|
In addition to the other activities for improving healthcare, SETMA has become a member of the National Quality Forum. As SETMA prepared to apply to the National Committee for Quality Assurance (NCQA) for recognition as a Patient-Centered Medical Home (SETMA was awarded a Tier III recognition in July, 2010), which designation is a registered trademark of NCQA, we were confronted with the requirement that we report to our providers and to at least one external organization our performance on ten quality measures endorsed by the National Quality Forum (NQF). In February, 2009, we had never heard of the NQF.
Thus began our journey into understanding both the science of "quality metrics" and to our participation in the work of NQF. This statement does not imply that SETMA is an expert in the field of quality metrics, or that we currently play a significant role in the NQF, but we do continue to increase our understanding of quality metrics and our participation in NQF. NQF defines itself as, "a unique, multi-stakeholder organization instrumental in advancing efforts to improve quality through performance measurement and public reporting...(and as) a private, not-for-profit membership organization with more than 400 members representing virtually every sector of the healthcare system."
The following is a brief history of NQF. In 1998, A report of the President's Advisory Commission on Consumer Protection and Quality in the Health Care Industry, proposed the formation of the Forum as a part of a national agenda for improvement in healthcare delivery. Formed in 1999, NQF's declared:
"The mission of the National Quality Forum is to improve the quality of American healthcare by setting national priorities and goals for performance improvement, endorsing national consensus standards for measuring and publicly reporting on performance, and promoting the attainment of national goals through education and outreach programs."
NQF's vision is to be, "the convener of key public and private sector leaders to establish national priorities and goals to achieve the Institute of Medicine Aims-health care that is safe, effective, patient-centered, timely, efficient and equitable. NQF-endorsed standards will be the primary standards used to measure and report on the quality and efficiency of healthcare in the United States. The NQF will be recognized as a major driving force for and facilitator of continuous quality improvement of American healthcare quality."
NQF (www.qualityforum.org)"is a voluntary consensus standards setting body as specified by the National Technology and Transfer Advancement Act of 1995 and OMB Circular A-119 (1998). NQF endorsement, which involves rigorous, evidence-based review and a formal Consensus Development Process, has become the "gold standard" for healthcare performance measures. Major healthcare purchasers, including CMS, rely on NQF-endorsement to ensure measures are scientifically sound and meaningful and to help standardize performance measures used across the industry."
As of October, 2008, NQF had endorsed 514 "national voluntary consensus standards." As indicated above, for NCQA recognition as a medical home, a physician group must report to its providers and to an external agency their performance on at least ten measures. In 2009, SETMA began reporting on forty-three NQF-endorsed quality metrics and in 2010, added an additional twenty metrics to our reporting. In 2009, SETMA also began publicly reporting, on our website (www.jameslhollymd.com), by provider name, our performance on these and several hundred others quality metrics.
Care Transitions
In September, 2010, a NQF conference was held in Washington, D.C., entitled National Priorities Partnership Care Coordination Convening Workshop. Two of SETMA's colleagues scheduled to attend this meeting.
In June, 2009 the Physician Consortium for Performance Improvement (PCPI) published an 18-point quality metrics set entitled "Care Transitions." This measurement set addressed fourteen data points which were established as required in order to improve the care of patients being discharged from the inpatient, or the emergency department of the hospital. In addition to the data points, there were four actions which were required. When SETMA read this material in June, 2009, we released that we had been performing all but one of these quality measures for at least seven years. Therefore, we designed a tool through which to document the performance of these 18 quality metrics and through which to audit our performance on completing them. This PCPI Care Transitions measure set is one of the quality metric sets which we began publicly reporting on our website in late 2009.
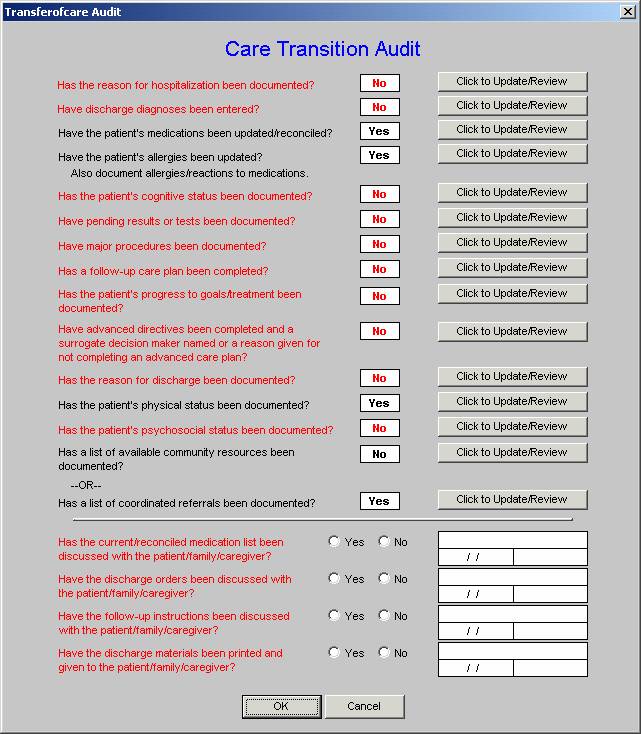
SEMA's Care Transitions template is displayed below. As can be seen by reviewing the 14 data points and the 4 actions required by the audit, when the elements of this audit are met and when the discharge summary and follow-up document are completed with this material, and are given to the patient and/or family, almost all continuity of care issues are resolved. The legend is that everything in black is done and everything in red has not been done.
On August 24, 2010, I wrote the President of the NQF and said, ""SETMA's Chief Medical Officer and I are registering to attend the NQF National Priorities Partnership on Care Transitions in Washington next week. I am a member of the HIMSS PS&CO committee and CEO of Southeast Texas Medical Associates, LLP, a medium size, multi-specialty practice in Beaumont, Texas. We have had experience with 'care transition' for the past 14 months and have designed a quality improvement initiative for decreasing avoidable readmissions to the hospital employing 'care transitions' metrics, as well as other strategies (a preliminary description of this project is attached, entitled 'Designing A Quality Initiative How? Hospital Re-admissions.'"
NQF responded with the following invitation:
"Thank you as well for sending along this useful and encouraging information on care coordination. I see you have registered as part of our audience, which is an open invitation extended to all NQF members. Allow me to offer you a formal initiation to attend the workshop as an invited content expert in this field and to participate in the round table discussions we will be having. Assuming this is agreeable we will send you along additional logistics."
During that conference, it became apparent that one fundamental flaw in healthcare is the name used for the hospital summary of care It is currently called a "discharge summary," and is essentially an administrative document required to complete the patient's record. However, when seen in its "real" purpose, this document would better be entitled, "Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan." SETMA has made that name change and is benefiting from the new and clearer understanding of the rationale for this document.
NQF membership
After our participation in the September, 2010 NQF conference, an invitation was extended for SETMA to consider becoming a member of NQF, which we did. As stated above by NQF policy, and as acknowledged by SETMA, any medical group can join the NQF and any member of the public can attend the open meetings of the NQF. The benefit of membership is that you will receive announcements of current work for which comment is solicited and you will also receive links to completed work, which is published for use in the healthcare industry. For SETMA, the benefit is that we are able to expand our understanding of the content of our transformation of our practice into a medical home, to increase our knowledge of the value and definition of quality metrics, and to broaden our participate in the national discussion about these critical matters in he future of healthcare.
This is illustrated by the notice SETMA received on November 1 with links to the following:
- Preferred Practices and Performance Measures for measuring and Reporting Care Coordination.
- The ABCs of Measurement
- NQF Member and Public Commenting for Driving Quality: A Model to measure Electronic Health IT use.
- Quality Connections and Care Coordination
The Executive Summary of this last publication states:
"Care coordination-a function that helps ensure that the patient's needs and preferences for health services and information sharing across people, functions, and sites are met over time-is foundational to high-quality healthcare. All patients, but especially the growing numÂber of Americans who suffer from multiple chronic conÂditions, can benefit from care coordination. Care coordiÂnation is an information-rich, patient-centric endeavor that seeks to deliver the right care (and only the right care) to the right patient at the right time. UnfortunateÂly, the prevailing model of healthcare for most patients is poorly coordinated, to the detriment of the patient. This poses a threat to patients and the healthcare system in the form of heavy disease burden, safety concerns, and financial inefficiency.
"Essential elements of care coordination include a written plan of care that anticipates routine needs and actively tracks up-to-date progress toward a patient's goals, and a communications 'feedback loop' consisting of open dialogue among members of the care team, the paÂtient, and his or her family. The 'healthcare home,' simiÂlar to but more expansive than the commonly known 'medical home,' is a promising model that may achieve truly coordinated care on a vast scale. The healthcare home is a single, coordinating source of usual care selectÂed by the patient, such as a large or small medical group, a single practitioner, a community health center, or a hosÂpital outpatient clinic. Several demonstration projects currently are testing the viability of the healthcare home model for many Americans.
"The National Quality Forum (NQF) has completed significant work to advance care coordination, including the endorsement of a definition and framework for care coordination; the NQF-convened National Priorities Partnership; the designation of care coordination as one of six 'National Priorities' for national action; and the endorsement of preferred practices and performance measures for care coordination. Ultimately, achieving coordinated care will be possible only when healthcare entities collectively agree to place the patient at the center of care."
SETMA has now read all of these documents, resulting in a clearer understanding of the concept of care coordination, which has already helped us expand the plan of care and treatment plan our patients receive and has benefited others as some of these concepts where discussed in a medical-home leadership conference in which I participated on November 7. SETMA will also incorporate these new understandings into our care transition's audit.
SETMA is looking forward to our relationship with NQF. We think our patients, our practice and our community will benefit.
|