|
Since the emergence of Human Immunodeficiency Virus (HIV) in the late 1970s, a major public health focus has been the identification of individuals who are positive for HIV and to control its spread. The good news is that while, as with any disease, prevention is the best strategy for control of HIV, more and more HIV-positive people are living normal lives with proper treatment. The stereotype is that only homosexuals and drug users can "get" HIV and that they all die quickly. As with all stereotypes, neither is true.
It is unfortunate that early in this epidemic HIV was identified with homosexuality, sexuality promiscuity and illicit drug use by injection. It is unfortunate because screening and surveillance for HIV focused on these groups and most others felt that they did not need to be tested. In a study published in the Journal of Acquired Immune Deficiency Syndromes: (15 April 2010 - Volume 53 - Issue 5 - pp 619-624) entitled, "Undiagnosed HIV Prevalence Among Adults and Adolescents in the United States at the End of 2006," the objective was, "To describe adults/adolescents (age 13 years and older) living with undiagnosed HIV infection in the United States at the end of 2006." The result of this study stated:
"An estimated 1,106,400 adults/adolescents...were living with HIV in the United States at the end of 2006; overall, 21.0%...were undiagnosed. (Caucasians) had the lowest percentage undiagnosed (18.8%) compared with Hispanics/Latinos (21.6%), blacks/African Americans (22.2%), American Indians/Alaska Natives (25.8%), and Asians/Pacific Islanders (29.5%...). Persons with a behavioral risk of injection drug use (IDU) had the lowest percentage undiagnosed (female IDU: 13.7% and male IDU: 14.5%); men exposed through heterosexual contact had the highest (26.7%) followed by men who have sex with men (23.5%)"
The study concluded, "Differences in undiagnosed HIV were evident across demographic and behavior groups. Effective testing programs and early access to treatment and prevention services are necessary to reduce undiagnosed HIV infections and HIV prevalence." This study and others demonstrated the need for surveillance programs which focused on the entire population rather than simply those with high risk behaviors.
A report entitled, Combating HIV and AIDS: Protecting the Health of Latino Communities, stated, "The U.S. HIV epidemic has expanded from one which primarily impacted white gay men in the late 1980's, to an epidemic which, in 2000, affects a more diverse population than ever before. HIV prevention efforts must aggressively target a wide range of communities, from new populations of white gay men, who remain at high risk, to gay men of color, African-American and Latino women at risk, injection drug users of all races, and adolescents as they come of age."
CDC Revised HIV Testing Recommendations in Healthcare Settings September 2006
Effective September 2006, the Center for Disease Control revised its recommendations for HIV testing in healthcare settings. The Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Healthcare Settings aim to make HIV testing a routine part of medical care in addition to expanding the gains made in diagnosing HIV infection among pregnant women. The Recommendations replace CDC's 1993 Recommendations for HIV Testing Services for Inpatients and Outpatients in Acute-Care Settings and they update portions of CDC's 2001 Revised Guidelines for HIV Counseling, Testing, and Referral and Revised Recommendations for HIV Screening of Pregnant Women.
Key differences in the Recommendations for patients in all healthcare settings are:
- HIV screening (another term for broad-based testing) for patients ages 13 to 64 in all healthcare settings after the patient is notified that testing will be performed unless the patient declines (opt-out screening).
- HIV testing of people at high risk for HIV infection at least once a year.
- Screening should be incorporated into the general consent for medical care; separate written consent is not recommended
- Prevention counseling should not be required with HIV diagnostic testing or as part of HIV screening programs in healthcare settings.
Additional key differences in the Recommendationsfor pregnant women in healthcare settings are:
- Including HIV screening in the routine panel of prenatal screening tests for all pregnant women, unless the patient declines (opt-out screening).
- Repeat screening in the third trimester in certain jurisdictions with elevated rates of HIV infection among pregnant women.
The Recommendationsemphasize the importance of voluntary testing. Various constituencies have expressed concern that eliminating the recommendation for separate informed consent for an HIV test could result in some patients being tested for HIV without their knowledge. Others have asserted that requiring separate, written informed consent is a barrier that makes HIV screening difficult to conduct in healthcare settings, and that removing this requirement would make widespread HIV screening feasible.
Why did CDC revise the Recommendations?
There are several compelling reasons why CDC has revised the Recommendations.
- An estimated one-fourth of the approximately 1 million persons in this country who are living with HIV do not know they are infected. That's approximately 250,000 persons who could be spreading HIV to their partners unknowingly. As HIV screening becomes a more routine aspect of medical care, more people will know they are infected with HIV.
- People living with HIV can receive effective treatment, resulting in improved health and extended life, if their HIV infection is diagnosed earlier.
- Currently, many people learn of their HIV infection only after they have developed symptoms (in a large study of HIV-infected persons, 65% reported they were first tested for HIV because of illness).
- Most people, after finding out they have HIV, adopt behaviors that reduce HIV transmission.
- Routine HIV testing may help protect the partners of persons who are living with HIV but do not know it.
- In theory, new sexually transmitted HIV infections could be reduced more than 30% per year if all HIV-infected persons knew of their infection and adopted changes in behavior similar to those of persons already aware of their infection.
Routine HIV testing may reduce the stigma associated with an HIV test offered based on the healthcare provider's perception (or knowledge) of risk. When every person gets offered an HIV test at some point in his or her health care, it should take controversy and judgment out of the test and make it a normal part of taking care of oneself.
Providers reported that requirements for pre-test counseling and written informed consent were not feasible in emergency rooms and other busy healthcare settings.
For whom are the Recommendations intended?
The Recommendationsare intended for healthcare providers in both the public and private sectors. These include healthcare workers in hospital emergency departments, inpatient services (including labor and delivery), correctional health care facilities, clinics including substance abuse treatment, public health, community, pediatric and adolescent, prenatal, and mental health, and other primary care settings. These Recommendationsaddress HIV testing in healthcare settings only. They do not change existing CDC guidelines on HIV counseling, testing, and referral for persons at high risk for HIV who receive testing in nonclinical settings (e.g., at community-based organizations.)
SETMA's Response to the CDC's recommendation
The Texas Department of State Health Services created an HIV/ASTD Prevention and Care Branch which manages a grant program Promoting Annual HIV Screening for ages 13-64. SETMA's first interest in this issue came from meeting with the staff of this program. Immediately, SETMA understood the value of this initiative, but as we proceeded, the application requirements were so complex SETMA decided to do the project without participating in the government funded program.
As a result SETMA has set aside $60,000 to fund the program over the first three months, beginning July 1, 2010. The funding will be for the screening of those patients whose health insurance does not pay for HIV testing.
The biggest question in this project is, "How do you get this done by providers who are already screening numerous diseases, giving extensive preventive care and processing multiple disease management tools at every visit? How will providers remember to do it and how will they have the time to do it? One of the principles of SETMA's deployment of electronic patient records is that we want to make it easier to do "it" right than not to do "it" at all. "It" is excellent healthcare and new initiatives which improve the quality of care the patients we care for receives.
As a result, SETMA took the Pre-visit/Preventing Screening tool which is already completed at every visit on every patient and add HIV screening. The screen shot below from our EMR shows the new screening tool for HIV outlined in red.
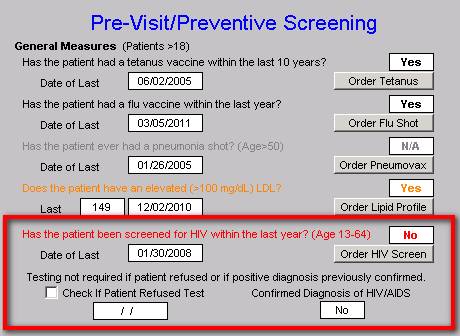
When the provider opens the template, if the patient is between the ages of 13 and 64, and if the patient has not had an HIV screening test in the past year, the screening question will be in red. In that case, all the healthcare provider has to do is to click the "order HIV Screen" button and the following things happen:
- The test is ordered and sent to SETMA's laboratory.
- The test is documented on the patient's chart
- The charge for the test is sent to the patient's insurance company.
- If the company refuses payment, SETMA will pay the charge.
- At the same time, a document is created where the patient can sign for permission for the test to be done.
All of this is done with one click on one button - what could be easier?
As can be seen, the provider or nurse can document two exceptions:
- The patient refuses the test. If the patient refuses the test, a pop-up appears where it is possible to document why the patient refuses.
- The patient has a known HIV positive test in the past.
If the HIV Screening question is "black," it means that the test has been done. If it is "grey," it means that the test does not apply.
Monthly, quarterly and annually, SETMA will report the following internally and to the Texas State Health Department:
- How many patients between 13-64 years of age were seen?
- How many patients were screened for HIV?
- How many patients refused and why?
- How many patients have a prior diagnosis of HIV or HIV/AIDS?
- How many patients were positive for the first time?
At the end of three months and at the end of six months, SETMA will determine the uncompensated cost to the practice of continuing this program. If it is manageable, we will continue it. If it is not, we will contact the major insurance carriers who are declining payment and see if they will change their policy. If we prove that this program is sustainable in a private setting without government, grant or other funding, then we will have performed a significant service to the community.
When your healthcare provider asks you to have an HIV test, say yes for you or for your child. It may save your life or someone else's.
|