|
It is often relatively easy to demonstrate that a patient is currently dehydrated or hydrated. However, it is often difficult to declare with objective evidence that while the patient is dehydrated today, he/she was not dehydrated at their last healthcare encounter.
The Hydration Assessment tool is designed to enable you to objectively establish the patient’s state of hydration and to document that in an objective, supportable way. This tool is particularly important to use in the Nursing Home setting as the patient’s state of hydration is an important aspect of long-term residential care and is often the focus of malpractice actions.
The Hydration Assessment Template can be launched from:
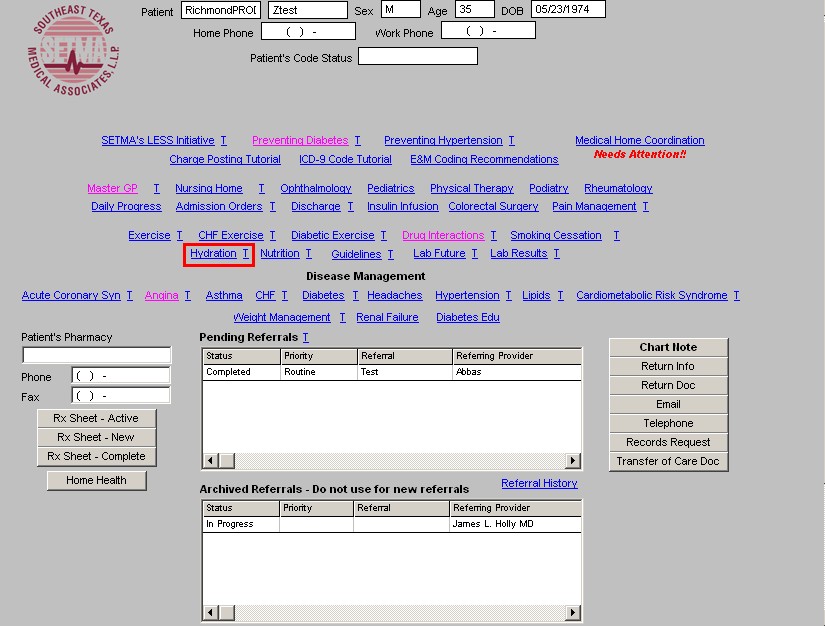
- SETMA Navigation Bar on Patient Data Master
- SETMA Navigation Bar on Nursing Home Templates
- Acute Renal Template in the Renal Failure Suite of Templates
The Hydration Assessment Templates will guide you in objectively documenting the following:
- Increased Risk of Dehydration
- Physical Evidence of Dehydration
- Metabolic and Chemical Analysis of Hydration
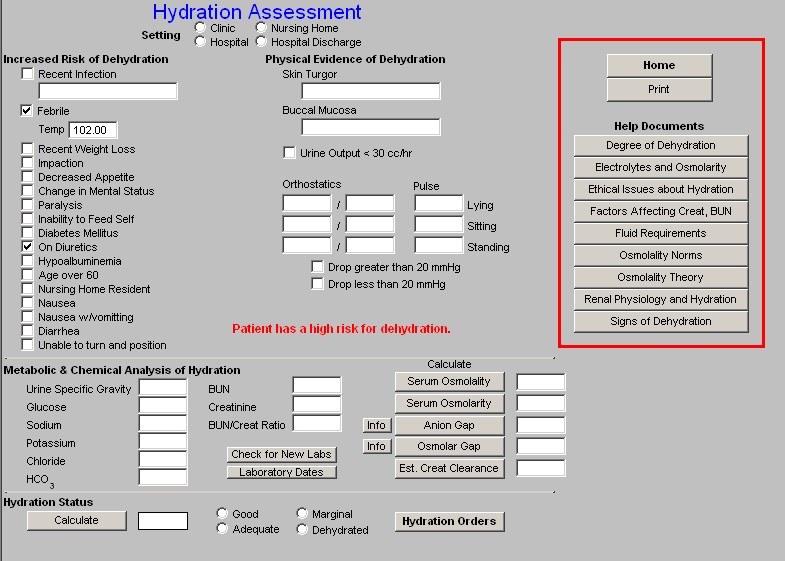
The contents of the Hydration Assessment Tool
The Hydration template is organized into a top section, a middle section and a bottom section. At the top of the Hydration template, there is a function whereby you can document where the tool was used: clinic, nursing home, hospital, hospital discharge.
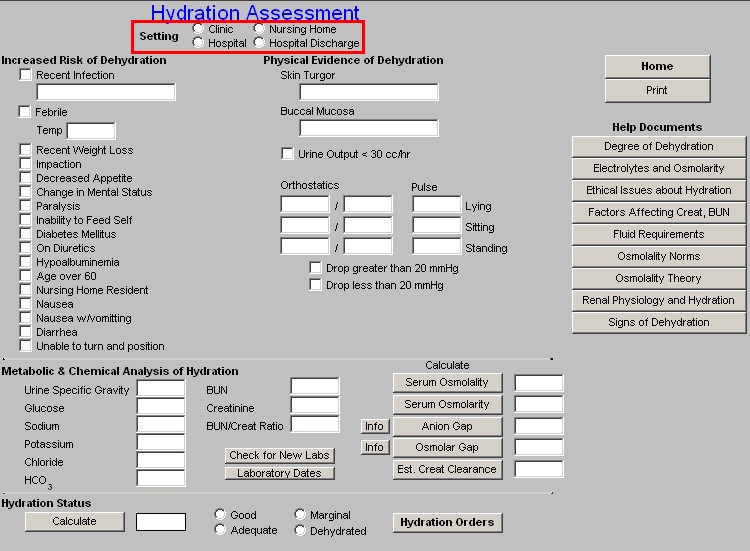
The top section of the template is organized into three columns:
Column 1:
Increased Risk of Dehydration
This provides opportunity for demonstrating that the patient has conditions which place him/her at higher risk of dehydration. These are:
- Recent Infection
- Febrile
- Recent Weight Loss
- Impaction
- Decreased Appetite
- Change in Mental Status
- Paralysis
- Inability to Feed Self
- Diabetes Mellitus
- Hypoalbuminemia
- Age over 60
- Nursing Home Resident
- Nausea
- Nausea with vomiting
- Diarrhea
- Unable to turn and position
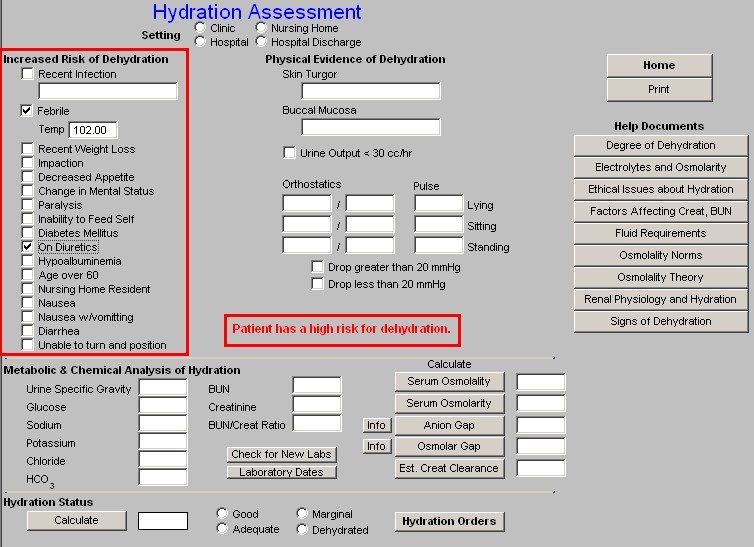
Some of these risk factors will be auto checked, as some of the elements of hydration risk are captured elsewhere in the medical record. For instance, the patient’s temperature is captured automatically, as is whether the patient has Diabetes Mellitus or not, as is the patient’s age, as is whether the patient is a Nursing Home Resident.
Note: It should always be remembered that just because a person has risk factors for dehydration does not mean that they are dehydrated; it only means that they have an increased risk of becoming dehydrated.
Depending on the number of factors, and the particular risks factors which are present for dehydration, the patient will be designated as:
- Patient has a high risk for dehydration
- Patient has a severe risk for dehydration
The only risk factors which will by itself place a patient at “high risk for dehydration” is a temperature of 103 or above. If a patient has a temperature of 102 or less, an additional risk factor such as being on a diuretic is required before the patient is at a higher risk of becoming dehydrated. Typically, it will require four risk factors or more to make a patient at “severe risk for dehydration.”
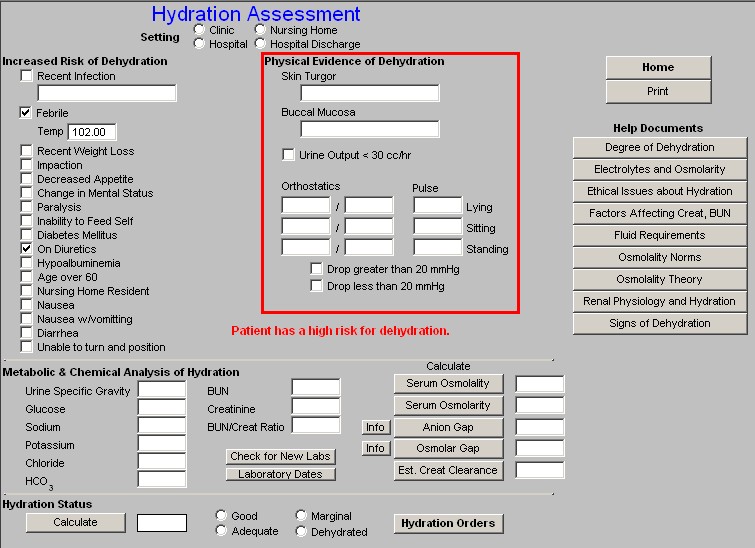
Column 2:
Physical Evidence of Dehydration
Skin Turgor - there is a box to document the patient’s skin turgor with a pick list of “fair,” “good,” and “tenting.”
Buccal Mucosa - there is a box to document the patient’s moisture content of the bucal mucosa with a pick list of: “moist,” and “dry.”
Urine Output - there is a box to check if the patient’s urine volume is less than 30cc an hour.
Orthostatics - there are boxes to document the blood pressure and pulse for lying, sitting and standing. Beneath these boxes are two check boxes: one to document a drop of greater than 20 mm Hg and another to document a drop of less than 20 mm Hg.
Column 3:
There are two buttons:
Home - a navigation button which carries you back to the AAA Home
Print - a button which generates a document for the Hydration Assessment which can be placed on the patient’s hospital or nursing home record. The information on the Hydration Assessment Template automatically prints on the PDM chart note, on the Nursing Home chart note and on the discharge summary note.
Help Documents entitled:
- Degree of Dehydration
- Electrolytes and Osmolarity
- Ethical issues about Hydration
- Factors affecting Creatinine and BUN
- Fluid Requirements
- Osmolality Norms
- Osmolality Theory
- Renal Physiology and Hydration
- Signs of Dehydration
The middle section of the Hydration Assessment addresses the
Metabolic and Chemical Analysis of Hydration
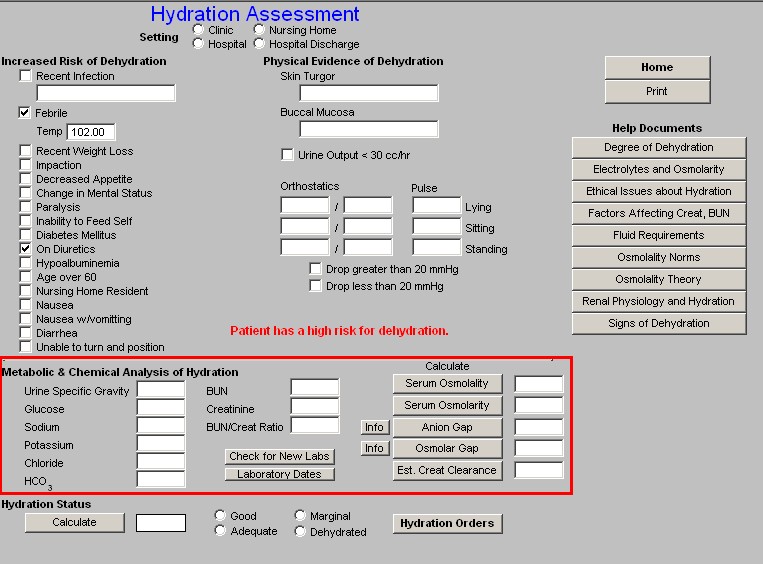
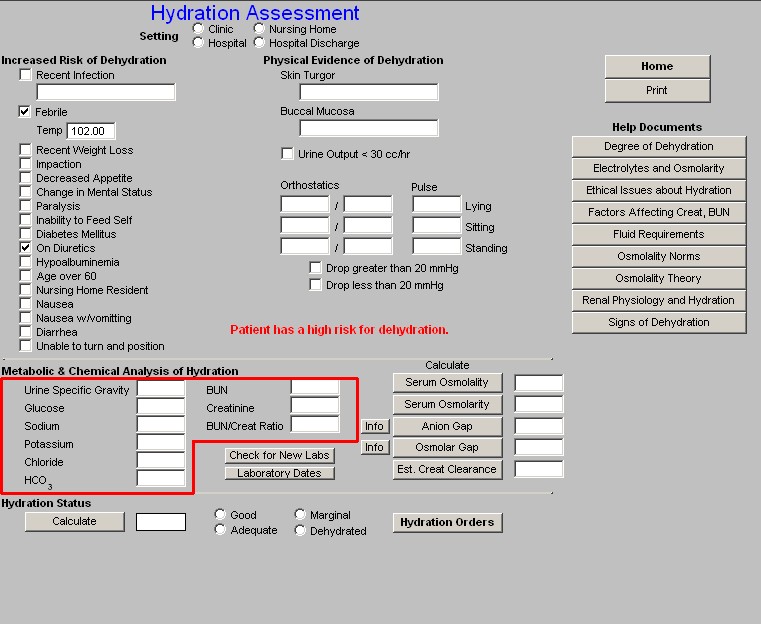
In this section, the following laboratory values are automatically drawn from the laboratory module in NextGen or absent that data, you can manually enter the data from another source. Those lab elements are:
- Urine Specific Gravity
- Glucose
- Sodium
- Potassium
- Chloride
- HCO3
- BUN
- Creatinine
- BUN/Creatinine Ratio
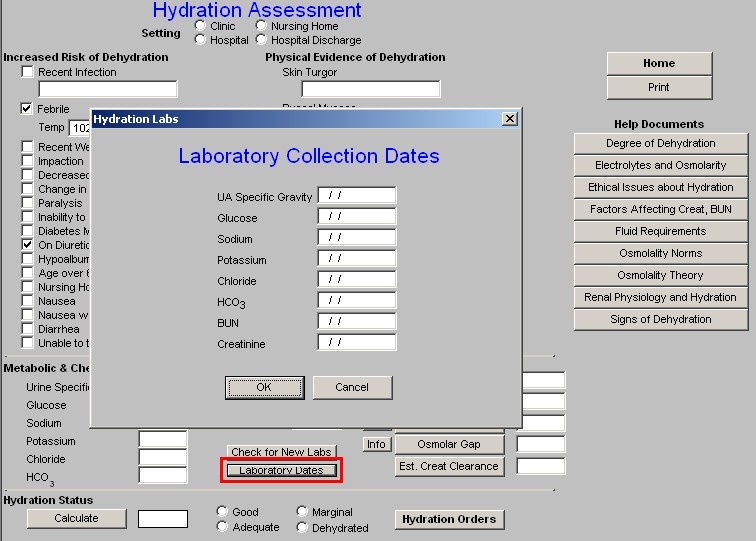
Beneath the BUN/Creatinine Ratio are two buttons:
- Check for New Labs – this checks the NextGen Lab Module for newer laboratory data to make sure that you are evaluating the patient’s hydration with the most recent data.
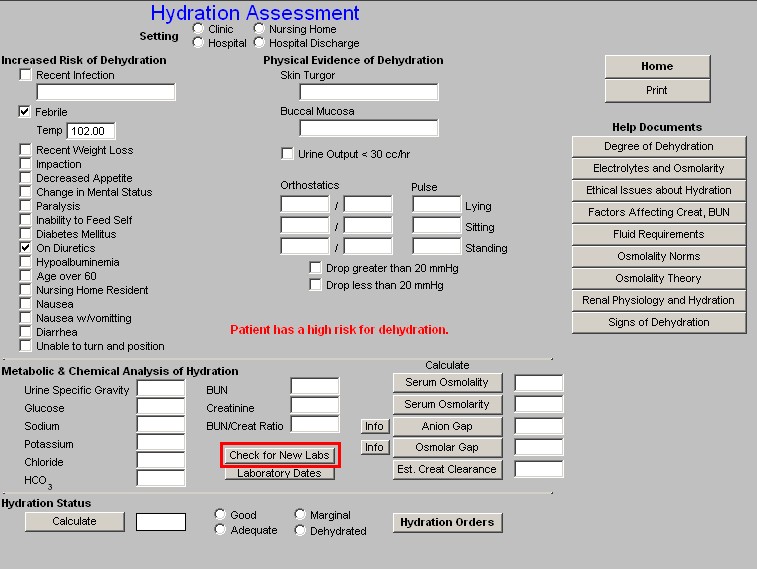
- Laboratory Dates – this launches a pop-up which will give you the dates on which each of the above laboratory tests were performed.
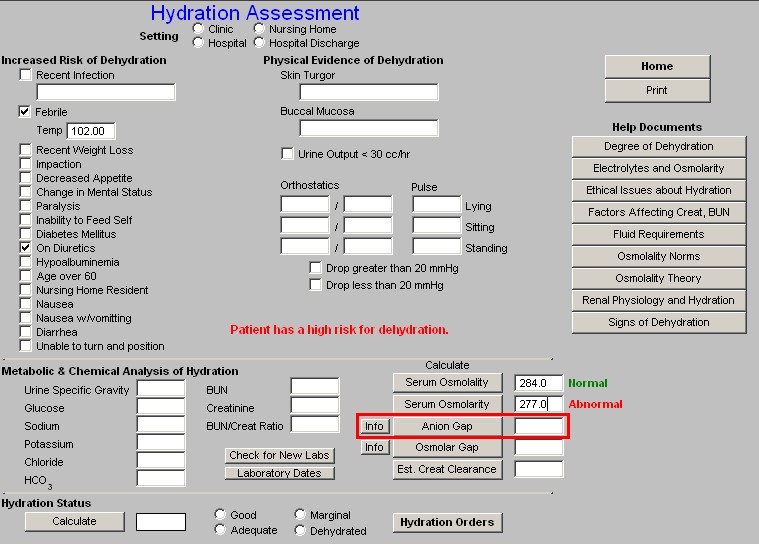
Beside the laboratory values, in the third column of this second section of the Hydration Assessment template are five buttons which automatically calculates and display information about the patient's state of hydration:
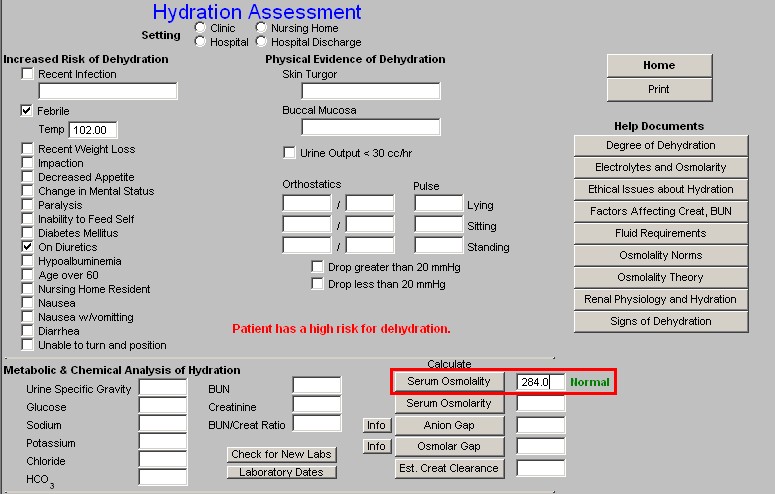
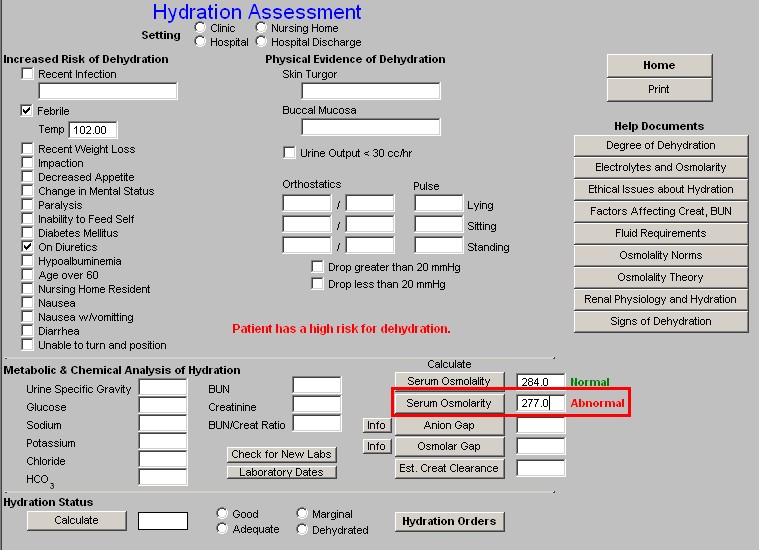
- Anion Gap – there is a help button next to this function which is entitled “Info,” this gives details of the value and interpretation of the Anion Gap.
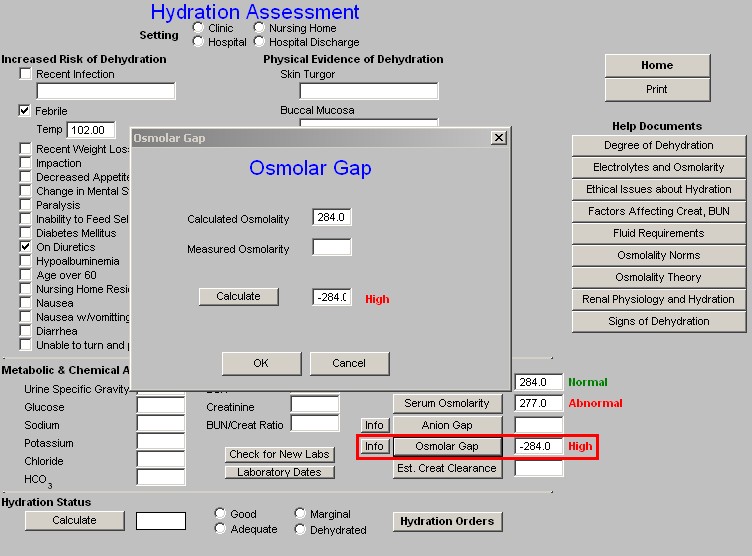
- Osmolar Gap – this button launches a pop-up which calculates the Osmolar Gap. This calculation requires you to add a value to the pop-up for the measured Serum Osmolarity. The “info” button by the Osmolar Gap button gives information about the interpretation and use of the Osmolar Gap.
- Est Creatinine Clearance – this button launches a pop-up calculates the estimate glomerular filtration rate based on the patient’s weight, sex, age and serum creatinine. These data are pulled over automatically. To have this estimate calculate, you must click the “calculate” button on the pop-up.
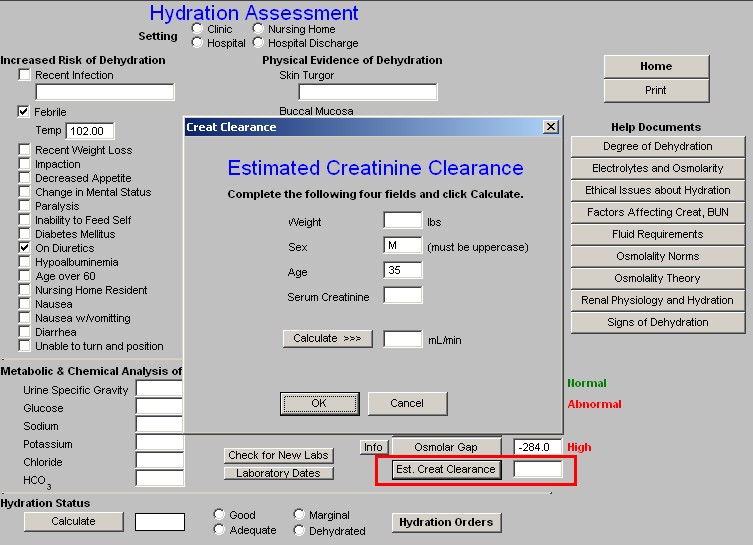
Note: This calculation is the same and the resulting value is the same as the Cockcroft-Gault, which is one of five estimation-of-glomerular-filtration-equations which are displayed on SETMA’s Renal Failure Suite of Templates (See the bottom line of the AAA Home).
The bottom section of the Hydration Assessment Template addresses the patient’s
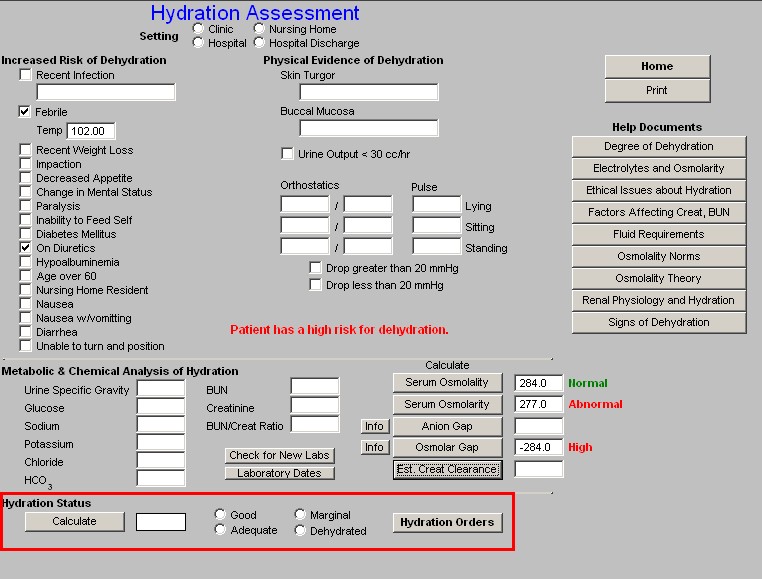
Hydration Status
Using the information in the
- Increased Risk of Dehydration
- Physical Evidence of Dehydration
- Metabolic and Chemical Analysis of Hydration
When you click on the “Calculate” button in this bottom section, the algorithm which is built into this template determines that the patient’s state of hydration is:
- Good
- Adequate
- Marginal
- Dehydrated
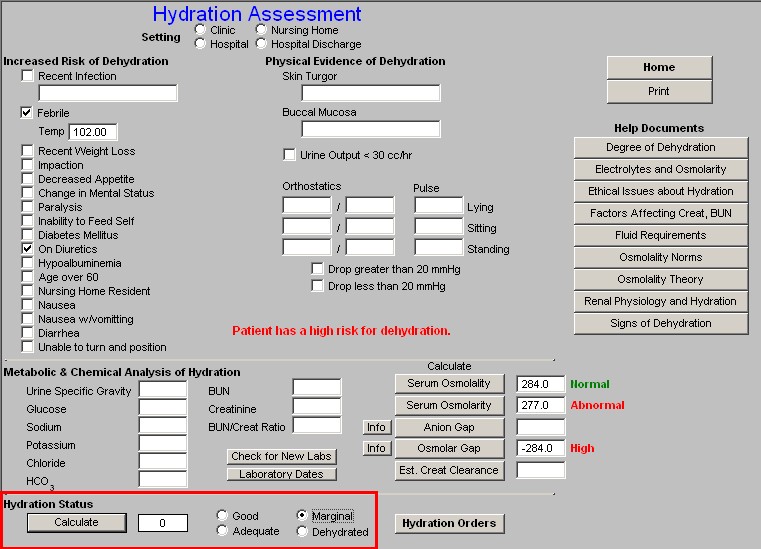
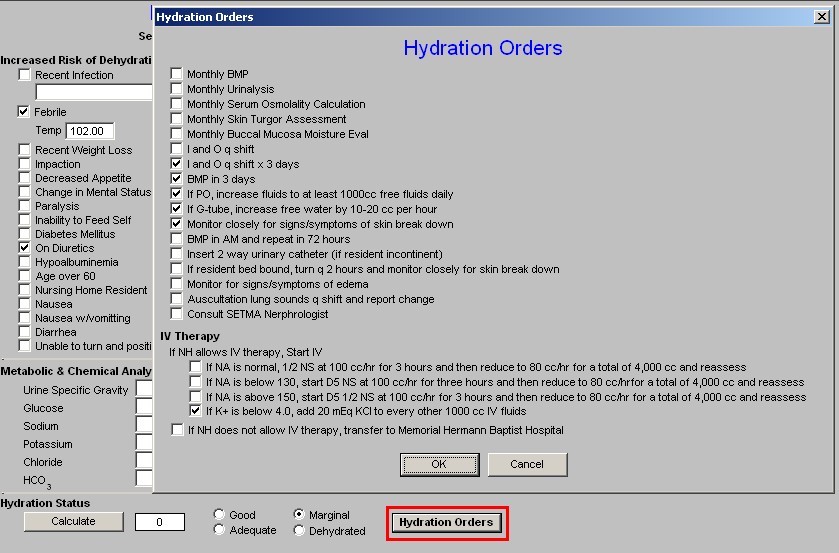
At this point, it is possible to click on the Hydration Orders button which will launch a pop-up which will automatically indicate appropriate actions to prevent dehydration and/or to correct it if it is already present.
These orders will print on the hydration assessment note and then can be placed in the order section of the clinic, hospital or nursing home.
When the hydration template is completed, it provides an objective and comprehensive documentation of the patient’s state of hydration on the date of the present evaluation.
Print
Once the template has been completed, the “Print” button should be launched. This will create an independent Hydration Assessment document which can be placed on the patient’s hospital or nursing home note. The data will also be placed automatically on the clinic, nursing home and discharge notes.
|