|
HEDIS@ is the most commonly used quality metric set. The only successful way to use quality metrics consistently is to have data aggregated automatically and to allow providers to see their performance at the time they are seeing each patients. This has been the key to SETMA’s success in improving care with the help of metrics.
SETMA’s Quality Metrics Philosophy
SETMA’s approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there. In a different context, this was described in 1856 by Abraham Lincoln when he said, “If we could first know where we are and whether we are tending, we could better judged what to do and how to do it.”
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
The Limitations of Quality Metrics
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinicians/scientists. But what makes us better healthcare providers is our caring for people.
The following is a description of SETMA’s deployment of the HEDIS@ measures.
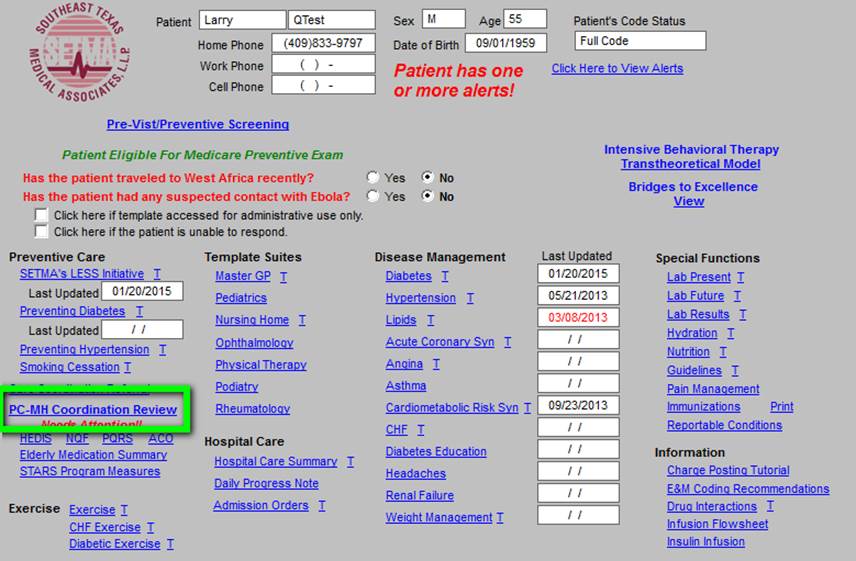
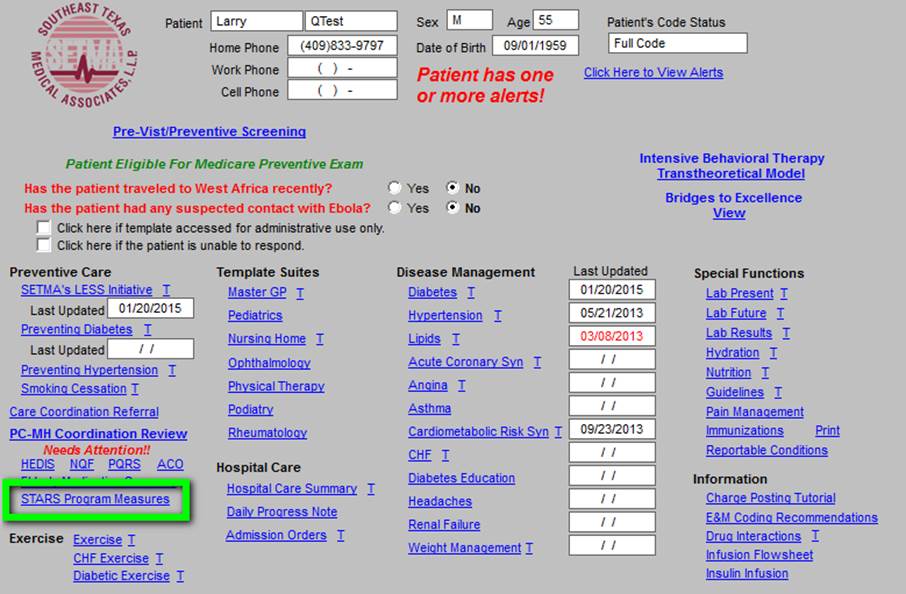
The first screen of SETMA’s Electronic Medical Record is seen below. In the first column is a hyperlink entitled PC-MH Coordination Review (seen outlined in Green below).
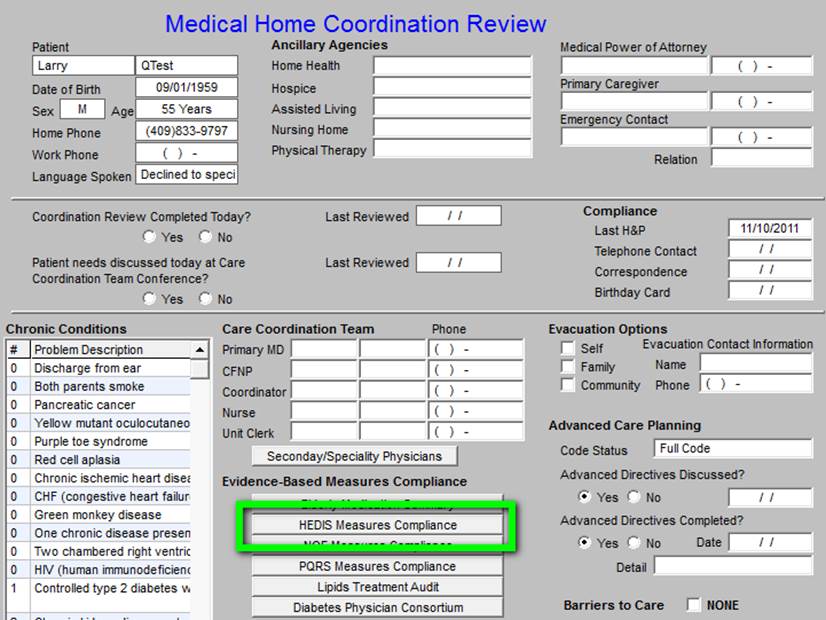
When this link is activated, the Medical Home Coordination Review appears. As indicated above and as seen in the hyperlink outlined in Green below, the full HEDIS@ measure sets is listed here. A picture of that screen was seen in the January 29th Examiner.
If a provider wishes to evaluate his/her own HEDIS@ performance on all measures, it can be done by clicking this button. If the provider wishes to review all HEDIS@ measures which are dependent upon the healthcare provider, he/she can do so by accessing this link.
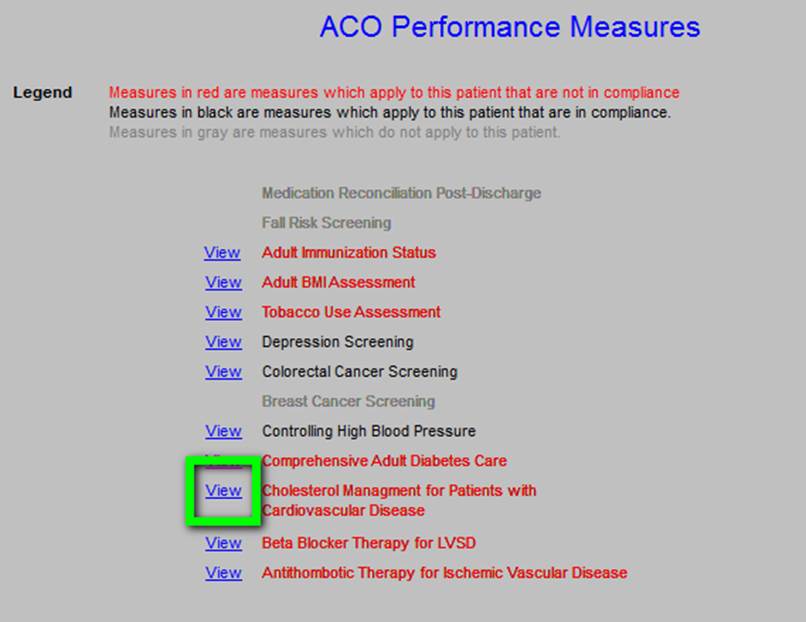
The following is an example of the technical specifications of a HEDIS@ measure. All can be reviewed by accessing each of the measures. To determine whether the provider has fulfilled HEDIS@ measures he/she can simple use the color coding: red means the measure applies to this patient and has not been fulfilled; black means the measure applies to the patient and has been fulfilled; grey means the measure does not apply to this patient. On this screen it is possible for the provider to review the details of each of the individual quality measures as illustrated in the February 5th Examiner.
ACO HEDIS@ Metrics
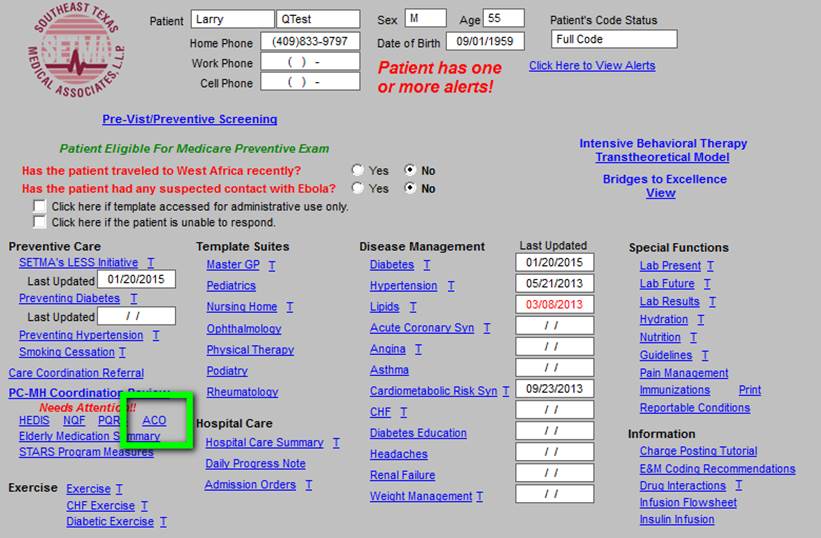
For the provider to review his/her performance on the HEDIS@ quality metrics required in order to benefit from the Accountable Care Organization (ACO) shared-savings plan, the provider can see the link on the AAA Home Template below, outlined in green.
The provider’s performance is shown on the template which pops us. The coding is the same: red applies and not done; black applies and done; grey does not apply.
The Medicare Advantage STARS Program quality metrics are launched below by clicking on the hyperlink outlined in green
The following gives the details of the HEDIS@ measures which apply to the MA STARS program.
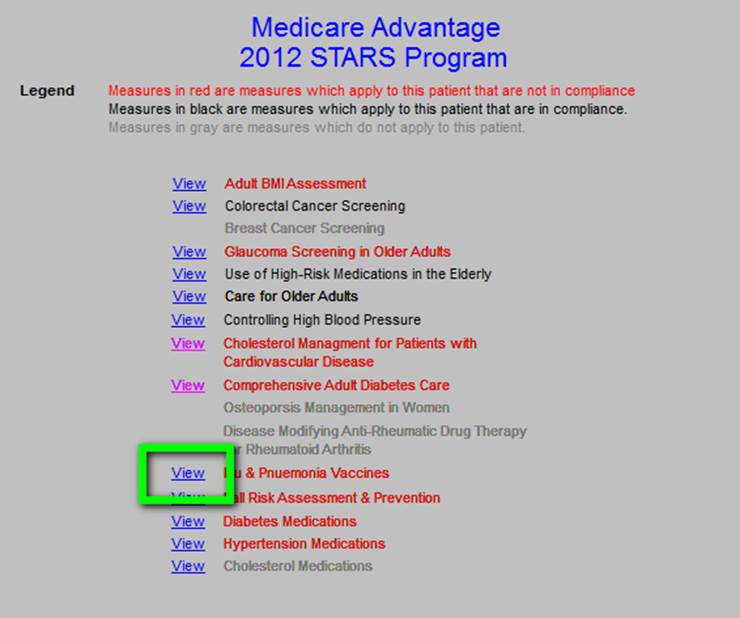
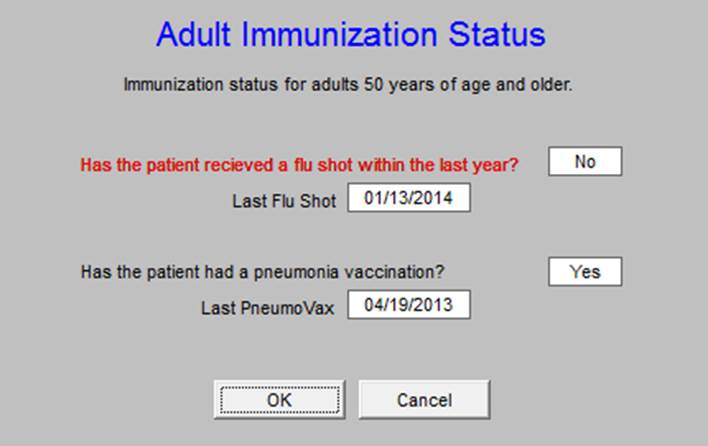
The following are the details of one of the HEDIS@ STARS metrics.
Once a provider knows what metrics are and once he/she has a method for aggregating the data automatically, the provider can use metrics to improve his/her own performance. And, once patients know what metrics are, they can objectively judge the quality of care they are receiving.
|