|
Yet this was not enough - A System’s Solution to Medication Reconciliation
In 2012, SETMA began thinking that a system’s solution (see Peter Senge, The Fifth Discipline, “The more complex a problem the more systemic the solution must be.”) to medication reconciliation would be a huge step forward in safety and quality of patient care, and in the pursuit of the Institute of Healthcare Improvement’s Triple Aim. Whether addressing care transitions, care coordination, hospital readmissions, or patient safety, medication reconciliation is a key element of success.
In preparation for a visit October 29-November 1, 2012 from a Robert Wood Johnson Foundation research team (see the following link for a description of their research project The Primary Care Team: Learning from Effective Ambulatory Practices (PCT-LEAP): Performance Measures Worksheet - Robert Wood Johnson Foundation), SETMA prepared a 57-page document describing SETMA’s auditing and quality programs. The link above will guide readers to that document. The document addresses SETMA’s solution to care transitions, care coordination, etc. Based on the AMA’s monograph, The physician’s role in medication reconciliation Issues, strategies and safety principles(Making Strides in Safety® program ©2007 AMA) and, AHRQ’s Medications at Transitions and Clinical Handoffs (MATCH) Toolkit for Medication Reconciliation, and other studies SETMA understood the potential benefit for a structured, systemic solution to medication reconciliation.
In addition to effective care transitions (the following link is to SETMA’s performance on the Physician Consortium for Performance Improvement (PCPI) Care Transitions Measurement Set for 2009 through 2016, PCPI Care Transitions -- the next link is to the public reporting by provider name for 2012 Care Transition Audit (Section A), SETMA has established the following steps and principles for medication reconciliation:
We think that forming a coalition with pharmacies, clinicians, patients and IT technology could result in a solution to medication reconciliations which could:
- Reduce the time involved in medication reconciliation to less than two minutes
- Advance a practice closer to perfect medication lists
- Make it easy to reconcile medications at every contact and even when the patient is not schedule for a visit.
- Increase patient safety
- If a D. Pharm consultant is involved in the process, it would even be stronger. I look forward to hearing from you.
The Electronic Age Accelerates the Achievement -- What has brought us to this day in the Spring of 2016?
- March 30, 1998 - Purchase of Electronic Patient Record System
- January 26, 1999 - Foundation laid and SETMA began documenting patient encounters electronically
- May 20, 1999 - SETMA realized that EMR was too expensive and too hard if all we did was document a patient encounter electronically.
- May 20,1999 - SETMA adopted Electronic Patient Management as our goal and began developing chronic disease management tools and clinical decision support
- May 20, 1999 - Defined ten principles of patient-centered medical home
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to every patient encounter what is known, not what a particular provider knows
- Make it easier to do “it” right than not to do it at all
- Continually challenge providers to improve their performance
- Infuse new knowledge and decision-making tools throughout an organization instantly
- Promote continuity of care with patient education, information and plans of care
- Enlist patients as partners and collaborators in their own health improvement
- Evaluate the care of patients and populations of patients longitudinally
- Audit provider performance based on endorsed quality measurement sets
- Integrate electronic tools in an intuitive fashion giving patients the benefit of expert knowledge about specific conditions
- January, 2000 - SETMA began auditing provider performance
- January 2004 - SETMA began using electronics to increase efficiency and excellent of care with process analysis taking complex and difficult tasks and reducing them to simple problems.
- Used electronics to improve medication management with:
- Maintaining of accurate and complete medication lists -- 1999
- E-prescribing of routine medications -- 2010
- Systematizing of Medication Reconciliation
- E-prescribing of controlled substances -- 2014
- Systemic Monitoring of patient use of opioids - 2014
- Reducing Long Term Care use of Antipsychotics - 2014
- Texas Prescription Program - Electronically verifying patient use of controlled substances - 2015.
- Collaboration with NextGen and Surescripts to create an electronic capacity for efficiency, effective and excellent medication reconciliation
The NextGen Solution of Medication Reconciliation in Collaboration with Surescripts
Tutorial for Medication Reconciliation
With the conceptual foundation laid in the first three parts of this series most of the functions which needed for an automated medication reconciliation solution is available now and can be used by going to the NextGen medication module and by clicking on the icon outlined in green below.
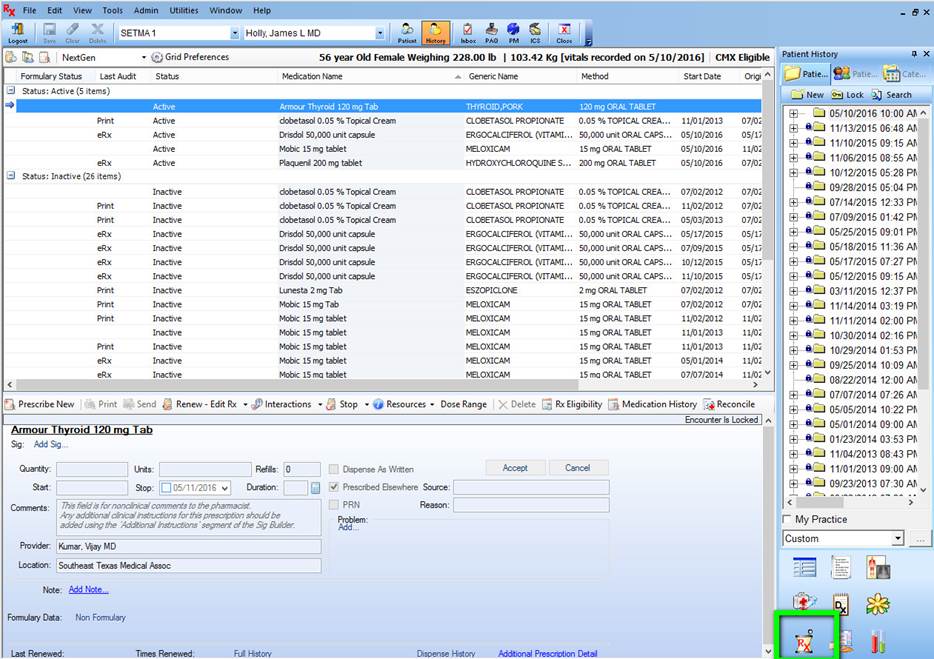
Once on the medication module, you can see if this patient is eligible for use of the automated medication reconciliation by looking at the designation in green below. As long as this does not read “Not Eligible,” you may use the reconciliation function for that patient.
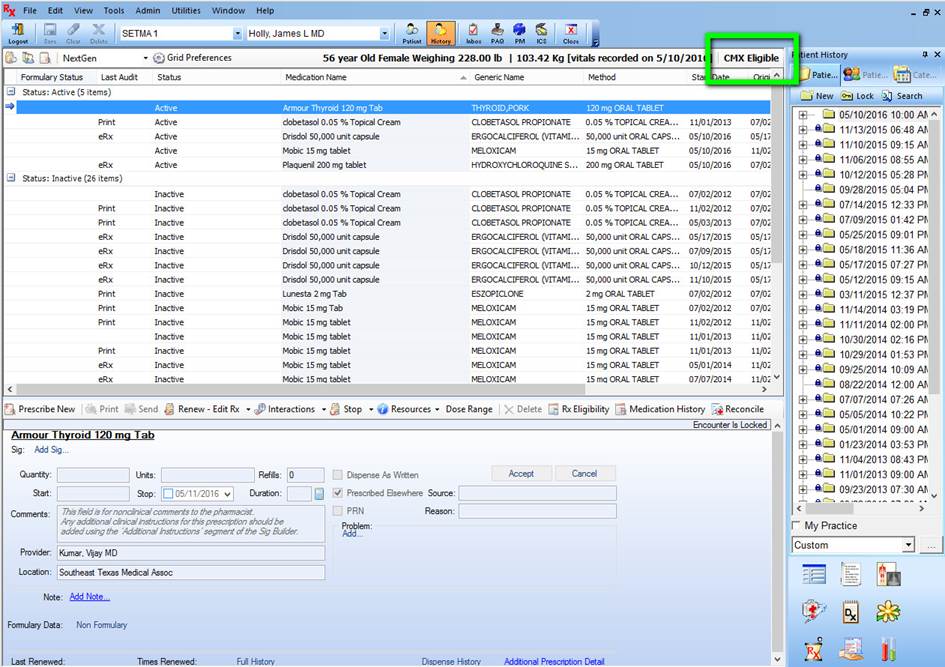
Currently, Surescripts builds their database from medications prescribed from a formulary which is a restricted list of medications which the patients insurance company will pay for. Some new insurance companies, such as the Affordable-Care-Act plans do not yet provide this information. Uninsured patients generally do not have a Surescripts database record. SETMA is currently working with Surescripts and NextGen to expand the access to patient data but what we have gets a good start.
Some medications from Surescripts have “sig” codes and some don’t. (“Sig” stands for “signa” which is the name for the directions on a prescription for taking a medication.) Why do only some medications have “sig” codes? Surescripts’ Medication History data consists of two datasets:
- claims from Pharmacy Benefits Management Solutions (PBMs) and
- dispensed records from pharmacies.
“SIG” codes are contained in pharmacy dispensed records but are not contained in PBM claims. So within the overall medication list, some meds may contain SIG information and some may not.
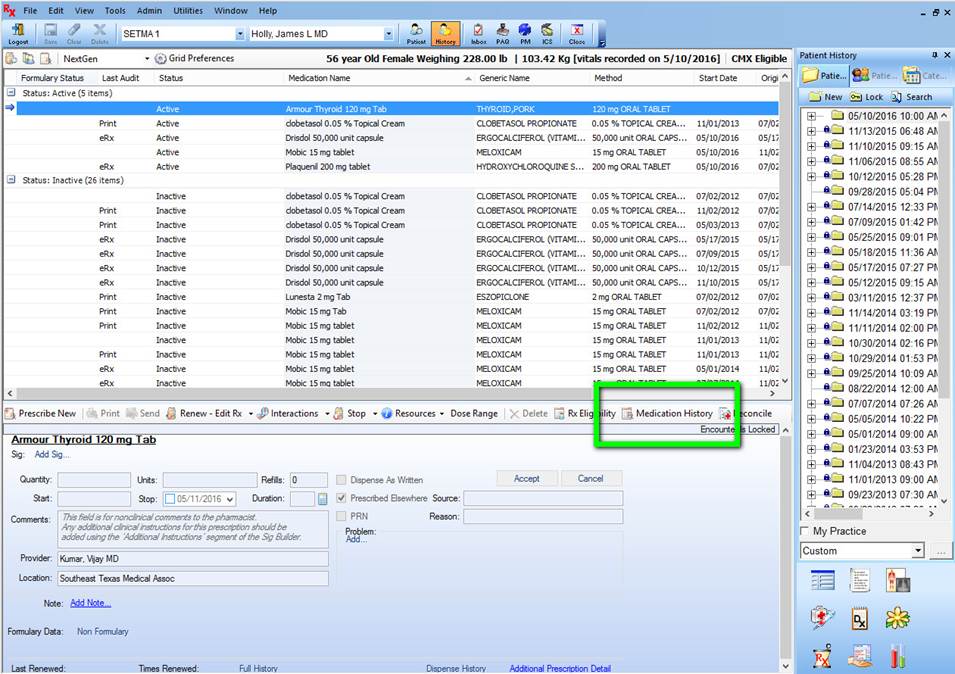
If the record shows that the patient is eligible for medication reconciliation, the provider will click on the button entitled “Medication History,” seen below outlined in green.
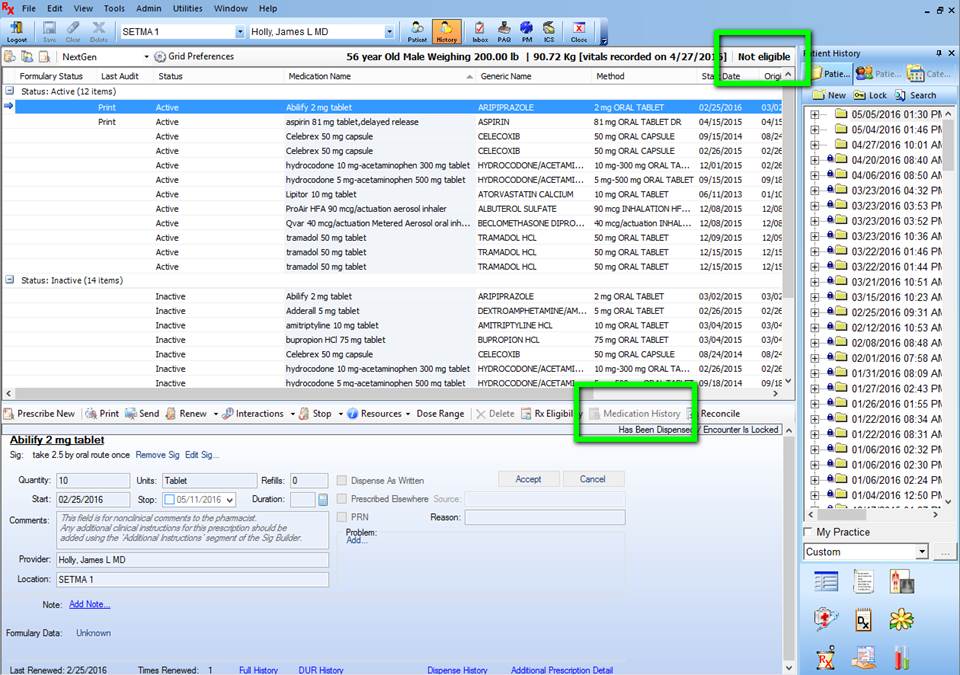
If the patient is not eligible, you will see the designation outline in green below which states, “Not Eligible” and the button “Medication History” will be grayed out.
When the patient is eligible for a “medication reconciliation, the provider will see the following window which states “Status: Has Not Been Requested.” In order to obtain the “medication history” from Surescripts the provider must complete this form.
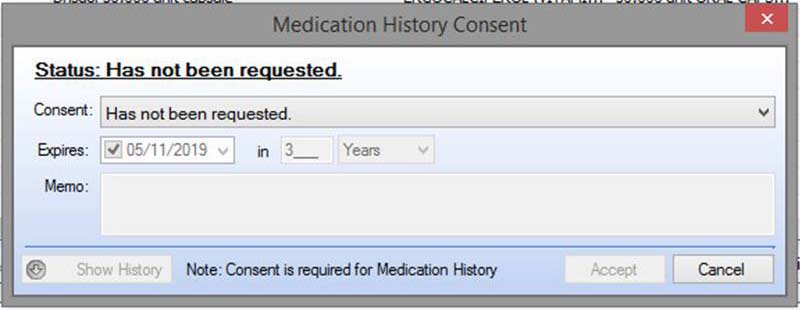
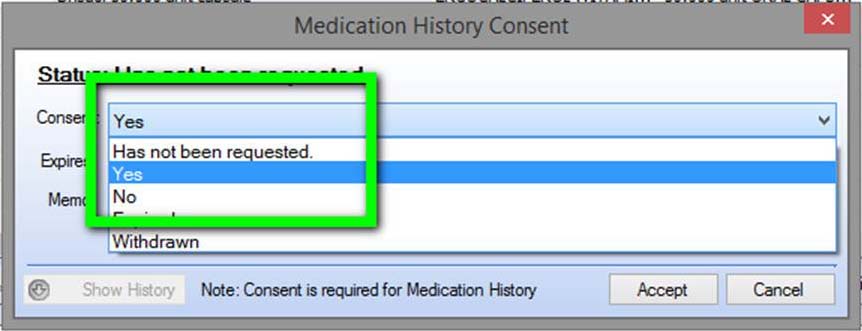
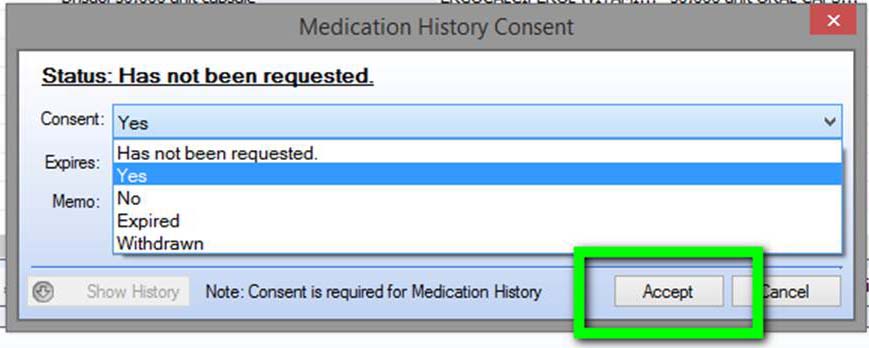
To obtain the “medication history” from SureScripts you must do three things:
- Click on the “Has not been requested” button
- Click on the “Yes” button
- Click on the “Accept” button out lined in the second screen below
Click on “Accept” button below outlined in green.
In the fourth part of this series, the final steps of electronic medication reconciliation will be discussed.
|