|
It is one thing to determine to do something to improve patient safety, to achieve cost savings, or to improve treatment outcomes in healthcare. It is another to do it. Over the past thirteen years, SETMA has identified the following principles about choosing a new quality initiative; they are:
- Begin a new project while completing another
- Build upon your past work
- Leverage your resources in improving care
- Think about what you want to accomplish
- Examine your past work and ask if it has made a difference
- Develop an algorithm to electronically audit to transform data to information
- Use the information to implement change that will make a difference
This description of our current hospital readmission initiative illustrates these principles. Before looking at our initiative to reduce preventable readmissions to the hospital, look at the Institute of Medicine's report (REDESIGNING CONTINUING EDUCATION HEALTH PROFESSIONS, Institute of Medicine of National Academies (IOM) December 2009) which recommends remodeling "continual medication education (CME)" to "continuing professional development (CPD)."
Remarkably, we will discover that CPD is not a great deal different from "continual quality improvement (CQI)" in a medical practice. The IOM's report quotes Goethe on its title page; he said, "Knowing is not enough; we must apply. Willing is not enough; we must do." Here is the difference between CME and CPD. The former is about taking in information; the latter is about transforming performance. The former will not necessarily produce the latter but the latter will begin with questions and answers. This is not unlike the old mantra, we all learned in our medical training, "See one; do one; teach one." It is when you can teach others that you have truly learned if the basis of your teaching is that you have "done."
The IOM report states:
"In recent years, a broader concept, called continuing professional development (CPD), has been emerging that 1ncorporates CE as one modality while adding other important features. CPD is learner-driven, allowing learning to be tailored to individual needs. CPD uses a broader variety of learning methods and builds on a broader set of theories than CE. CPD methods include self-directed learning and organizational and systems factors; and it focuses on both clinical content and other practice-related content, such as communications and business." (p. 17, emphasis added).
The IOM's report went on to say, ""...knowledge of any clinical skill can be broken down into four progressive stages." They are:
- "Declarative knowledge: the learner gains the awareness to identify a problem or to know what should be done;
- "Procedural knowledge: the learner not only understands that there is a problem to solve but also gains knowledge of how to go about solving it;
- "Competence: the learner advances to a stage where he can demonstrate or show how a problem is to be solved; and
- "Performance: the learner identifies the problem, knows how to address it, demonstrates the needed skill, and solves the problem in practice-the learner does what he has learned." (pp. 95-96)
The "doing" which will result from "CPD" is described by the IOM's report as follows: "...an effective CPD system should ensure that health professionals are prepared to:
- "Provide patient-centered care.
- "Work in inter-professional teams.
- "Employ evidence-based practice.
- "Apply quality improvement.
- "Use health informatics." (p. 94)
With SETMA's principles of quality improvement and the IOM's discussion of professional development, let's examine SETMA's 2011 initiative to reduce preventable readmissions to the hospital. Where are we starting?
- SETMA treats almost one thousand patients in long-term residential care. Nationally, hospital admissions from nursing homes have risen to more than 10% of the population of nursing home residents, and readmission rates are over 19%. SETMA has effectively reduced nursing-home hospital admissions to less than 6% of the patients we care for and in one population of patients have reduced readmission rates to 2%. SETMA is currently deploying the recently published National Quality Forum quality measurement set for Long-term Resident Care. We believe that the 21 elements of this measure set will allow us to focus our attention even more on improve the quality of care and consequently the need to transfer patients to the hospital.
- SETMA has reduced the overall readmission rates for Medicare Advantage beneficiaries to 11.6%. from a national figure of over 19%
Both our passed experience and our goals for the future are based on our analysis of the processes of healthcare delivery and of our development of those processes to support effective, safe and excellent care which will result in our reducing preventable readmission rates. What are the steps to that process:
- Ten years ago, SETMA began using our EHR in the hospital to produce history and physical examinations for hospital admissions. This created a continuity-of-care pattern based on the patient's healthcare data.
- Eight years ago, SETMA began using our EHR in the hospital to produce discharge summaries which further advanced the continuity of patient care. Eventually, we renamed the "discharge summary." The deficiency of the name "discharge summary" was that it only incidentally, but not intentionally,, dealt with the complex transitions of care issues created by moving from the inpatient or the emergency department to the ambulatory care arena or other place of other. The name was changed to "Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan." More will be discussed about this later.
- Eight years ago SETMA designed hospital admission order sets based on national standards of care which created a consistency of treatment plans. This act alone decreased SETMA's lengths of stay by almost 22 hours per hospitalization.
- Eight years ago, SETMA began using the EHR in all twenty-two nursing homes we staff. Because our patients' care is managed in the same electronic data base, whether they are in the ambulatory setting, hospice, home health, physical therapy, hospital, emergency department, nursing home or other place, there is a continuity of care which is data and information driven. The
- Two years ago, when the Physician Consortium for Performance Improvement published the first national quality measurement set on Care Transitions, set deployed it in our EHR. In June, 2010, SETMA deployed the PCPI Care Transitions measurement set. The following depicts that deployment in the EHR:
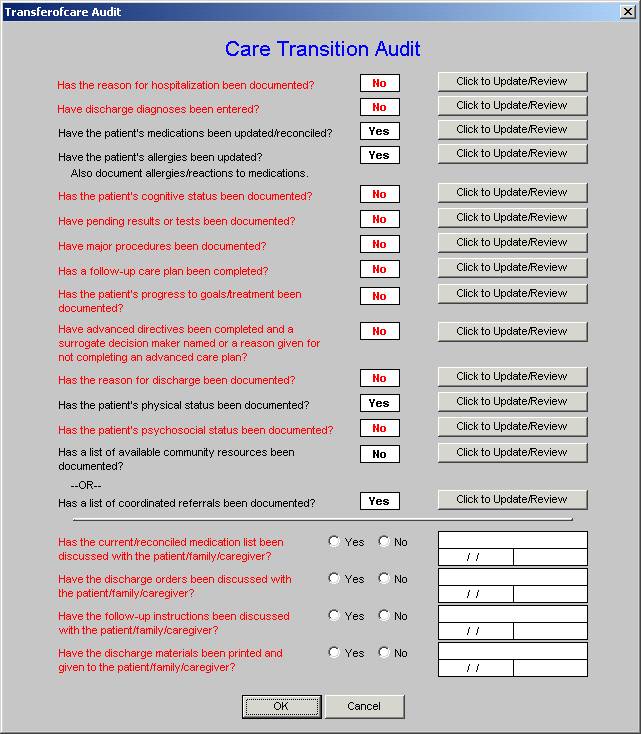
The legend is that all in black apply and are done; all in red apply and are not done.
From July, 2010 to March, 2011, SETMA discharged 2205 patients from the hospital. 99.1% of them had their Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan completed at the time of discharge with a copy being given to the patient, family or parent. The Transition of Care metric set has 14 data points and four actions. The following is our COGNOS audit for the year 2010 on these 18 quality metrics.
- In 2010, pursuit to SETMA become a Tier 3 PC-MH, we created a Department of Care Coordination. As part of that initiative, we began calling every patient discharged from the hospital. The call takes place the day after their discharge and involves a 12-30 minute call which addresses major transitions of care, patient safety, and quality of care issues. If after three attempts no telephone contact is made, a letter is automatically generated and mailed to the patient asking them to contact our office for follow-up.
- About the same time, SETMA designed a Business Intelligence audit of our hospitalized patients to examine differences between patients who are readmitted and those who are not. The BI audit looks at: gender, ethnicity, socio-economic issues, morbidities and co-morbidities, lengths of hospital stays, age, and rapidity of follow-up after discharge from hospital, whether a follow-up call was received and numerous other issues. All of these measures are looking for leverage points for "making a change which will make a difference."
- Four years ago, SETMA's partners realized that many of our patients, even those with insurance cannot afford parts of their health care. Thus The SETMA Foundation was created. The partners have given over $1,000,000 to the Foundation which pays for medications, surgeries and other care such as dental for our patients who cannot afford it. For those whom we have been able to help, virtual miraculous results have been achieved.
- 18 months ago, SETMA undertook to publicly report by provider name the results of our performance on over 200 quality metrics. In addition, the disease management plan of care for hypertension, cholesterol and diabetes includes the provider performance on each individual patient's care as judged by these quality metrics. The former, without patient identification, are reported under Public Reporting.
- 12 years ago, SETMA realized that excellent care in the 21st Century was going to be team-based. As a result, we have a hospital service team which provides 24-hour a day, seven-days a week, in house health coverage for all of our patients. This team supports the healthcare providers and together, this team is achieving remarkable results. In the fall of 2011, we are going to increase the access of our patient to clinic in afterhours care so as to minimize the need for use of the emergency department further.
- Six years ago, SETMA discovered that five different departments in SETMA were keeping paper records of patients admitted to the hospital in an effort to manage the business and professional activities related to these patients. Realizing that this is inefficient and ineffective, SETMA design the IMRC (Inpatient Medical Record Census). This is an electronic function which is deployed on SETMA's intranet. It is HIPPA compliant, secure and password protected by 128 bit encryption. When a patient is admitted to the hospital, the patient's name and place of admission is documented. Then the date of completion of the History and Physical examination is entered. This is done over 99% of the time on the date of admission. Then the date of discharge and date of completion of the Hospital Care Summary and Post Hospital Plan of Care and Treatment plan is documented. If the business office has a question in order to properly bill for services, they post it on the IMRC, the research is done and report to the Central Business Office.
- SETMA has deployed both a secure web portal and a health information exchange to allow the seamless exchange of information between the hospitals and SETMA. Over the next five years, it is our hope to have all healthcare providers in a seven county area connected and sharing secure healthcare information.
- SETMA partners with a Medicare Advantage home health agency and in a Stark-compliant manner with other home health agencies and with free-standing hospices to provide compassionate, competent care for our patients in settings other than the inpatient to reduce readmission from our most vulnerable patients.
- The Hospital Care Summary and Post Hospital Plan of Care and Treatment is transmitted to the next site of care as follows:
- Inpatient to ambulatory outpatient (family) -- The "baton" in a printed format is given to the patient or in the case of a minor or incompetent adult to a parent or care giver. The "plan of care and treatment plan" -- "the baton" -- is reviewed with the patient, parent and/or family before the patient leaves the hospital.
- Inpatient to ambulatory outpatient (clinic physician) -- for patients who are seen at SETMA, the "the baton" is created in the EHR and is immediately accessible to the follow-up SETMA provider. The provider is alerted by appointment when he/she is to see the patient and that the "baton" is available for review.
- Inpatient to ambulatory outpatient (follow-up call) -- after the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan (HCSPHPCTP) is completed, a template is completed and sent to the Department of Care Coordination. This template is in the EHR where the HCSPHPCTP also resides. Both are immediately accessible to the Department. The "follow-up call from the hospital" call request is delayed for one day so that the call is made the day after the patient leaves the hospital.
- Emergency Department to ambulatory care -- the same process as in "1" above.
- Inpatient to Nursing Home -- the "baton" with a special set of Nursing Home orders is given to the patient or family and a copy is sent to the Nursing Home with the transportation to the Nursing home.
- Inpatient to Hospice -- the same as with number "6"
- Inpatient to Home Health -- the same as number "5" and "6" above. If the patient is seeing MediHome, they have access to SETMA EHR and thus to the "baton."
- Inpatient to outpatient out of area -- "Baton" given to patient and family and also posted to web portal and HIE. Token sent to health provider in remote area which allows one time access to this patient's information.
With this infrastructure and with these care coordination, continuity of care and patient support functions, we believe that we are ready to make a major effort to decrease preventable readmissions to the hospital. Each of these 14 steps is building the foundation for our quality initiative.
We believe that the improvements we achieve on this foundation will be sustainable. Two months ago, we discharged 26 patients in two days on the weekend. We have tracked these patients and have experienced 6.8% readmissions. We treated these patients, even though some of them were challenging discharges, through our established procedures and processes so as to have a valid snapshot of the results were are achieving. Sustainability is the key to quality improvement. The foundation we have built will allow us to sustain our efforts even after the initiative is complete. We look forward to monitoring our results over the next three years.
|