|
The plaque arrived on April 23, 2013 and read: “Texas Physician Practice Award presented to Southeast Texas Medical Associates, LLP for Providing Exceptional Preventive Health Care Services using Health Information Technology.” Awarded by The Texas Physician Practice Quality Improvement Award Committee, the committed is made up of the TMF Health Quality Institute (Texas’ CMS Quality Improvement Organization), the Texas Medical Association and the Texas Osteopathic Medical Association. Because our Nurse Practitioners are also included in the award, SETMA has recommended expanding the sponsoring organizations to include the Texas Nurses Association.
The Committee commented further, “Congratulations on this significant accomplishment, which illustrates your commitment to delivering quality care to all patients. Your award demonstrates that SETMA has an exceptional team.” “Quality care to all patients” is one of the major goals of healthcare reform and one of the foundational principles of an ACO. This award is also an affirmation of SETMA’s decision in 2000 to begin tracking quality metrics performance and our 2009 decision to begin public reporting of performance by provider name. The results are now posted on SETMA’s website www.jameslhollymd.com under Pubic Reporting for 2009-2013.
Value Equation
The value equation is at the heart of the quality process, i.e., value equals quality divided by cost. Value can be increased by improving quality of care and/or by decreasing the cost of care, or both. In its March, 2013 Brief the Commonwealth Fund tied payment reform to accountability for improved care. They recommended that providers and Accountable Care Organizations (ACO) should be eligible “for additional payment if practices participate in “a high-value ACO,” “bundled payment arrangement,” or other “innovative models of health care delivery.” Also, in March the Commonwealth Fund addressed accountability for quality in a paper entitled, Early Adopters of the Accountable Care Model: A Field Report on Improvements in Health Care Delivery http://www.healthreformgps.org/wp-content/uploads/aco-3-14.pdf.
The Triple Aim and Integrators of Care
Increasingly, health plans and particularly Federal programs are requiring evidence of quality performance with reimbursement tied to that evidence. In 2007, the Institute for Healthcare Improvement (IHI) enunciated The Triple Aim for the future of healthcare which is: improved health, improved care, lower cost. IHI identified “integrators” of health as being organizations which move healthcare by pursing healthcare transformation and innovation. Three of those “integrators” have defined sets of quality measures which must be met in order to receive maximum reimbursement; they are:
- Medicare Advantage - STARS Program - 53 Quality Metrics (This is not to be confused with IHI’s STAARS Program, which is working to decrease hospital readmissions.)
- Patient-Centered Medical Home - National Quality Forum endorsed measures - 10 required by NCQA
- Accountable Care Organizations - 33 define quality metrics
There is significant overlap to these requirements. SETMA reports on numerous quality measures and groups of measures - NCQA, PCPI, AQA, HEDIS, NQF, Guidelines Advantage, Hospital Core Measures, Bridges to Excellence for multiple disease processes, PQRS, Joslin Diabetes, SETMA Developed Measurement Sets, STARS, and ACO measurements.
SETMA’s Quality Metrics Philosophy
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The tracking of quality metrics should be incidental to the care patients are receiving and should not be the object of that care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
SETMA’s Clinical Decision Support
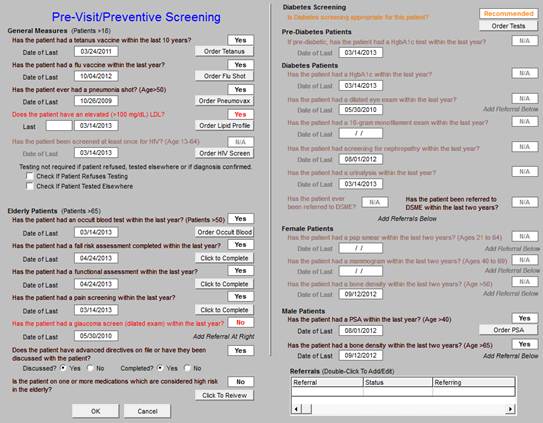
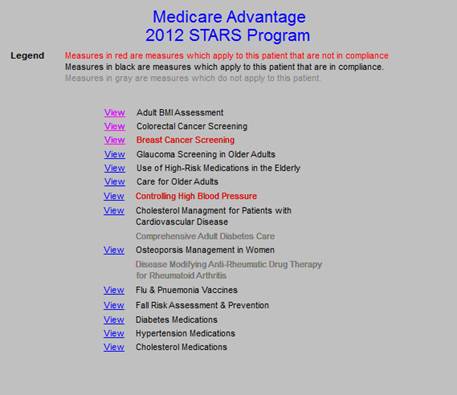
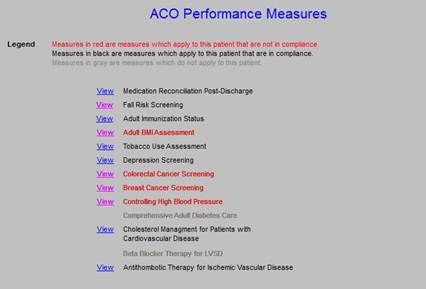
The following are screen shots of our MA STARS and our ACO Quality Metrics tools. The legend is:
- If the measure applies to the patient and has been done, it is in black
- If the measure applies to the patient and has not been done, it is in red.
- If the measure does not apply to the patient, it is in grey.
If a provider wishes to review the content of each metric, he/she can click on “view” and it will show what it takes to fulfill the metric. This makes it possible for the provider, at the point of service, during the office visit, to measure their own performance for what ever “integrator” of care in which the provider is working.
This Clinical Decision Support tool is for general preventive and screening functions.
This is the tool for the Medicare Advantage STARS Program
This is for the ACO Quality Metrics requirements
Why not cheat?
- If you are going to be given a test, and
- if you are given the test questions before hand, and
- if the test is an open-book examination, and
- if there is no time limit for the test,
Why not “cheat?” Look up the answers before the test so that you know what your performance is before you go into the test. Don’t wait until an insurer or an ACO measures your HEDIS performance, or your performance on an ACO measurement set; know your performance before hand by measuring it yourself. In fact, know your performance at the time you see a patient.
Of course, ethically and morally, there is no “cheating” in this context. The test is not measuring what you know, but it is measuring what you have access to and what you pay attention to. The test is not measuring what you remember, but it is measuring what you are reminded of. Consequently, if you have Clinical Decision Support tools (CDS) which remind you of what needs to be done and if you have CDS tools which allow you to measure your own performance at the point of care, it is obvious that you can consistently improve your performance.
Being accountable for good preventive care? That’s easy, which makes the future of ACOs and other “healthcare integrators” bright.
|