|
How do you design a quality improvement project in outpatient ambulatory care? In our community - Southeast Texas, which comprises a five-county geographic - there is a hospital which has always impressed me. The reason? Historically, they have begun one project, as they completed another project, as they designed another. This continuum, based on strategic planning, has always intrigued me. This dynamic character of a growing organization is a good pattern to follow.
On April 8, 2010, Southeast Texas Medical Associates (SETMA) completed a 14-month project of beginning the transformation of our practice into a Patient-Centered Medical Home (PCMH). On April 23, 2010, we will complete an eight-month Phase I and Phase II of our COGNOS Project. This project is described on our website at www.jameslhollymd.com under both Your Life Your Health and Public Reporting. This is a part of our PCMH transformation. COGNOS is IBM's Business Intelligence, data-mining , software. SETMA has collaborated with a consulting firm LPA Systems (www.LPA.com) to create the ability to do re-time auditing of quality metrics and to publicly reporting of provider performance displayed statically from structured audits and dynamically with digital dashboard displays of comparative and population data.
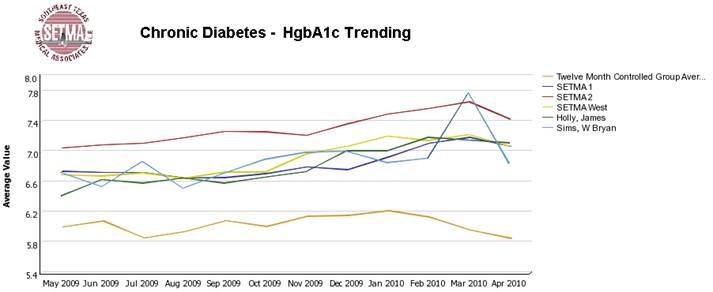
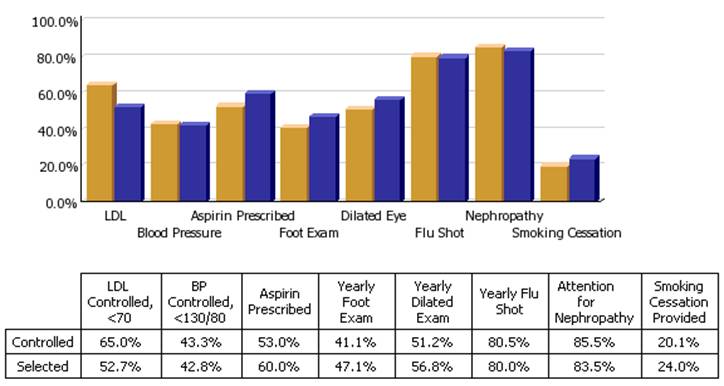
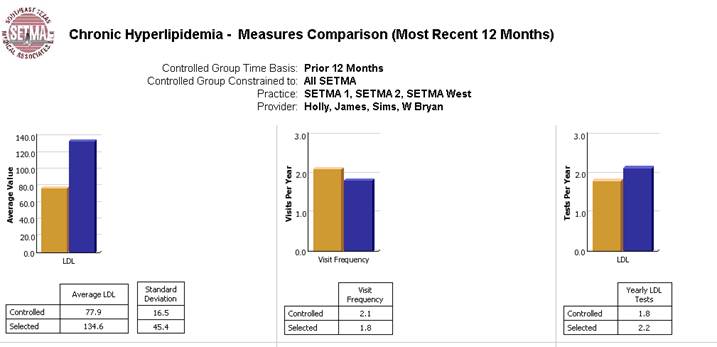
Through COGNOS, data can be analyzed by provider, practice, clinic, and over any period of time. Pre-visit audits of preventive health and screening health quality metrics can be done and given to providers before each day's visits. Also, at the time of a visit, with the click of a button, the provider can display the patient's status on fulfillment of quality metrics published by NCQA (HEDIS), Ambulatory Care Quality Alliance (AQA), Physician Consortium for Performance Improvement (PCPI, Diabetes, Hypertension, CHF, Chronic Stable Angina, Chronic Renal Disease Stage IV-V, Care Transitions, etc), National Quality Forum (NQF, over 50 quality metrics), Physician Quality Reporting Initiative (PQRI, multiple comprehensive groups), and quality audits which SETMA has designed in the absence of published ones, such as Lipid Management, Elements of Hypertension not included in other metrics, and Chronic Renal Disease Stage I-III.
COGNOS also gives SETMA the ability to examine population-management performance by socio-economic and ethnic groups as well as by payer class. This was suggested to SETMA by the Senior Vice President for Quality Performance and Improvement for Massachusetts Blue Cross Blue Shield. The purpose is to examine whether we have, as we think, eliminated the disparities of care commonly reported for the economically disadvantaged and for certain ethnic groups. We are also able to compare SETMA's total patient population with subsets of that group. For instance, we can compare patients who have been treated to goal for diabetes, lipids or hypertension with our patients who are not at goal. We can examine frequency of visits and testing, gender, age, or severity of illness to see if patterns exist which would suggest ways in which to improve the care of those subsets.
We believe that this real-time, comparative and longitudinal data will show us how to improve the quality of care which all of our patients receive. The following are illustrations of these capacities
Why can we do this?
These audits are possible because over the past 12 years, SETMA has designed disease- management tools which automatically captured provider performance and allow providers, at the time of care and at the point-of-service to evaluate their own performance without any additional work, other than the click of a single button. Herein, we find a critical principle of designing a quality improvement initiative: it is both built upon past work and the new process is a logical extension of the previous work. A new initiative typically will not be built in isolation.
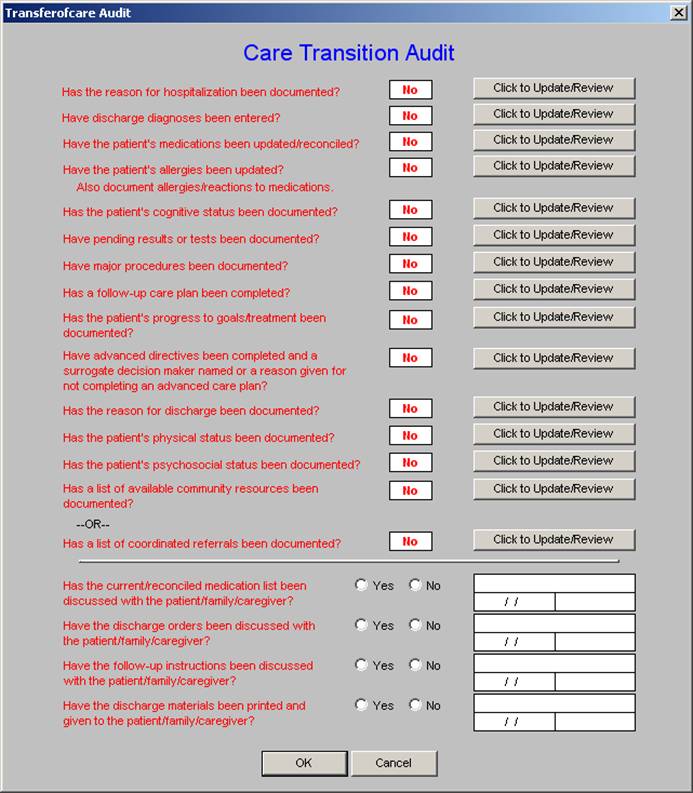
An illustration of this is PCIPI's Care Transition quality metrics. This is a comprehensive data set which deals with the transition of a patient from inpatient to outpatient care, or from the emergency department to the outpatient setting. The AMA published the Care Transitions data set in June, 2009. When SETMA saw the data set, it was apparent that with the addition of only two data points, our electronically-generated Discharge Summary fulfilled all 14 data points and 4 actions required of Care Transitions. As a result, because of the previous work, this project took two days to complete and since June, SETMA has performed at 100% compliance with this quality audit.
Again, to give a mental picture, the following is what the Care Transition audit looks like. The data points required are captured automatically by the computer. If any data point is missed in the discharge summary, it is possible to click a button, which automatically returns you to the part of the discharge summary which addresses that issue. This fulfills one of SETMA's standards of software development: "Make it easier to do it right than not to do it at all."
Thus the first two elements of the design of a quality initiative are:
- Begin the design of a new project while you are completing a project.
- Build upon past work and design a function which is a logical extension of what you have already done.
Both of these principles will contribute to your success. A third element of design is the selection of a quality initiative which will leverage your resources in improving care and/or in improving outcomes. As SETMA is completing multiple projects and as we are initiating other projects, we began to think of how we could leverage our COGNOS project in improving patient care and patient satisfaction while achieving cost savings and fulfilling quality metrics..
Auditing Re-Admission Rates: Process and Outcomes Analysis
The selection of the auditing and evaluation of re-admissions fit all of our criteria:
- We have the capacity to do this audit because of previous work.
- It is a matter of national interest and concern due to the cost of preventable readmissions.
- It will increase patient satisfaction, safety and quality of care.
- Because SETMA has a population of patients for which we are "at risk" financially, this initiative has potential positive economic implications, also.
The fourth principle of design is to think about it. What do you want to accomplish? "Thinking" will most often take the form of questions which you want to ask of your data. In the re-admissions audit, we want to:
- Know what our readmission rate is by condition.
- Are there discernable differences between patients with similar conditions who were and who were not readmitted in 60 days?
- If those differences exist, can we leverage that information into decreasing readmissions?
The fifth principle of design is to examine whether you have done things in the past which have made a difference in our re-admission rates?
- SETMA instituted the Transitions of Care audit; has that made a difference?
- SETMA began calling all patients discharged from the hospital; has that made a difference?
We are completing an audit right now to examine these questions. This audit is complex and time consuming, unlike the COGNOS audit which we will build. Building the COGNOS audit is complex and time consuming but once it is one, it is quick and efficient to use.
The sixth principle of design is to develop an algorithm based on the above, which allows you to create an electronic audit out of which data will become information. Once data is transformed into information you can make treatment decisions which will make a difference.
The final step - the seventh - is to be prepared to make changes based on the data and information you develop. You must be aware, however, that if you are going to make a change, it must make a difference. Quality initiatives which change a process have no value until they make a difference in the outcome. It is important to analyze the process and to design the process, but until that process results in improved outcomes, it is no worth doing.
Where is SETMA in the design of a Re-Admission Quality Audit?
SETMA started the design process on April 12th. This is being written on April 13th. Thus far, we have gone through the following steps:
- We are starting a new project as we complete another.
- We are building upon passed work and designing a quality initiative which is a logical extension of our previous work.
- This project will leverage our resources in improving care and/or in improving outcomes
- We have though about this project and have enunciated multiple questions we want to answer.
- We believe we have done things in the past which have impacted re-admissions and we will analyze that question.
- The following is the algorithm which will guide our development of this auditing tool.
Algorithm for analyzing re-admissions in order to improve our performance.
The following data points will be required in the audit:
- Diagnoses (COPD Exacerbation, Chronic Stable angina, CHF)
- Date of Discharge
- Date 60 days hence
- Length of stay
- Was the patient with one of these targeted diagnoses admitted for a procedure or for a scheduled admission
- Payer class
- Ethnicity
- Socio-economic group
- Barriers to care
- Patient lives alone or not
- Patient receiving ancillary care (Home Health, Case management, physician therapy, hospice)
This audit will require the addition of two data points: length of stay and whether the admission was scheduled or not. The following information will be required in order to complete the process-auditing:
- Patients readmitted within 60 days for one of the targeted conditions
- Patients not readmitted within 60 days for one of the targeted conditions.
- Were the patients readmitted seen in the clinic prior to be re-admitted?
- What was the length of time between discharge and readmission?
- What was the length of time between discharge and being seen in the clinic for those re-admitted and for those not re-admitted?
- Was the Transition of Care completed on both groups consistently?
- Was the follow-up call successfully completed with both groups?
- At the time of the post hospital follow-up call, did those re-admitted indicated:
- That they were improved following hospitalization.
- That they had their medications.
- That they had their follow-up appointments.
- How many times did those re-admitted and those who were not call the clinic in the sixty days following discharge.
- Did the patients who were re-admitted have any unanswered telephone contracts with the clinic?
- Was there a severity of disease distinction between those re-admitted and those who were not? The metrics for this measure will be:
- CHF - BNP value, Ejection Fraction, CHF Stage
- COPD --- Pulse oximetry, TV,
- Angina Pectoris - Canadian Cardiovascular Society Classification System
- Were quality metrics met at discharge and/or at any point before readmission for CHF, Chronic Stable Angina, COPD
- Was the patient contacted by the clinic, provider or disease management within 7 days of re-admission.
- If a patient, who was re-admitted, called for an appointment, how long was it before an appointment was given?
- Did the re-admission take place between the "call for an appointment" and the appointment?
Once this algorithm is in place, the following data will be computed:
- Rate of re-admissions adjusted for scheduled admissions.
- Rate of re-admission by payer class (Medicare Advantage, Medicare. Medicaid, Blue Cross, etc )
- Rate of re-admission by ethnicity
- Rate of re-admission by socio-economic group
- Rate of admission for those who live alone, or who have a poor support group
Administrative Issues related to Re-admissions
- The following patient satisfaction survey will be completed by the patient and by the principal care giver on all re-admissions. (to be designed to include many of the above data points).
- SETMA will establish a readmission program which will include a weekly telephone call and/or a weekly home visit for the 60 days following discharge after a re-admission.
- We will establish a case management and/or disease management protocol for patients with readmissions for the same cause within 60 days.
When this process is complete, SETMA will publish another article which will show the result of this design process.
|