|
Southeast Texas Medical Associates, LLP (SETMA) has been actively working on reducing preventable readmissions for almost three years. We have employed multiple methods in this process.
The SETMA Methods
In a 2008 HIN reducing readmissions survey, thirteen methods (in bold-faced type below) were identified as being employed for the reducing of preventable readmissions to the hospital. The comments in parenthesis address some of the ways in which SEMTA is employing these methods. They were:
- Pre-admission Coaching. This is the continuity of care piece whereby the patient understands the purpose and goal of inpatient care. The patient and family understand that except in accidents, this is typically a failure of effective outpatient care and the goal is to prevent the need for inpatient care in the future. The three-fold method of surviving the hospital is explained: eat u; get up and get out! They know what to expect as to duration of inpatient care and transition to home.
- Use of Hospitalists. SETMA is using hospitalists for particular populations of patients but more than hospitalists the hospital-care-team, made up of physicians, nurse practitioners, nurses, care coordinators and case managers are the structural ways of solving this problems Hospitalists improve the disease-management elements of inpatient care but without a support tem often reproduce the transition-of-care deficiencies of the non-hospitalists program.
- Inpatient Coaching. Keeping the patient and family informed is critical to reducing readmissions. Diagnoses, testing results and prognosis are critical elements to this part of the coaching. Expectations are made realistic, when possible, and the patient and family are prepared for the transition to the post-hospital care setting.)
- Improved Discharge Notes. SETMA has changed the name of the “discharge summary,” to “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.” While long, this name is functional. For 2009-2011, SETMA discharged 25,949 patients from the hospital; 99.1% of the time this transition of care document was presented to the patient at the time of discharge.
- Plan of Care/PHR. In SETMA, the Plan of Care and Treatment Plan is the “baton” whereby responsibility for care is transferred from the provider to the patient.
- Care Transitions & Management. For SETMA, Care Transitions begins on admission, includes the “Hospital Care Summary” document, the Post-Hospital Care Coaching, 12-30 minute telephone contact, and does not end until the patient sees their personal healthcare provider in the clinic, which is always within six days unless the patient is designated as a high potential for readmission where it is within three days.
- Community Partnerships. Key partnerships for decreasing readmissions are hospice, home health, physical therapy, meals-on-wheels and local government agencies who are prepared to supplement the healthcare needs of the patient. For SETMA patients this includes The SETMA Foundation which can help with cost not covered by insurance.
- Care Transitions Coaching. For SETMA, this is done at the time of discharge by the hospital care team, and subsequently by SETMA’s Department of Care Coordination.
- Post-hospitalization Coaching. SETMA’s Care Coordination Department staff makes the hospital follow-up call the day after discharge and schedules other calls as needed..
- Telephone Monitoring Post-discharge. SETMA is adding telemonitoring for targeted conditions such as CHF, Diabetes, etc.
- Medication Reconciliation. Each inpatient event results in four episodes of medication reconciliation: at admission, at discharge, in the care coaching call and then at the follow-up visit. Because all of these are done in the same electronic database, they are additive in their value to the patient’s safety.
- Case Management. This is the new part of the healthcare team. In the past, case management was added on to the care of inpatients but seldom interacted with primary healthcare deliverers. Now they are an integral team and they bring skills and functions which are critical to our goal.
- Self-management Education. If the patient is to be in charge of his/her care 8,760 hours a year, they need educational resources with self-paced learning tools. When a patient or caregiver has a question, the first resource is the secure-web portal for research by the patient or family; the second is a secure message to the provider through the web portal and the last is a face-to-face visit.
As can be seen, the thirteen methods of the HIN survey are not distinct methods in SETMA’s judgment, but elements of one integrated method.
The Baton
“The Baton” is a pictorial representation of the patient’s “plan of care and the treatment plan,” which is the instrument through which responsibility for a patient’s health care is transferred to the patient. Framed copies hang in all pubic places throughout SETMA’s clinics. A poster copy hangs in every examination room. The poster declares:
Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient,
If change is to make a difference
8,760 hours a year. |
 |
The poster illustrates the following seven key princples:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
It must be remembered that when a patient leaves the hospital, until they are seen in the office or home, the provider team member who is in charge of the patient's care is the patient or a family member. Therefore the baton must be successfully passed to the patient, if the coordination, integration, and continuity of care are to be maintained.
The Analytics
To successfully achieve and sustain reductions in readmissions, healthcare organizations must track, audit, and analyze the data.
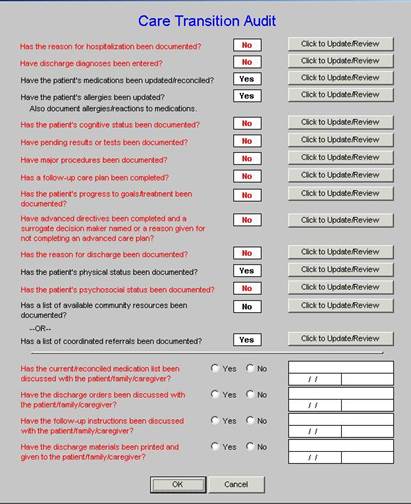
Care Transition - in June, 2009 the AMA released the "PCPI Care Transitions measurement set". This transition audit is one of the tools used to "build" the "baton" and then to make sure that the complete "baton" has been transferred to the next team member. |
 |
Lessons to Date
What we have learned so far is:
- The disease-management model-of-care will not solve this problem. Healthcare providers can’t see patients often enough, give them enough medications, or do enough procedures on them, to effectively reduce readmissions and/or to sustain any reductions which are achieved.
- Care, even within the same organization or system, is still too fragmented to effectively achieve reductions in readmissions. Team building and learning how to effectively use teams are key to this process. SETMA’s current, active effort is to create a “team spirit and collaboration” between four SETMA departments which are working extraordinarily well individually but which are experiencing barriers to a full, integrated, team approach between departments.
- Analytics will be an important part of discovering leverage points for the improving of readmission rates. SETMA has deployed Business Intelligence analytics for that purpose. Because health deteriorates, and on an individual basis and on organizational level, methods must change to respond to that deterioration; it is imperative to continue to redesign the readmissions-reduction effort to keep pace with new realities.
- There is no “silver bullet” for solving the problem of readmissions. A multi-pronged effort will gradually improve readmission rates, until it is suddenly apparent that the system is working. Research will be required to determine the percentage contribution of each element to the success of the effort.
Readmissions rates will always be a challenge. They can be managed effectively with a system such as the one used at SETMA. More details on this system are available under Your Life Your Health by accessing the icons entitled Care Transitions and Care Coordination.
|