As part of SETMA’s Patient-Centered Medical Home, we annually complete five questionnaires for each patient to assess the following:
The standard is that each questionnaire should be completed on all patients at least once a year and more frequently if a change in conditions dictates. The Fall Risk should be completed on all patients over 50 and on younger patients who as a result of chronic condition are at risk of falling. Provider performance on these questionnaires is publicly reported below. The content of the questions are as follows.
Falls represent one of the greatest dangers to the health of our elderly and particularly our frail elderly. The life expectancy of a person over 80 who breaks a hip from a fall has a fifty-percent, six months morality rate. At 30 days, the morality rate is 10%. The elements of the fall risk assessment are on the following template which is completed electronically.
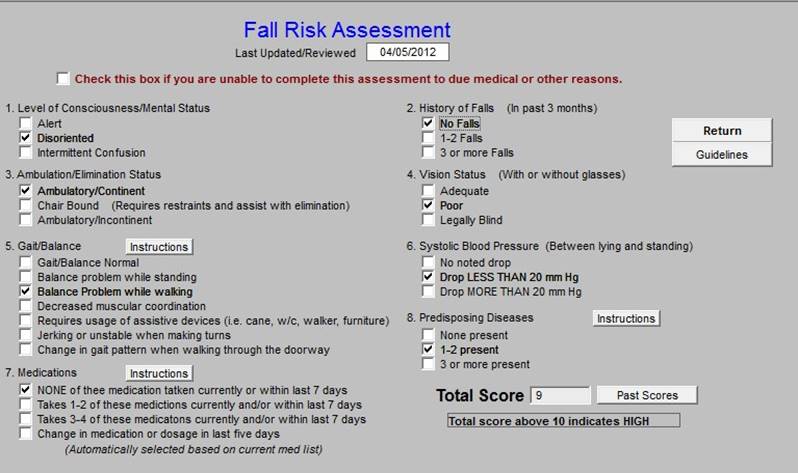
Once the Fall Risk Assessment is completed, the provider should, on the basis of the score, access the “Guidelines for Fall Precaution” and prepare a plan for preventing falls.
The importance of this assessment along with the assessment of the bone density (the bone strength) of elderly patients is important in the prevention of fractures. Remember, the six months survival of patients over eighty years of age after a hip fracture is only 50%. Most cancers have a longer survival rate. The cause of this high mortality is not directly the fracture but the stress related to the fracture, its treatment and to other conditions.
The next questionnaire is a Global Assessment of Functioning. This tool is adapted from the Global Assessment of Functioning (GAF) Scale -- American Psychiatric Association. (2000), Diagnostic and statistical manual of mental disorders (4th edition.
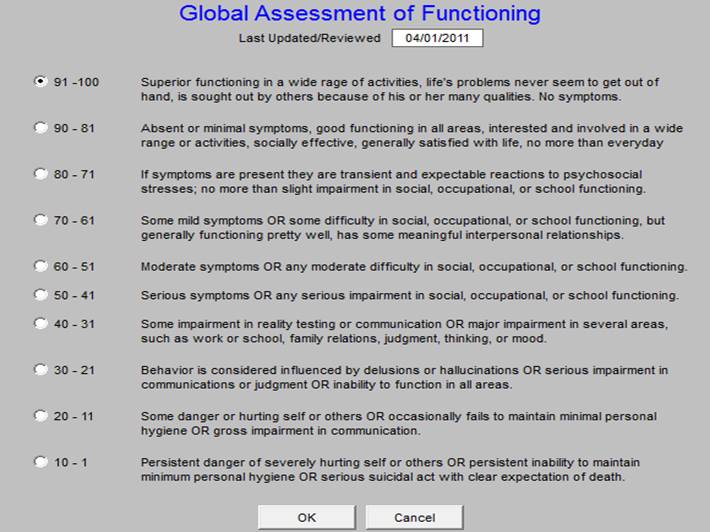
This assessment is important in both the design of a plan of care and treatment plan and in the judgment of how engaged the patient can be in their own care. Also, it helps evaluate and document safety issues in regard to whether a patient can live alone and care for him/herself independently. This is particularly important in transitions of care from one setting to other, i.e., from the inpatient status to the ambulatory setting. If a patient has a low functioning status and lives alone, the are going to require a change of living circumstances to be safely cared for.
SETMA uses this questionnaire in conjunction with three others which are primarily involved in Hospice care but which have great value in functional assessment. They are: the Karnofsky Performance Scale for adults; the Lansky Performance Scale for Children under sixteen; the Functional Assessment Testing Alzheimer’s And Other Related Conditions. These can be reviewed at www.jameslhollymd.com under Electronic Patient management Tools/Specialized Tools/ Stratifying End-of-Life Risk for Hospice Services.
The third questionnaire is the Patient Pain Screening tool. This tool was developed by the National Institute of Health 2007, Pain Intensity Scale. This is a simple but valuable tool which allows you to assess the patient’s perception of their level of discomfort. This assessment must
be balanced with the physical examination. If the patient states that their pain is 8-10 and they are sitting quietly with normal pulse, no sweating, elevated heart rate, elevated blood pressure, clammy, cold skin or other physical evidence of pain, the possibility of an exaggeration of pain exists.
The fourth scare is the Stress Assessment. This assessment was published in the University of California, Berkley Wellness Letter, and August 1995. The Scale Developers were: Lyle Miller and Alma Dell Smith of Boston University Medical Center.
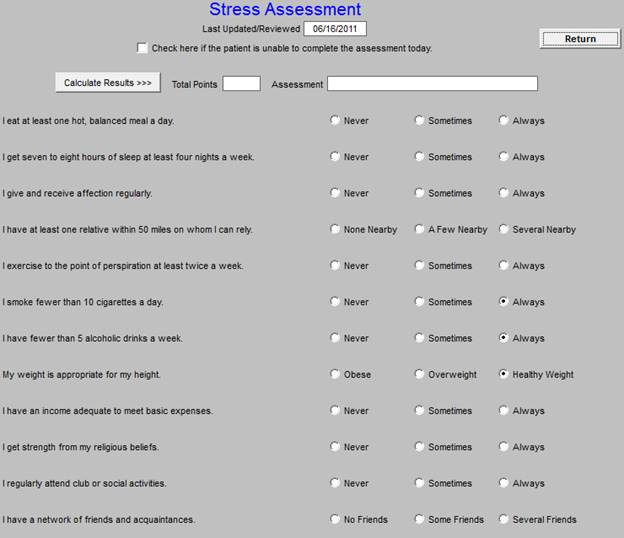
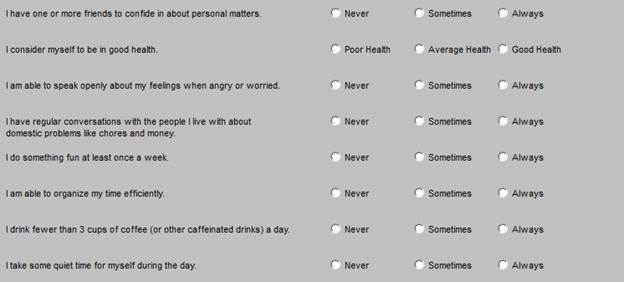
The Stress Assessment based on the Score
>=80 points You have an excellent resistance to stress.
>=60 points You may be somewhat vulnerable to stress.
<60 points You may be seriously vulnerable to stress.
The importance of this score is both its results and its content. The elements of the assessment alert a healthcare provider and a patient to the things which cause stress and points to means of stress reduction. Stress is destructive to the human body. Stress increases blood pressure and pulse both of which contribute to heart disease. Stress increases certain chemicals in the body all of which in excess amounts are harmful to health. It is often possible to improve the control of diabetes without more medications by the reduction or elimination of stress. And, it is important that the best stress reduction does not come from a pill but from life-style modification and the elimination of stressors in one’s life.
The fifth questionnaire is a Wellness Assessment. This was produced by the University of Wisconsin, Health Promotion and Human Development Department through the work of Anne Abbott, Jane
P. Jones and John Munson. Like the Stress Assessment, the Wellness Assessment has value from its result and from its content. It is far more important for a physician, nurse practitioner, physician’s assistant or other healthcare provider to promote wellness than to treat disease. Remember, the best way to treat diabetes is still “don’t get it.”
The following is the Wellness Assessment. This assessment focuses on activity, diet, rest, alcohol consumption, coping skills, etc.
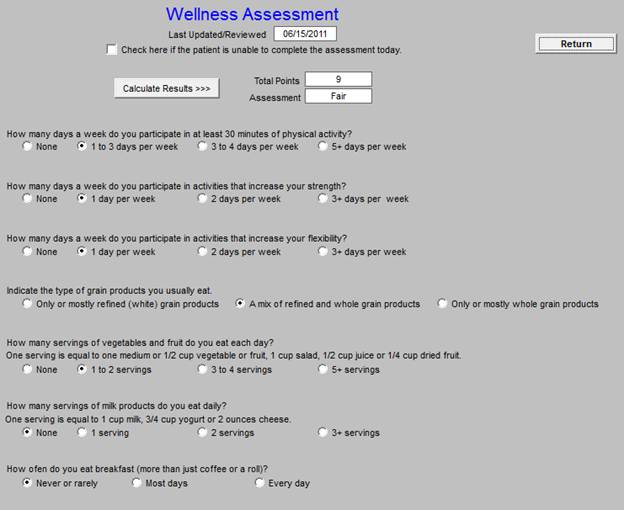
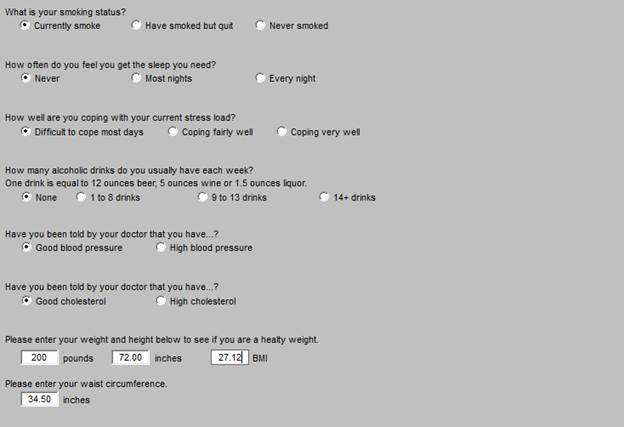
Wellness Assessment results based on the Score
< 5 points Poor
5-9 points Fair
10-19 points Good
20-29 points Very good
>=30 points Excellent
Healthcare is more complex than it once was. Increasingly we have a need for and we have the availability of quantifiable assessments of foundational elements of health and of healthcare.