|
On January 24, 2011, the Archives of Internal Medicine published an article which examined whether electronic health records and clinical decision support functions in EHRs improved quality outcomes. The conclusion was:
"Our findings indicate no consistent association between EHRs and CDS and better quality. These results raise concerns about the ability of health information technology to fundamentally alter outpatient care quality." Electronic Health Records and Clinical Decision Support Systems Impact on National Ambulatory Care Quality
Process and Improvement
This conclusion is not surprising and should have been expected. Typically, a change in process will not result in a change in outcome until process is internalized and is transformed into a personal passion. Simply using an electronic means of documenting a patient encounter should not be expected to change the outcome of patient care in and of itself. Process change alone is not unlike results from reform (external pressure), which are limited; real and sustainable improvement in outcomes will only come from transformation which is an internalization of the elements of the process change such that those changes become a personal passion. It is then that care quality improvement will result.
The difference between the present reality and the desired change in outcome will create what Peter Senge refers to as "creative tension."
- "Creative Tension" will occur in an organization when "process becomes passion." When the goal is internalized and becomes a product of "generative" (creative) thinking and a personally felt pressure to change (i.e., "creative tension"), both of which exist independent of external pressures of reform, outcomes will improve.
- Health reform employs external pressure to reshape healthcare delivery into a desired pattern. It produces results only as long as rules, regulations, requirements and restraints squeeze the system into a desired form. Unfortunately, it is not generative and is not self-sustaining. When the pressure decreases, the changes disappear.
- Healthcare transformation will result from internalized ideals which create vision and passion, both of which produce and sustain "creative tension" and "generative thinking." Transformation is not the result of pressure and it is not frustrated by obstacles. In fact, the more difficult a problem is, the more power is created by transformation in order to overcome the problem.
It is here that we see the application of Peter Senge's The Fifth Discipline to medical information technology most clearly. It is here where we discover why EHR alone does not produce improved quality outcomes.
The following concepts derive from Senge's systems principles:
- Healthcare delivery is not improved simply by the providing of more information to the healthcare provider at the point of care.
- Healthcare delivery is improved when the organization of that information is such that there is a dynamic interaction between the provider, the patient, the consultant and all other members of the healthcare equation, as well as the simultaneous integration of that data across disease processes and across provider perspectives, i.e., specialties.
- Healthcare delivery is not necessarily improved when an algorithm for every disease process is produced and made available on a handheld, pocket-computer device but it is improved when the data and decision-making tools are structured and displayed in a fashion which dynamically change as the patient's situation and need change.
- Healthcare delivery also improves when data and information processed in one clinical setting is simultaneously available in all settings. This improvement does not only result from efficiency but from the impact the elements contained in that data set exert upon multiple aspects of a patient's health. In this way, the data reflects the dynamic within the system under analysis, which in the case of healthcare is a living organism which is constantly changing.
- Healthcare is improved when there is simultaneous evaluation of the quality of care as measured by evidenced based criteria is automatically determined at the point of and at the time of care. Healthcare is improved when the data display makes it simple for the provider to comply with the standards of care, if the evaluation demonstrates a failure to do so.
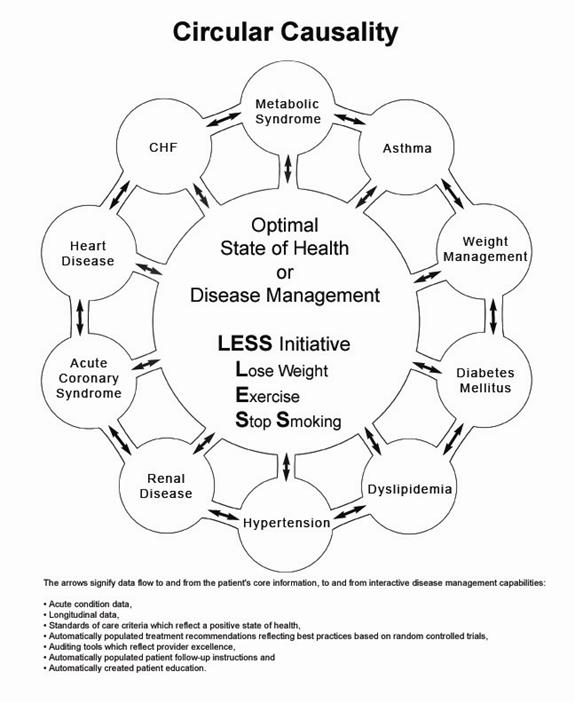
- Healthcare is also improved when data can be displayed longitudinally, demonstrating to the patient over time how their efforts have affected their global well-being. This is circular rather than linear thinking. A person begins at health. Aging and habits result in the relative lack of health. Preventive care and positive steps preserve, or restore health.
- Healthcare improvement via systems will require dynamic auditing tools which give the provider and the patient immediate feedback on the effectiveness of the care being provided and received.
The Foundation of EHR Design which produces improved outcomes
If excellent healthcare requires healthcare organizations:
- to be "learning organizations"
- to avoid "learning disabilities"
- to think in a circular rather than in a linear fashion
- to look at "dynamic complexity" rather than "detail complexity"
then how would data need to be displayed to support these functions?
If health science has the capacity:
- To create far more information than anyone can absorb,
- To foster far greater interdependency than anyone can manage
- To accelerate change far faster than anyone's ability to keep pace.
then how can electronic patient records and/or electronic patient management help solve these problems and make it possible for healthcare providers to remain current and fulfill their responsibility of caring for patients with the best treatments available?
First, the data organization must see the patient:
- As a whole rather than as a summary of many different parts; this requires a circular perspective of a patient's life.
- As a living organism rather than as a disease process; this requires a circular perspective of a patient's life.
Second, the data organization and management must:
- Encourage and provoke change in patient behavior.
- Encourage and provoke change in provider behavior.
- Provide feedback to the provider at the point and time of service whereby the excellence of care can be measured.
Third, the data manipulation must have:
- Multiple points of entry
- Easy and dynamic interaction between the various elements of the database
- Automatic summarizing of the patient's care as measured against evidenced-based criteria
This mental model has resulted in the principles which have guided Southeast Texas Medical Associates' development of an EHR data base which produces change. These principles have guided SETMA to:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets, HEDIS, NCQA, NQF, PQRI, AQA and other measure sets..
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
Dynamic Complexity
The problem with biological systems is that change, even change which results in deterioration of health, does not occur quickly and it often occurs without any signs or symptoms until the illness, or disease process has already caused significant damage.
Senge defines "dynamic complexity" as a situation "where cause and effect are subtle, and where the effects over time of interventions are not obvious." This perfectly describes the development of many disease states and the benefit of their treatment. We know that obesity causes, or contributes to most diseases including diabetes, hypertension, heart disease, cancer, etc. In these conditions, "obesity" is the cause; "cancer" is the effect, but the change is slow and is not apparent. Also, the results of treatment are very slow. Consequently, it is hard to sustain the changes necessary to eliminate the "cause," which is obesity, in order to avoid the "effect" which is cancer.
Shifting the Burden
There are structural problems which aggravate the obvious solutions to a business or a health problem; Senge addresses one of these and calls it "the shifting the burden." He defines "shifting the burden," as "an underlying problem generates symptoms that demand attention. But the underlying problem is difficult for people to address, either because it is obscure or costly to confront. So people €˜shift the burden' of their problem to other solutions - well intentioned, easy fixes which seem extremely efficient. Unfortunately, the easier €˜solutions' only ameliorate the symptoms; they leave the underlying problem unaltered. The underlying problem grows worse, unnoticed because the symptoms apparently clear up, and the system loses whatever ability it had to solve the underlying problem."
This happens in healthcare when a person looks to healthcare providers or medications to solve a problem which can only be solved by their own habits, choices, decisions and resolution. A pill, or a procedure, or a prescription is sought in order to overcome the "obesity." It will work for a short while but not long term. When it fails, more aggressive interventions are tried without addressing the fundamental problem.
The Quick Fix Deception
Senge's business prescription is a good one for healthcare, also. He says, "Beware the symptomatic solution...that address only the symptoms...not fundamental causes, tend to have short-term benefits at best. In the long term, the problem resurfaces and there is increased pressure for symptomatic response. Meanwhile, the capability for fundamental solutions can atrophy." (p. 104) Senge adds, "The 'easy solution...the 'quick fix'...solves the problem temporarily...(but) a shifting of burden structure lurks behind many 'solutions' (and) explains a wide range of behaviors where well-intentioned 'solutions' actually makes matters worse over the long term." (p. 107)
Senge and Medicine
The longer a person delays addressing the "real" cause of their problem, the fewer options and the fewer resources they have for dealing with the "real" cause of the problem. For instance, the longer a person fails to exercise, often resulting in gaining weight and diminishing heart function, the more difficult effective solutions will be once a person determines to improve their health. If a person continues to "shift the burden" of their own irresponsibility for maintaining or recovering their own health to another, expecting an artificial solution to relieve the burden created by the rejection of the real solution, they will never achieve their goal.
In this case, the harder the patient pushes for solutions from a healthcare system which cannot solve their problem, for which a natural and obvious solution exists, the less benefit the patient will achieve from the healthcare they have sought. It is possible to ignore the real solutions - i.e., activity such as walking - until the knees and other joints have deteriorated and it is not possible to become active. In that case, more and more pressure is placed on the artificial system with less and less satisfaction with the results.
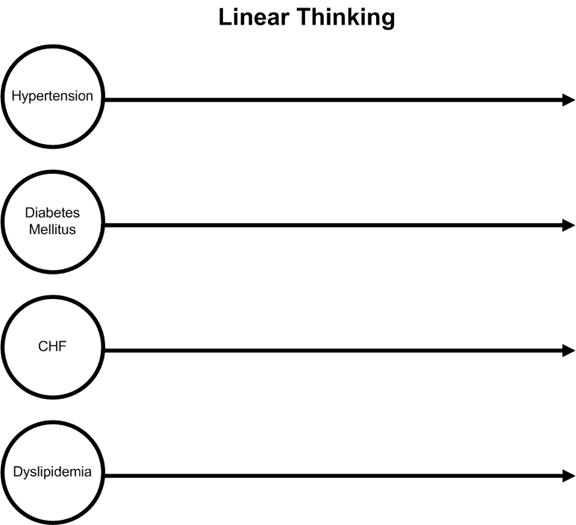
Linear and Circular Causality Thinking
If we are going to change provider and patient behavior so that patient's will realize improved health outcomes, even in the face of decrease cost of care, it will require data display and organization in an EHR which facilitates that change. Schematically, this data organization can be contrasted with "linear thinking." Thinking linearly, a healthcare provider would begin with a disease or problem and focus exclusively on that problem until it was resolved and then go to another problem. Each problem would be dealt with in isolation and without interaction between the two. In biological systems, as in business, nothing occurs in isolation. The following is a simply representation of linear thinking in medicine.
On the other hand, reality in a biological system can only be effectively approached from a circular- causality platform which is designed to encourage and facilitate the dealing with complex, interrelated problem solving for maximal effectiveness. Schematically, this would be represented as follows.
Under Your Life Your Health, numerous articles appear which address this subject including these which appear below:
- Patient Centered Medical Home: The Power of Data in Designing the Future of Healthcare, May 20, 2010.
- Transforming Healthcare: Public Reporting of Provider Performance on Quality Measures December 2, 2009
- SETMA and COGNOS: What is our Goal, November 17, 2009
EHR is a powerful took with which to transform healthcare, but like any took it must be well designed and properly used in order to fulfill its promise.
|