|
April 13, 2011
Donald Berwick, MD
Administrator of the Centers for Medicare & Medicaid Services
Health and Human Services
Washington, D.C.
Dear Dr. Berwick:
The Partnership-for-Patients conference call, April 12, 2011, addressed many issues with which Southeast Texas Medical Associates, LLP has been working. Both Transitions of Care and Preventable Readmissions to the Hospital have been part of our group's focus for the past two years, along with the elimination of ethnic disparities of care in diabetes and hypertension.
Each week, I write a 2,000 word newspaper article on healthcare. All articles are posted under Your Life Your Health on our website. There are 29 articles on public policy and health and almost as many on Patient-Centered Medical Home. The following are only a few which address the issues at hand (see Related Articles below).
- Designing a Quality Initiative: How? Hospital Re-admissions, Your Life Your Health, April 22, 2010.
- Eliminating Ethnic Disparities in Diabetes Care, Your Life Your Life Your Health, May 13, 2010.
- Reducing Preventable Readmissions to the Hospital, Your Life Your Health, March 31, 2011.
- Passing the Baton: Effective Transitions in Healthcare Delivery, Your Life Your Health, March 12, 2010.
- Transforming Healthcare Public Reporting of Provider Performance on Quality Measures, Your Life Your Health, December 3, 2009.
- Patient-centered Medical Home SETMA's COGNOS Project Changing Patient and Provider Behavior, Your Life Your Health, October 29, 2009.
Peter Senge
When SETMA started doing "electronic patient management" using electronic health records (EHR) in 1998, we applied Dr. Peter Senge's work in The Fifth Discipline to medicine and particularly to the design of an EHR. The link Peter Senge, The Fifth Discipline and Electronic Patient Records will take you to multiple articles about our application of his work to medicine. This innovation in the design and deployment of EHR has led SETMA to be named by the Office of National Coordinator, HIT, HHS, as one of thirty exemplary practices in clinical decision support. Other recognitions of our work are displayed at Awards and Recognitions.
Care Transitions
In SETMA's Model of Care (for a full description of this see my presentation to the Office of National Coordinator, Care Transitions involves:
- Fulfillment of PCPI Transitions of Care Quality Metric Set which has fourteen data points and four action items.
- Post Hospital Follow-up Call which is a 12-30 minute call which takes place the day after the patient leaves the hospital which is made by members of SETMA's Care Coordination Department.
- Plan of Care and Treatment Plan, which is symbolized by the "baton."
- Follow-up visit with primary provider in less than seven days of discharge and usually within three.
Over the past fourteen years, SETMA has developed numerous tools which enable us to sustain an effort to impact preventable readmission rates. In June, 2009, the Physician Consortium for Performance Improvement (PCPI) published a quality metric set on Transitions of Care. Because SETMA had been completing hospital history and physicals and discharge summaries in the EHR, we were prepared to deploy this measurement set. We have been successfully doing so since that time with 6,147patients discharged from the hospital.
Changing the Name of the "Discharge Summary"
Last September, at a National Quality Forum workshop of Care Transitions in Washington, it occurred to us that the name "discharge summary" was outdated and not helpful. The document had become almost an administrative function often completed weeks after the patient left the hospital. It was not the critical element in the patient's moving from their inpatient or emergency department state to the ambulatory or other setting.
We immediately changed the name of that document to "Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan." This is a long and perhaps awkward name, but it is extremely functional, focusing on the unique elements of Care Transition. From June, 2009 to April, 2011, SETMA has a 99.1% rate of completing this document at the time the patient leaves the hospital. During this time we have discharged 6,147 patients from the hospital.
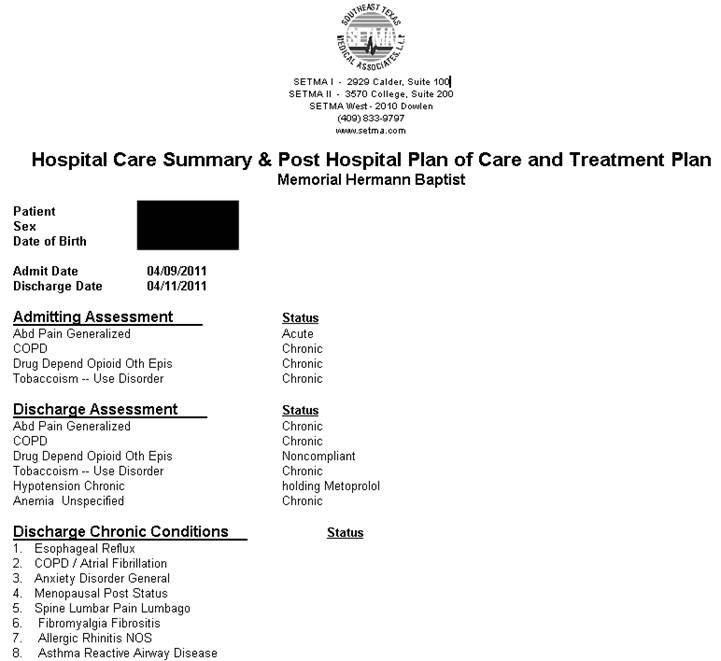
Hospital Care Summary
This is a suite of templates with which the discharge document is created. (For a full description of this see the following on SETMA's website: Electronic Patient Tools; Hospital Care Tools; Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan Tutorial) The following is a screen shot of the Master Discharge Template entitled "Hospital Care Summary". This screen shot is from the record of a real patient whose identify has been removed.
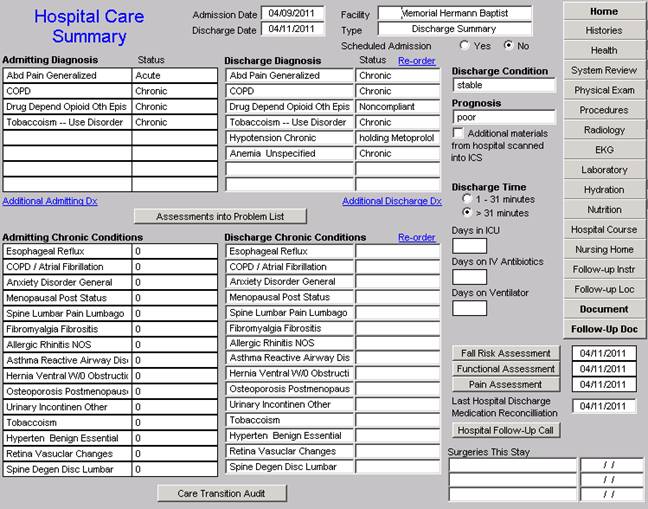
At the bottom of this template you will see a button entitled "Care Transitions Audit." Once the suite of templates associated with the Hospital Care Summary has been completed, the provider depresses this button and the system automatically aggregates the data which has been documented and displays which of the 18-data points have been completed.
The elements in black have been completed; any in red have not.
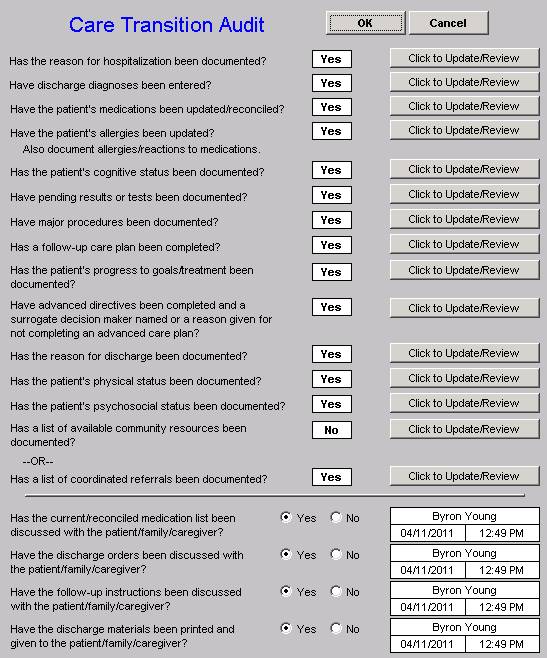
If an element is incomplete, the provider simply clicks the button entitled "Click to update/Review." The missing information can then be added. This fulfills one of SETMA's principles of EHR design which is "We want to make it easier to do it right than not to do it at all."
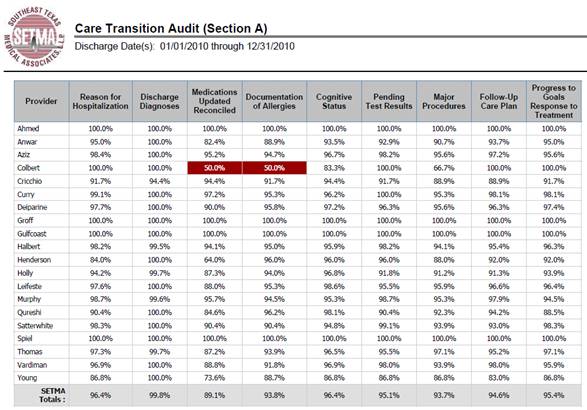
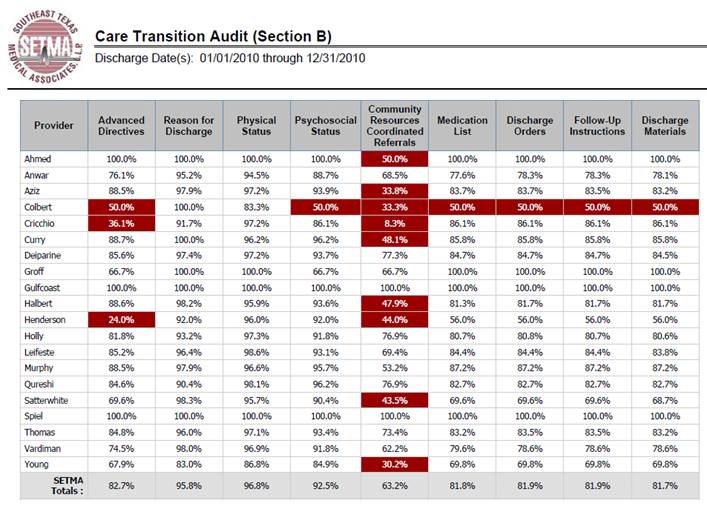
At appropriate intervals, usually quarterly and annually, SETMA audits each provider's performance on these measures and publishes that audit on our website under "Public Reporting," along with over 200 other quality metrics which we track routinely. This reporting is done by provider name. The following is the care transition audit results by provider name for 2010. This presently is posted on our website. The audit is done through SETMA's COGNOS Project which is described in detail on our website under Your Life Your Health by clicking on the icon entitled COGNOS.
Once the Care Transition issues are completed, the Hospital-Care-Summary-and-Post- Hospital-Plan-of-Care-and-Treatment-Plan document is generated and printed. It is given to the patient and to the hospital. The complexity of the Transition of Care is illustrated by this analysis of how many different places this document can be needed. It can go from:
- Inpatient to ambulatory outpatient (family) -- The "baton" in a printed format is given to the patient or in the case of a minor or incompetent adult to a parent or care giver. The "plan of care and treatment plan" -- "the baton" -- is reviewed with the patient, parent and/or family before the patient leaves the hospital.
- Inpatient to ambulatory outpatient (clinic physician) -- for patients who are seen at SETMA, the "the baton" is created in the EHR and is immediately accessible to the follow-up SETMA provider. The provider is alerted by appointment when he/she is to see the patient and that the "baton" is available for review.
- Inpatient to ambulatory outpatient (follow-up call) -- after the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan (HCSPHPCTP) is completed, a template is completed and sent to the Department of Care Coordination. This template is in the EHR where the HCSPHPCTP also resides. Both are immediately accessible to the Department. The "follow-up call from the hospital" call request is delayed for one day so that the call is made the day after the patient leaves the hospital.
- Emergency Department to ambulatory care -- the same process as in "1" above.
- Inpatient to Nursing Home -- the "baton" with a special set of Nursing Home orders is given to the patient or family and a copy is sent to the Nursing Home with the transportation to the Nursing home.
- Inpatient to Hospice -- the same as with number "6"
- Inpatient to Home Health -- the same as number "5" and "6" above. If the patient is seeing SETMA's home health, they have access to SETMA EHR and thus to the "baton."
- Inpatient to outpatient out of area -- "Baton" given to patient and family and also posted to web portal and HIE. Token sent to health provider in remote area which allows one time access to this patient's information.
With this infrastructure and with these care coordination, continuity of care and patient support functions, SETMA is ready to make a major effort to decrease preventable readmissions to the hospital.
The document generated once the care transition issues are met, in part looks like the following. The full document includes reconciled medications, follow-up appointments with time, dates, address and provider name and any referrals which have been initiated as a result of the hospitalization.
The Baton
The following picture is a portrayal of the "plan of care and treatment plan" which is like the "baton" in a relay race.

"The Baton" is the instrument through which responsibility for a patient's health care is transferred to the patient or family. Framed copies of this picture hang in the public areas of all SETMA clinics and a poster of it hangs in every examination room. The poster declares:
Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient,
If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the "baton," is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the "baton" which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient's healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider's knowledge is useless to the patient.
- That the imperative for the plan - the "baton" - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient's health.
- That this transfer requires that the patient "grasps" the "baton," i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for "carrying the baton," longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home are symbolized by the "baton." Its display continually reminds the provider and will inform the patient, that to be successful, the patient's care must be coordinated, and must result in coordinated care. In 2011, as we expand the scope of SETMA's Department of Care Coordination, we know that coordination begins at the points of "transitions of care," and that the work of the healthcare team - patient and provider - is that together they evaluate, define and execute that plan.
Hospital Follow-up Call
After the care transition audit is completed and the document is generated, the provider completes the Hospital-Follow-up-Call document:
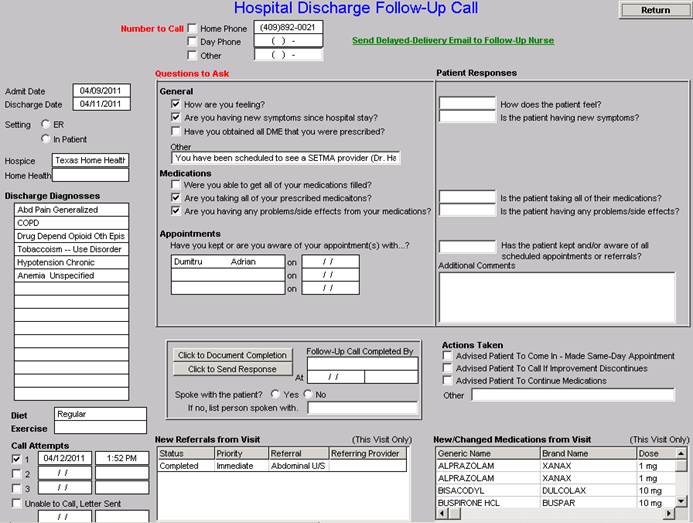
During that preparation, the provider checks off the questions which are to be asked the patient in the follow-up call. The call order is sent to the Care Coordination Department electronically. The day following discharge, the patient is called. This call is a beginning of the "coaching" of the patient to help make them successful in the transition from the inpatient setting to their next level of care. After the call is completed, the answers to the questions are sent back to the primary care provider by the care coordinator. If the patient has any unresolved issues or is having any problem, he/she is given an appointment that same day.
The Care Coordination takes 12-30 minutes with each patient and engages the patient in eliminating barriers to care. If appropriate, an additional call is scheduled at an appropriate interval. If after three attempts, the patient is not reached by phone, the box in the lower left-hand corner by "Unable to Call, Letter sent" is checked. Automatically, a letter is created which is sent to the patient asking them to contact SETMA.
Follow-up Visit with Primary Care Provider
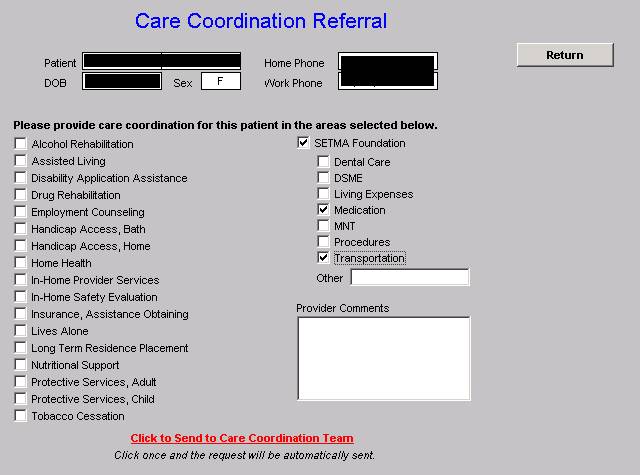
The Transition of Care is complete only when the patent is seen by the primary care provider in follow-up. Many issues are dealt with in this follow-up visit, but one of them is another potential referral to the Care Coordination Department. If the patient has any barriers to care, the provider will complete the following template. In the case of this patient, with the checking of three buttons the need for financial assistance with medications and with transportation is communicated to the Care Coordination Department by clicking the button in red entitled, "Click to Send to Care Coordination Team."
The SETMA Foundation and Patient-Centered Medical Home
Four years ago the partners of SETMA formed The SETMA Foundation. This Foundation provides funding for health care for our patients who cannot afford it. In the past 16 months, the partners of SETMA have contributed $1,000,000 to the Foundation and the results in the lives of our patients have been miraculous. The following is an illustration of the union of Care Transitions, Care Coordination, The Foundation and PC-MH.
Under the Medical Home model the provider has NOT done his/her job when he/she simply prescribes the care which meets national standards. Doing the job of Medical Home requires the prescribing of the best care which is available and accessible to the patient, and when that care is less than the best, the provider makes every attempt to find resources to help that patient obtain the care needed. In February 2009, SETMA saw a patient who has a very complex and fascinating healthcare situation. When seen in the hospital as a new patient, he was angry, bitter and hostile. No amount of cajoling would change the patient's demeanor.
During his office-based, hospital follow-up, it was discovered that the patient was only taking four of nine medications because of expense; could not afford gas to come to the doctor; was going blind but did not have the money to see an eye specialist; could not afford the co-pays for diabetes education and could not work but did not know how to apply for disability.
After his office visit, he left SETMA with our Foundation providing:
- All of his medications. The Foundation has continued to do so for the past two years at a cost of $2,200 a quarter. In September, his Medicare benefits will begin after two years of being disabled.
- A gas card so that he could afford to come to multiple visits for education and other health needs.
- Waiver of cost for diabetes education with SETMA's American Diabetes Association accredited Diabetes Self Education and Medical Nutrition Therapy program.
- Appointment to an experimental vision preservation program at no cost.
- Assistance with applying for disability.
Are gas cards, disability applications, paying for medications a part of a physician's responsibilities? Absolutely not; but, are they a part of Medical Home? Absolutely! This patient, who was depressed and glum in the hospital, such that no one wanted to go into the patient's room, left the office with help. He returned six-weeks later. He had a smile and he had hope. It may be that the biggest result of Medical Home is hope. And, his diabetes was treated to goal for the first time in ten years. He has remained treated to goal for the past two years.
Every healthcare provider doesn't have a foundation and even ours can't meet everyone's needs, but assisting patients in finding the resources is a part of medical home. And, when those resources cannot be found, Medical Home will be "done" by modifying the treatment plan so that what is prescribed can be obtained. The ordering of tests, treatments, prescriptions which we know our patients cannot obtain is not healthcare, even if the plan of care is up to national standards.
Conclusion
Due to the length of this communication, I have excluded discussion of project to address preventable readmissions, diabetes care and ethnic disparities of care.
Hopefully, we will have the opportunity to discuss these areas of our work in the future.
Thank you for "listening." We look forward to the opportunity for contributing to the on-going dialogue about how to transform heath care in the United States.
Sincerely yours,
James L. Holly, MD
CEO, SETMA, LLP
CC: SETMA Partners
SETMA Executive Management
SETMA Providers
SETMA Nurses
|