|
As we approach the conclusion of this ten-part series on PC-MH, each of which parts relate to continuity of care, creativity of solutions and consistency of performance, we come to “care coordination.” While this seems so obvious to us now, soon to be ten years into our PC-MH pilgrimage, it has not always been obvious. The following is what we have learned.
In addition to the SETMA Model of Care (see: http://jameslhollymd.com/The-SETMA-Way/pdfs/setma-model-of-care-pc-mh-healthcare-innovation-the-future-of-healthcare.pdf), there are many activities which relate to the “heart of patient-centered medical home.” Care Coordination is among them. Addressing the fourth goal of the 2011 National Priorities Partnership, in their report to HHS, the National Quality Forum stated that in regard to care coordination: “Healthcare should guide patients and families through their healthcare experience, while respecting patient choice, offering physical and psychological supports, and encouraging strong relationships among patients and the healthcare professionals accountable for their care... Focus in care coordination by NPP are the links between: Care Transitions- ...continually strive to improve care by ... considering feedback from all patients and their families... regarding coordination of their care during transitions between healthcare systems and services, and...communities. Preventable Readmissions- ...work collaboratively with patients to reduce preventable 30-day readmission rates.”
The principle tool of Care Coordination at SETMA is ‘The Baton.”
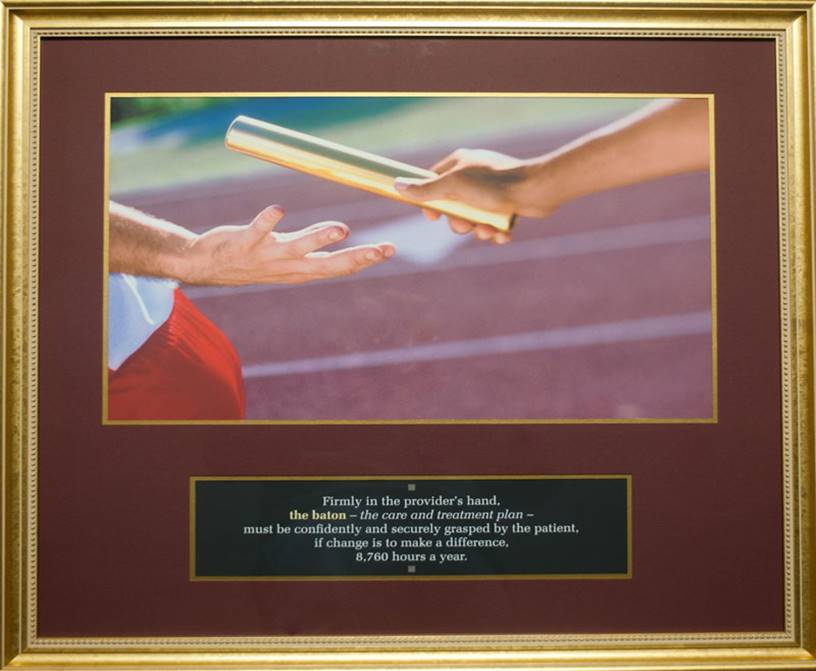
This is a framed copy of "The Baton," which is a representation of the patient's "plan of care and the treatment plan." This is the instrument through which responsibility for a patient's health care is transferred to the patient. Framed copies hang in the waiting room of and hall way of every public place in SETMA. A poster copy hangs in every examination room. The poster declares:
Firmly in the providers hand
--The baton – the care and treatment plan
Must be confidently and securely grasped by the patient,
If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of quality healthcare.
- That the plan of care and treatment plan, the "baton," is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the "baton" which has been developed by the healthcare team, including the patient, is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient's healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider's knowledge is useless to the patient.
- That the imperative is that the plan - the "baton" - is transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient's health.
- That this transfer requires that the patient "grasps" the "baton," i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for "carrying the baton," longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home is symbolized by the "baton." Its display will continually remind the provider and will inform the patient, that to be successful, the patient's care must be coordinated, which must result in coordinated care. Coordination begins at the points of "transitions of care," and the work of the healthcare team - patient and provider - is that together they evaluate, define and execute that care. The most common and frequent transition of care is when the patient leaves the provider’s office.
As the Baton is the “tool” of coordination, the philosophy of coordination is contained in the statement that, “Convenience Is The New Word For Quality.”
At the HIMSS Leaders & Innovators Conference held at Amelia Island in November, 2011, Mark Bertolini, Chairman, CEO & President of AETNA said, “Convenience is the new word for quality." The statement on its face seems an oversimplification. How can doing things, the way patients want, when they want, where they want and how they want, contribute to the achievement of quality outcomes?
In 2009 and 2010, as SETMA became a Tier III, PC-MH, and as we struggled with the concept of “care coordination,” we prepared over 50 articles on PC-MH. On August 18, 2011, three months before Bertolini’s addressed, SETMA published an article entitled: Medical Home Series III Part VII Care Coordination” (see: http://jameslhollymd.com/your-life-your-health/Medical-Home-Series-Two-Part-VII-Care-Coordination).
This article in part stated, “As with most issues of quality care in the 21st Century, a process has an outcome and a metric may measure one or the other.” The article continued: Coordination of Care is the process an organization goes through to assure that patients receive the care they need and Coordinated Care is the outcome, i.e., the experience and perception the patient has when the care has been organized for continuity, for convenience and for compliance.”
Care Coordination involves the following five elements:
- Collaboration
- Convenience
- Comprehensiveness
- Connection
- Communication and Continuity
Initially, the idea of convenience in the scheduling of multiple appointments at the same time was the extent of SETMA's understanding of this element of coordination. Eventually, "convenience" was translated into the understanding that coordinated care means more than just making patients comfortable; it meant and it resulted in:
- Convenience for the patient, which
- Results in increased patient satisfaction, which contributes to
- The patient having confidence that the healthcare provider cares for the patient personally, which
- Increases the trust that the patient has in the provider, all of which
- Increases compliance (adherence) in the patient obtaining healthcare services recommended, which
- Promotes cost saving in travel, time and expense of care, which
- Results in increased safety, quality of care and cost saving for the patient.
This requires intentional efforts to identify opportunities to:
- Schedule visits with multiple providers on the same day, based on auditing the schedule for the next 30-60 days to see when a patient is scheduled with multiple providers and then to determine if it is medically feasible to coordinate those visits on the same day.
- Schedule multiple procedures, based on auditing of referrals and/or based on auditing the schedule for the next 30-60 days to see when a patient is scheduled for multiple providers or tests, and then to determine if it is medically feasible to coordinate those visits on the same day.
- Scheduling procedures or other tests spontaneously on that same day when a patient is seen and a need is discovered.
- Recognizing when patients will benefit from case management, or disease management, or other ancillary services and working to provide the resources for those needs.
Convenience is a process, not an outcome of coordination of care. Therefore, SETMA formed a Department of Care Coordination and created a convenient method for enlisting that department in a patient’s care.
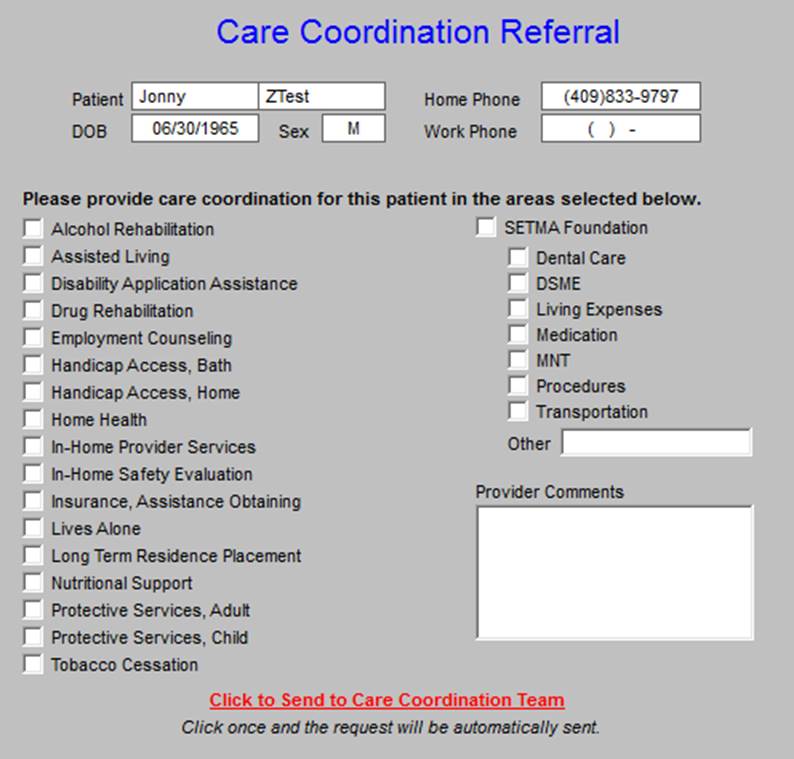
This template allows the provider and/or nurse to send an e-mail to the Department of Care Coordination, which helps find resources for a patient's special needs. Several functions are included with this template:
If a provider completes three or more referrals in any given encounter, an e-mail is automatically sent to the Director to allow for the coordination of those referrals to increase convenience and compliance.
It was only through this analysis that we accepted "convenience" as a worthy goal of quality care as opposed to it only being a means of "humoring" patients. This fulfilled SETMA's goal of ceasing to be the constable, attempting to impose healthcare on our patients; and, to our functionally becoming the consultant, the collaborator, the colleague to our patients, empowering them to achieve the health they have determined to have.
|