|
Through its EHR and Business Intelligence data management tools, SETMA has eliminated any uncertainty about whether it is meeting national quality standards-and its providers no longer need to wait months to receive quality reports from payers. IBM’s B I software, COGNOS, allows every provider to examine performance at the point-of" service on over 200 quality metrics, including age-appropriate screening and preventive care needs.
The discrete data capture capabilities of SETMA's EHR are used to measure, on a daily basis, each individual physician's performance of "best practice" standards against every applicable healthcare quality measure available. Before a patient is seen, for example, his or her chart is searched to determine if all HEDIS, NQF, PQRI, PCPI, AQA or NCQA standards have been met. Nurses independently initiate the completion of preventive and screening services according to age requirements.
Software also allowed SETMA to create dashboards that display seasonal outcomes patterns. For instance, trending showed diabetes patients were less healthy from October to January because of lax diet, exercise, and medication interventions during the holiday season. Further analysis revealed lower visit and testing frequency as well. As a result, the practice designed a plan to encourage checkups during the holidays. This issue never could have been noticed, or addressed, by looking at individual patient data.
Dashboards allow the identification of population-wide trends that drive the changes in practice policies that improve care. SETMA has been able to analyze patient populations by: provider panel; practice panel; financial class (payer); ethnic groups; and socio-economic groups. Some of the metrics reviewed include: visit and test frequencies; number of medications taken; changes in treatments and patient education levels.
SETMA feels that tracking only single or a few quality measures will not substantially change outcomes. So it has defined multiple groups of quality measures and reports on their outcomes as well: a "cluster" is seven or more quality metrics for a single condition (e.g., diabetes, hypertension); and a "galaxy" is multiple clusters for the same patient (e.g., diabetes, hypertension, lipids and congestive heart failure). Fulfilling "clusters" and "galaxies" of metrics at the point-of-care will lead to substantial outcomes improvement, SETMA believes.
Incorporating comprehensive disease management tools within EHR workflow also has furthered the ability of providers to deliver timely, quality care. Tools are available to help facilitate best practices in the diagnosis and treatment of diabetes, hypertension, lipid abnormalities, renal disease, cardiometabolic risk and congestive heart failure. Indeed, the ability to perform quality review while still in the room with a patient bolsters the provision of optimal care during every encounter.
Ethnic Disparities of Care
Perhaps one of the most valuable benefits of SETMA’s EHR and BI auditing capabilities is in regard to our care of patients who are part of a minority population. SETMA is a multi-ethnic, multi-cultural, multi-faith practice. This is true among the partners, the providers, the patients, and the management of SETMA. As a result, we are particularly sensitive to disparities in access to care, or in the outcomes of care for any group regardless of a discriminator which may describe or define any person or group of persons. There is no place this is truer than in the case of ethnicity. While nationally there are significant disparities of care between various racial groups, SETMA has worked hard to eliminate those differences.
With an EHR and BI capabilities, we are now able to understand the processes and outcomes of the care we delivery to all of our patients and to compare those processes and outcomes by ethnic groups, gender groups, socio-economic groups and other categories. The following are SETMA's results for treating over 8,000 patients with diabetes. The goal is to successfully treat all patients with diabetes to goal and to eliminate totally ethnic disparities in the care of diabetes. SETMA's results are good and do demonstrate that ethnic disparity of care has been dramatically decreased particularly in the care of diabetes.
Diabetes
For an analysis of ethnic disparities, our data for the treatment of diabetes for the past twelve months is as follows:

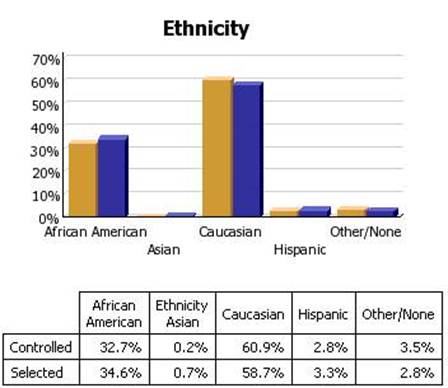
Before the judgment is made that Caucasians receive significantly better healthcare, the bar graph must be described.
- 3783 patients seen by SETMA providers in the past twelve months had diabetes.
- As a percentage of the 3783 patients with diabetes 1,323 were controlled. (For this audit, "controlled" is defined as the patient having had a HgbA1C below 6.5 % for the entire year.) If, as in the case of the National Quality Forum (NQF) Comprehensive Diabetes Measurement Set, "controlled" were defined as below 7% and the measure called for an examination only of the most recent HgbA1C, the percentage of those designated as "controlled" would rise to 59.9%.
- 60.9% of the patients who had diabetes and who were seen in the past twelve months and whose HgbA1c was below 6.5% for the entire year, were Caucasians
- 32.7% of African American treated by SETMA who had diabetes, who were seen in the past twelve months and who had HgbA1C had a HgbA1C continuously below 6.5%.
- The second classification on this graph is entitled "selected." In the case of the above bar graph, "selected" refers to all patients whose diabetes, at any point in the year, was above 6.5%. There were 2460 of them.
At first glace, it might be assumed that the care of Caucasians was twice as good as that of African Americans. But note that the percentage of "controlled" and "Selected" is not of a subset but a percentage of the same whole. As a percent of the whole, SETMA treats twice as many Caucasians as African Americans. As a percent of those who exhibited continuous control of their diabetes, it is the same proportion of African American as Caucasian. Their treatment judged by process measures or by outcomes measures is identical. The conclusion is that the ethnic distribution of all of SETMA's patients with controlled diabetes is nearly identical to the ethnic distribution of SETMA's patients with uncontrolled diabetes.
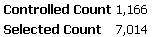
Cholesterol (Dyslipidemia)
In the case of the treatment of cholesterol (dyslipidemia), the case for the elimination of ethnic disparities of care is not as clear. In the current audit the definition of "controlled" for lipids is a Low Density Lipoprotein (LDL) below 70 mg/dl.
As can be seen by the bar graph below, there is a statistically significant disparity in the care of African Americans with dyslipidemia. Because we have eliminated the financial barriers of access to care for our patients, we recognize that the remaining disparity has to do with life-style, cultural and socio-logical problems. All for which we are working to design solutions. These data represent a total of 8,170 discreet patients with the diagnosis of dyslipidemia.
Approximately 23% of those number are African American and slightly over 70% are Caucasians.
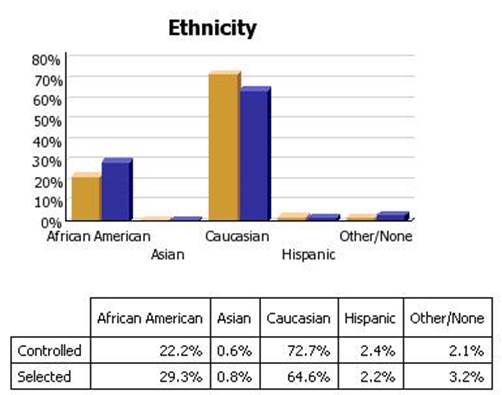
Hypertension
The same explanation applies to hypertension. The goal is to have blood pressure below 130/90 which is defined as "controlled." Again, this audit is displays as "controlled" only those patients whose blood pressure is below 130/90 for the entire year. If we changed the auditing criteria to the last blood pressure being below 130/90, the "controlled" group would rise to over 70%. A total of 8,180 patients where seen in the past 12 months with the diagnosis of hypertension.
Approximately 9,632 discreet patients with hypertension were treated at SETMA in the past twelve months. 6,476 of them had blood pressure readings consistently below 130/90. 3,156 had at least one reading above 130/90.

This disparity is less than that of dyslipidemia but it still exists.
Through patient-centered medical home SETMA continues to design education programs, dietary management programs and other interventions in an attempt to overcome the remaining disparities in the outcomes of our care of African Americans with these serious health problems.
|