|
Your Life Your Health for September 30, 2010, described SETMA's Diabetes Screening and Prevention Program. That program includes:
- Identifying those who are at high risk of developing diabetes and screening them every three years for diabetes.
- Documenting those who have pre-diabetes, which places them in an even higher risk for the development of diabetes and screening them annually for diabetes.
- Distinguishing between the two groups of pre-diabetes which are Impaired Fasting Glucose (IFG) and Impaired Glucose Tolerance (IGT). While both need aggressive intervention to prevent the development of diabetes; patients with IGT are an even higher risk of developing diabetes than patients with IFG.
(Remember, IFG is diagnosed when your fasting blood sugar is 100 to 125 mg/dl. IGT is diagnosed when your 2-hour blood sugar is between 140-199 mg/dl, during a two-hour glucose tolerance test.)
Don't Get it
When it is possible, the best way to treat diabetes is still "don't get it." For patients with Type 1 Diabetes, there was nothing they could have done to prevent the disease, but for many people who will develop Type 2 Diabetes, it is possible either to delay the onset of the disorder, or to prevent it completely.
As SETMA assumes the mantle of being the Diabetes Center of Excellence Affiliate in Southeast Texas, we have renewed our commitment to make certain that we identify all patients with diabetes through proper screening and to help all patients at risk for the development of diabetes to know what they can do to prevent the disease.
All patients at SETMA are accessed by the "screening recommendations" discussed last week. All patients who are "at risk" for the development of diabetes will be evaluated by the complete Diabetes Prevention Program. Upon the completion of that evaluation, the following note will be generated and given to the patient. Each note is personalized and contains the patient's personal and individual data and calculations. The following example is from a real patient who was seen at SETMA recently.
Preventing Diabetes Note
According to evidence-based studies, patients who have a low risk of developing diabetes have the following characteristics:
- have a low BMI
- consume a diet high in cereal fiber
- consume a diet high in polyunsaturated fat
- consume a diet low in trans-fatty acids
- consume foods with a low glycemic index
- engage in moderate to vigorous physical activity for at least 30 minutes each day
- do not smoke
- do not consume more than 5 grams of alcohol per day (A standard drink in the United States contains 14 grams of pure alcohol -- about 0.6 fluid ounces or 1.2 tablespoons.)
(Note: The Glycemic Index has been discussed before. There is information on this subject at www.jameslhollymd.com under Your Life Your Health. Essentially, it refers to how quickly a food is turned into sugar in the body. The higher the glycemic index, such as in refined sugar or simple carbohydrates, the more insulin demand is placed on the body)
Screening Recommendations
The following are factors which indicate that screening for diabetes should be initiated in you.
- Age > 45 years of age
- Family history of diabetes
- Dyslipidemia
- Hypertension
Each of these increase your risk of developing diabetes and careful attention should be taken to control each of them which are subject to change.
Predicting The Development of Diabetes in Older Adults
At SETMA, we use a prediction calculator to determine your risk of developing diabetes as an older adult. The four factors of the score are
- your age,
- your sex (females have a higher risk),
- your fasting blood glucose results and
- your triglycerides results.
You have a total score of 4 points.
Because your score is less than 5 points, you are not at an increased risk of developing diabetes. But, you should continue to take steps to maintain a healthy body weight, exercise regularly and avoid smoking to keep your risk of developing diabetes low.
Screening for Insulin Resistance
Remember, when your liver and your muscles do not response to insulin, you have "insulin resistance," which is the first step toward the development of diabetes. The following are factors which increase the likelihood of insulin resistance in you.
- Family history of diabetes, hypertension, or CVD
- Age > 40 years
The following are abnormalities of insulin resistance syndrome which are present in you.
- Elevated triglycerides €“ Your Triglycerides - 90 mg/dL
- HDL - 54 mg/dL
- Elevated blood pressure €“ Your Blood Pressure - 130 / 72 mmHg
- Fasting Glucose - 97 mg/dL
- 2 Hour OGTT €“ not done
Conclusion - You have one or more risk factors AND two or more abnormalities which indicate the presence of the insulin resistance syndrome.
Questionnaire - Could You Have Diabetes And Not Even Know It?
- My weight is abnormal as indicated by my BMI or body fat percentage? Yes
- I am 65 years old or older? Yes
Point Total - 14 points
Conclusion - You are at greater risk for having diabetes. Talk with your health care provider to determine if you have diabetes.
Fasting Lab Results
FPG - 97 mg/dL
Cholesterol - 183 mg/dL
HDL - 54 mg/dL
LDL - 111 mg/dL
Triglycerides - 90 mg/dL
Magnesium - 2.5 mg/dL
Plan of Care and Treatment Plan
Because you :
- are over 65 years of age
- have hyperlipidemia
- have hypertension
you should take steps to lose weight, exercise and stop smoking to help lower your risk of developing diabetes.
Review your LESS Initiative carefully. It will guide you in taking the steps mentioned above. If you want or need help, ask your healthcare provider to refer you to:
- Medical Nutrition therapy for nutritional counseling
- Physical Therapy for an exercise program
- Group weight management therapy
Progression to Type 2 Diabetes
The progression from normal glucose tolerance to Type 2 Diabetes involves two processes:
- insulin resistance
- decreased insulin production by the pancreas
Insulin resistance exists when the liver and muscle have a decreased response to insulin. As a result the pancreas produces a great deal more insulin in an attempt to compensate for the decrease response to insulin. Initially, plasma glucose levels are maintained in the normal range but gradually the pancreas is unable to "keep up" with the demands for more insulin. The cells which produce insulin - called beta cells - begin to fail in the production of insulin and the increased sugar in the blood actually results in the destruction of beta cells further decreasing the capacity to produce insulin.
The first abnormality that is detected is a rise in the glucose levels after meals because of reduced "first-phase insulin" secretion. "First-phase insulin" is the insulin which has been stored in the Beta cells and is the fastest to respond to the increase of sugar caused by a meal.
With time, further decline in beta-cell function leads to elevation of the fasting glucose levels. Eventually, diabetes occurs. The following graph illustrates this process. Most people who develop diabetes have a genetic pre-disposition to diabetes. This is assessed by determining whether anyone in the family has diabetes. Age, obesity and inactivity are called "acquired" causes of diabetes. Obviously, you can only change two of these, but as you get older, it is more and more important to control your weight and to maintain your exercise and active lifestyle. The problem, of course, is that both weight loss and exercise are often more difficult to do both as we get older.
Once "insulin resistance" develops, the body "compensates" by producing more insulin. Eventually, due to increasing demands and to decreasing production of insulin the body is not able to compensate and impaired fasting glucose develops followed by progression to impaired glucose tolerance and then full blown diabetes.
At any point that you decide to take charge of your health, lose weight, exercise, stop smoking and change what you are eating, you can slow or reverse your progression to diabetes.
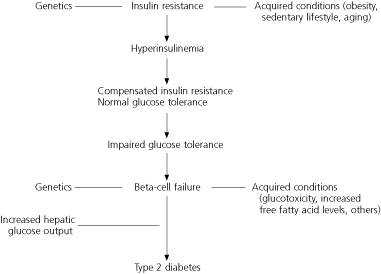
Figure 1. Etiologic sequence for the development of type 2 diabetes.
Results of Evidence-Based Studies and Lifestyle Interventions
Recent studies of patients with IGT have shown success for lifestyle interventions in delaying or preventing the development of diabetes. There is strong evidence that a structured program of diet and exercise can reduce the risk of progression to type 2 diabetes in patients with IGT. Patients with IFG and IGT should be advised on the benefits of modest weight loss, good dietary habits, and regular physical activity.
In the Diabetes Prevention Program, 3,234 patients with IGT and a BMI greater than 24 were assigned to one of the following groups: placebo, metformin (Glucophage), or intensive lifestyle modification. The lifestyle modification group was offered a 16-lesson curriculum aimed at achieving a weight loss goal of more than 7 percent of their initial body weight through a low-calorie, low-fat diet and moderate-intensity exercise for 150 minutes per week.
After an average follow-up of 2.8 years, there was a 58 percent relative risk reduction in the progression to diabetes in the lifestyle intervention group compared with the placebo group. The relative risk reduction was 31 percent in the metformin group compared with the placebo group. In this study, lifestyle intervention was effective in men and women, and in all ethnic groups. It was most beneficial in patients older than 60 years; in this group, it reduced the incidence of diabetes by about 71 percent.
Finnish Diabetes Prevention Study
In the Finnish Diabetes Prevention Study, 522 obese patients with a mean BMI of 31 and IGT were assigned to a control group or an intervention group. Patients in the intervention group were instructed to lose 5 percent of their body weight, limit fat intake to less than 30 percent of daily calories, limit saturated fat intake to less than 10 percent of daily calories, increase fiber intake to at least 15 g per 1,000 calories, and exercise moderately for at least 150 minutes a week.
After 3.2 years of follow-up, there was a 58 percent relative risk reduction in the incidence of diabetes in the intervention group compared with the control group. There also was a significant positive correlation between the ability to achieve lifestyle modifications and preventing progression to diabetes.
Da Qing IGT and Diabetes Study
In the Da Qing IGT and Diabetes Study in China, 577 patients with IGT were assigned to a control group or to one of three treatment groups: diet alone, exercise alone, or diet plus exercise. Over six years of follow-up, the relative risk reduction in progression to diabetes was 31 percent in the diet group, 46 percent in the exercise group, and 42 percent in the combined group.
To Prevent Diabetes the Recommended Lifestyle Changes
- Fat: <25 to 30 percent
- Saturated fat: <10 percent
- Carbohydrates: 50 to 60 percent
- Protein: 15 to 20 percent
- Daily fiber intake: >15 g for every 1,000 calories consumed
- Foods: salad, vegetables, fruits, whole grains, fish high in omega-3 fatty acids, legumes, lean meat; minimal intake of refined sugars
- Exercise: moderate-intensity physical activity, such as brisk walking or biking, for 150 minutes per week
- Weight loss goal: 5 to 7 percent of body weight
- Counseling by professionals on weight reduction and exercise with regular follow-up and reinforcement.
Pharmacologic Agents
Although not as effective as lifestyle interventions, drug therapy with metformin and acarbose (Precose) has been shown to prevent the progression of IGT to diabetes.
In the Diabetes Prevention Program, treatment with metformin was associated with 31 percent relative reduction in the progression of diabetes in patients with IGT. Metformin was more effective in younger patients with a higher BMI and higher fasting plasma glucose levels, and was least effective in patients older than 60 years.
In the Study to Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM), patients with IGT who were treated with acarbose showed 25 percent relative reduction in progression to diabetes. This risk reduction did not persist when acarbose therapy was discontinued at the end of the study. The incidence of diabetes increased in the group that originally had been treated with acarbose, indicating that this drug therapy must be continued to maintain preventive effects.
Final Comments
Lifestyle interventions can be difficult to implement because it is impractical for the usual family practice systems to provide intensive dietary and exercise interventions similar to those used in clinical trials. However, lifestyle interventions are highly effective and superior to drug therapy, and should be the first choice in treating patients with IGT or IFG.
Although pharmacologic agents have been shown to be successful in preventing or delaying the onset of diabetes, whether these agents can prevent complications of diabetes or protect against cardiovascular disease remains unknown. Routine use of pharmacologic agents as a substitute for lifestyle modification should be discouraged until more studies have been conducted and the cost-effectiveness of drug therapy has been assessed. A healthier lifestyle can modify other risk factors for cardiovascular disease such as obesity, hypertension, and dyslipidemia. Drug therapy can be considered when aggressive lifestyle interventions are unsuccessful.
Summary
These are the facts. The fact is you can make a difference in your future health by making a change now. The fact is if you ignore your weight and exercise, you may develop diabetes, but if you lose weight and exercise, you will significantly reduce your risk.
|