 |
James L. Holly, M.D. |
|
 |
|
|
|
|
|
|
|
|
| James L. Holly,M.D. |
| March 13, 2008 |
| Your Life Your Health - The Examiner |
|
Infections, inflammation, infirmity - these words and the conditions they identify have a great deal in common. The problem is that we cannot see "infection" in its early stages and we can not see the inflammation which takes place in the arteries of our body. Yet, infections and inflammation are the most direct causes of the infirmities we associate with aging. And, infections and inflammation are affected by our lifestyle, diet, activity and habits. High calorie, high fat foods contribute to inflammation. Smoking and excessive alcohol contribute to inflammation. Inactivity - a sedentary lifestyle - contributes to inflammation in the body.
When we see the twisted hands of a person with chronic rheumatoid arthritis the reality of inflammation and its affects on the body are real, but we hardly think about the same inflammation which is going on in our bodies unseen but which is unceasingly causing disease. The same dysfunctions of immunity, T-cell abnormalities and immune markers are present in both diseases.
In the Physician's Health Study, 22,000 initially healthy middle-aged men were tracked and they showed that:
- 50% of all people who have heart attacks and strokes do not have hyperlipidemia (high cholesterol)
- 20% of all these events do not have identifiable major risk factors
Surprising? Half of people with heart attacks do not have high cholesterol! This has led to the search for other markers of inflammation within the arteries which would identify those patients at risk for having a heart attack, or markers which themselves are a cause of inflammation.
This search has resulted in the identification of what is now called high-sensitivity C-Reactive Protein (hsCRP) as a strong independent predictor of the risk of myocardial infraction (MI). Equally important is that hsCRP is also a predictor of stroke. The stroke predictive value is important because we know that cholesterol-lowering drugs (statins) lower the risk of stroke. Low-density lipoprotein (LDL - the bad cholesterol) cholesterol is not a very good risk factor for predicting stroke, so unit hs CRP was discovered it was unclear as to why lipid-lowering drugs were effective at decreasing the risk for stroke.
In 2000, the clinical community was interested in lipoprotein(a) and homocysteine as markers and/or cause of risk for heart attacks or strokes. Those did not turn out to be very effective. But along with hsCPR, the following three inflammatory markers - which are not yet being used clinically - have a high value for predicting risk; they are:
- Interleukin (IL)-6 -- a cytokine produced by many different cells including monocytes/macrophages, fibroblasts, endothelial cells, keratinocytes, mast cells, T cells and many tumor cell lines. Elevated IL-6 levels may occur in different conditions including sepsis, autoimmune diseases, lymphomas, AIDS, alcoholic liver disease, tumor development, Alzheimer’s disease, and in c with infections or transplant rejection. Elevated levels of IL-6 may be associated with an increased risk of heart attack, and stroke.
- intracellular adhesion molecule (ICAM)-1
- serum amyloid A
The following table shows the relative risk factors for future cardiovascular disease for eleven inflammatory markers. The eleventh is the risk of the combination of high LDL + high hsCRP. :
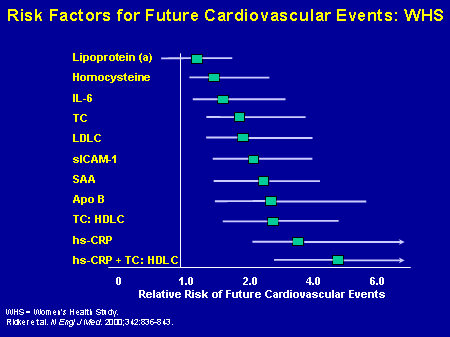
This data comes from Harvard’s Women's Health Study which was a study of a very large group of healthy women. As can be seen the single strongest predictor of future heart disease in otherwise health women was not cholesterol but hsCRP. Yet, the best predictor was the ratio of the total high-density lipoprotein (HDL)/cholesterol plus, and a good inflammatory marker such as the CRP levels
The following levels of hsCRP are now widely accepted as being associated with the following disease risk of future vascular disease:
- less than 1 mg/L -- lower risk
- the 3 mg/L, yellow - average risk
- greater than 3 m/L -- higher risk
In a study published in the Journal of the American Medical Association, it was found that elevated levels of CRP and IL-6 predict the development of type 2 DM. These data support a possible role for inflammation in diabetogenesis
In the January 28, 2003 journal Circulation, the American Heart Association and the Center for Disease Control published their Scientific Statement on "Markers of Inflammation and Cardiovascular Disease: Applications to Clinical and Public Health Practice. They said in part: "Measurement of hs-CRP is an independent marker of risk and my be used at the discretion of the physician as part of global coronary risk assessment in adults without known cardiovascular disease . Weight of evidence favors use particularly among those judged a intermediate risk by global risk assessment."
Clinical Considerations in Anti-inflammatory Therapy
If, therefore, inflammation is the foundation of cardiovascular disease, would anti-inflammatory therapy prevent or mitigate the risk of that disease? When we think about pro-inflammatory pathways, we then have to go back and think about what is driving the CRP and that is generally the Interleukin-6 (IL-6) and Tumor Necrosis Factor Al;pha (TNF-alpha) pathways.
Anti-inflammatory therapy benefit is suggested by the fact that healthy,middle-aged men, who do not have inflammatory conditions but who have low-grade levels of IL-6 are at great risk of future MI. In studies of patients following an MI, those who have high TNF-alpha levels have the highest rate of recurrent cardiovascular events.
This leads back to the question of why statin therapy decreases the risk of strokes but just decreasing the LDL does not decrease strokes. The decrease in strokes with statins (cholesterol lowering drugs) is because they have an anti-inflammatory effect which is summarized in this table:
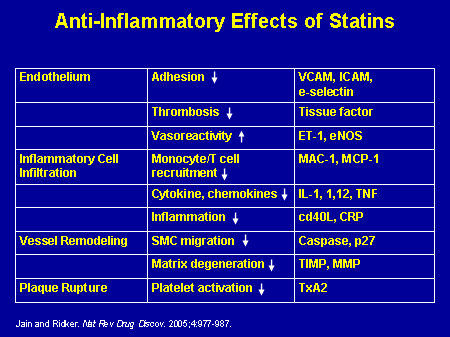
Statins:
- lower LDL and
- lower vascular event rates, but
- they also have a variety of anti-inflammatory effects.
Heart disease, vascular disease and strokes begin with inflammation in the lining of the arteries (endothelium) and progresses to plaque formation and then to plaque rupture. Statins and other anti-inflammatory agents decrease the substances - hsCRP, Interleukin-6, Tumor Necrosis Factor, ICAM-1, etc. - which cause this inflammation.
Clinical Significance of Managing LDL and CRP
This is the standard of care right now for acute cardiovascular medicine; we want to drive the LDL cholesterol below 70 mg/dL because our patients do better in the long term when we do so.
In the PROVE IT-TIMI trial, the CRP levels were measured 30 days after start of therapy and those who got their hsCRP down to less than 2 mg/L also did far better than those who did not. But the question arises, are the patients who reduce hsCRP also the patients who reduce LDL? If they're the same patients, we don't need to measure the CRP. However, it turns out they're largely different patients. We cannot predict the response of statin therapy in terms of the achieved LDL against the achieved CRP, and that means something very important. We also have to think about lowering CRP levels as a way to maximize care.
In the PROVE IT-TIMI study the best outcome was when, LDL was less than 70 and the CRP was less than 2. That survival curve is better than just lowering the LDL and better than lowering just the CRP alone. This was the first time we faced the fact that perhaps this notion of inflammation being managed on a chronic basis was very important to the survival of our patients. However, we need large-scale clinical trial replication before guidelines can get written.
Post MI, the best outcomes occur when both the LDL and the CRP come down, and the worst outcome occurs when only one of these parameters was reduced.
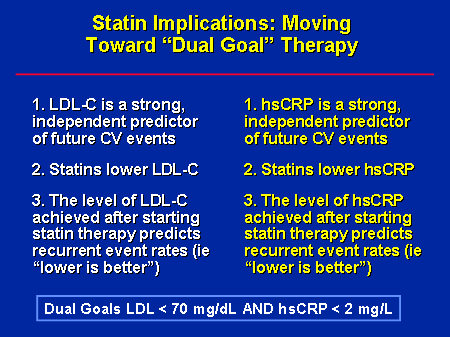
We are beginning to think about dual goals -- the notion of lowering both LDL and CRP for our patients. A very large clinical trial, called JUPITER, is underway to see if we can use the inflammatory biomarker hsCRP to actually prevent heart disease. If half of our patients, having heart attack, stroke, and primary prevention, do not have hypolipidemia, perhaps we can randomize patients who have low levels of cholesterol but high levels of CRP to a statin or the placebo to figure out if we can prevent events.
Potential Effective Therapies
Then why the interest in TNF inhibitors and IL-6 inhibitors; why are we thinking about lowering inflammation to lower vascular risk? In the general population about 10% of patients have extremely low CRP levels. They don't have increased rates of infection. They don't have increased rates of cancer, but they very rarely rupture atherosclerotic plaques, and that observation has been driving this notion that decreasing inflammation can be protective of the heart and of the vessels.
Can targeted anti-inflammatory therapy reduce cardiovascular risk? The following are potential anti-inflammatory therapies::
- Aspirin
- Direct CRP inhibitors
- Traditional anti-inflammatory agents
- IL-6 inhibitors
- TNF inhibitors
What about aspirin? The benefit of being on aspirin was directly related to the lowering of the underlying CRP levels. What about methotrexate? In a nonrandomized study, all-cause mortality and cardiovascular mortality were lower among those whom rheumatoligists chose for whatever reason to give methotrexate to, rather than a different agent. Similar registry data have come out of Sweden looking at anti-TNFs. We have the suggestion that perhaps being on these agents does indeed lower cardiovascular mortality and total mortality.
Finally there's a lot of discussion about whether there is a role, theoretically, for anti-TNF therapy to help with late stent thrombosis and re-stenosis. In the pre-drug-eluting stent era, trials were going on looking at methotrexate and prednisone as methods of preventing in stent re-stenosis and re-thrombosis. More recently, researchers figured out ways of coating the stents with anti-inflammatory drugs and in some ways we have created a new disease and in some ways we have fixed the problem, but the idea of inflammation was very relevant. Last, be aware that within the cardiovascular literature there is now a lot of discussion about directly lowering inflammatory biomarkers—whether CRP is the right biomarker or whether it's another part of the cascade, we don't know.
The future is bright for improving your health with new medicines, but nothing can improve it like losing weight, exercise and stopping smoking (SETMA’s LESS Initiative). Remember, it is your life and it is your health.
|
|
|
|
|
|
|
|
|
|
|