HbA1c will be document automatically. The Diabetes Consortium Data Set which includes targeted goals will be listed as is seen below and a referral tool will be deployable from this template as well.
In addition, there is a place to document the patient’s expressed concerns about their diabetes care and a place to denote whether diabetes was discussed in the current CCM contact with the details of the discussion and the treatment plan.
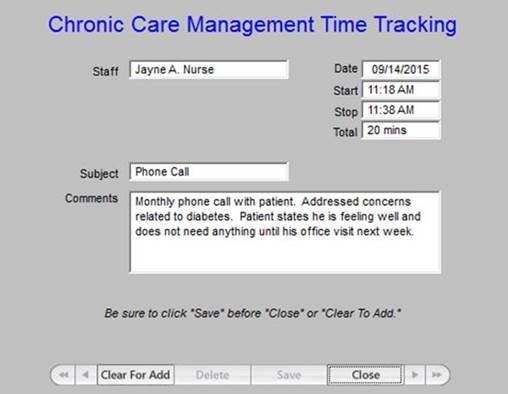
Time Tracking
Each patient enrolled in the CCM program must have a monthly contact. Between the planning and actually telephone contract the provider or nurse must spend at least twenty minutes to meet the requirement for a CCM payment. The following tools allow SETMA providers to document who completed the planning and who made the contract.
It is expected that the CCM program will decrease hospital admission and re-admissions and that it will improve patient health as it increases patient activation, engagement and shared decision making.
|