|
The following is a series of question which were presented to SETMA by a national organization about our 14-month pilgrimage to becoming a Patient-Centered Medical Home (PCMH). On the date of this article's publication, SETMA will have submitted an application to the National Committee for Quality Assurance (NCQA) for recognition as a PCMH. In is our hope to obtain a Tier-3 recognition which is the highest.
1. What motivated your organization to become a Patient Centered Medical Home?
In 1997, SETMA realized that we either had to learn the new method of managed healthcare, or be bypassed by a new healthcare delivery model. In spite of initially thinking that managed care was intrusive to the patient/physician relationship, we learned how to practice efficient, cost-effective medicine, while at the same time retaining excellent personal relationships with our patients. In 1998, we adopted the NextGen EMR and EPM products. In May, 1999, only three months after we launched our use of NextGen, we realized that what we needed was "electronic patient management" (EPM, for more on this concept see the EPM section on our website at www.jameslhollymd.com and the articles on EPM under Your Life Your Health) more than electronic patient records. This set us about the designing of disease management tools, doing population management, pursuing quality improvement and integrating all aspects of care delivered at our clinic, hospital, nursing home, physical therapy, hospice, home health, laboratory and other healthcare-delivery functions.
Even as the concept of PCMH became more and more main stream, we were as ignorant of what it meant as we were about managed care thirteen years ago. To show how dynamic this environment is even as PCMH is being accepted, its name is changing into "Health Home," to reflect the expansiveness of the relationship to include many professionals beyond physicians, CNFPs and nurses
After attending a PCMH lecture on February 16, 2009, which lecture was confusing and unhelpful, SETMA decided to take the same approach as we had with managed care. Over a one-month period we did a thorough analysis of our practice based on CMS' 28 principles of PCMH. In that process, we produced a 400-page analysis of our practice in which we identified the things we were doing which reflected the ideals of PCMH and the PCMH functions we were lacking. We then took the 9 Standards, 30 Elements and 183 data points of NCQA's PCMH model and did the same analysis.
By March, 2009, our judgment was that PCMH was a logical extension of what we had been working on for thirteen years. We began thinking and writing about PCMH (all of which is on our website www.jameslhollymd.com) and we published all of our electronic patient management tools on the site as well as publishing our Public Reporting of provider performance on quality measures there. Our early impressions about PCMH grew into a vision and then became a passion. We concluded that this was what we had been working toward all along, even when we didn't know what to call it.
2. What are the three key points of value from becoming a PCMH?
- Creating "intentionality" about quality, excellence, coordination and integration of our patients' healthcare rather than "coincidently" achieving parts of each (For more on this concept see "Medical Home Part IV: Help and Hope in Healthcare" below). In that article, it is stated:
"The most innovative aspect of Medical Home and the thing which
distinguishes it from any other well-organized and highly-functioning
medical organization is the concept of 'Coordination of Care'. This is the intentional structuring, reviewing, facilitating and practicing of a standard
of care which meets all current NCQA, CMS,NQF, PCPI, AQA, and HEDIS requirements for demonstration of excellence in the providing of care.
"The concept of 'intentionality' is critical in this process. This is contrasted
with "incidental." In healthcare, most HEDIS compliance and coordination
of care are done coincidental to a patient encounter as opposed to the having
of a purposeful, provable and persistent method of fulfilling of national
standards of care. Rather than hoping the result is good, 'Coordination of Care' plans and reviews care to make certain that it meets the highest standards.
"The Medical Home intentionally fulfills the highest and best healthcare
needs of all patients. In addition, the patient is involved in this coordination
by our making them aware of the standards and giving them a periodic review,
in writing, of how their care is or is not meeting those standards. Patients are encouraged to know and to initiate the obtaining of preventive care on their
own.
"Perhaps the ultimate judge of the success of Medical Home is when healthcare providers hear the following from their patients, 'I am here today for preventive healthcare.' Today, almost all healthcare providers would tell you that they have never had a patient present with that 'chief complaint,' or reason for scheduling an appointment."
- Team -- The challenge to create a healthcare team with the patient and all healthcare professionals as members of that team. It is the realization that if the one in charge of a patient's healthcare is characterized as the one with the "baton," the patient has the baton for the majority of the time. (For more on this concept see "Passing the Baton: Effective Transitions in healthcare Delivery", March 10, 2010 below). In that article it is stated:
"Athletic metaphors are commonly used in analyzing life situations. Often they are overstated and/or overused, but there is one place where an athletic metaphor is apt in defining a critical point in healthcare. That is in the 'transitions of care' from one venue of care to another. The metaphor is found in track and field relay races.
"No matter how talented the members of a relay team are, the most critical point of their collective performance is in the transition of the race from one runner to another. At this point, one runner, moving as fast as he/she can, must hand the baton to another runner, who has started running as fast as he/she can, before the first runner has even arrived in the "transfer zone." As if this were not complex enough, the rules of the race require that the transfer of the baton must take place within a certain zone.
"If the baton is dropped or if the transfer is not made in the prescribed time, the team, no matter how gifted, will be disqualified and will lose the race. As with life and with healthcare, it is not always the brightest, fastest, or best person who wins. It is the person, in this case, the team, which not only performs well in their individual area of responsibility but who also performs well in transferring the results of his/her performance to the next participant and who does so within the constraints of the rules. Often, it is forgotten that the member of the healthcare delivery team who carries the 'baton' for the majority of the time is the patient and/or the family member who is the principal caregiver. If the 'baton' is not effectively transferred to the patient or caregiver, then the patient's care will suffer."
- It is to discover the true implications of SETMA's motto which we adopted in August, 1995, which states, "Healthcare Where Your Health is the Only Care." It is to put the patient and their needs first. SETMA has done that in many ways. We developed The SETMA Foundation through which we help provide funding for the care of our patients who cannot afford it. In 2009, SETMA's partners gave $500,000 to the foundation We had one patient whose teeth were so rotten that her entire health was deteriorating. The Foundation paid the $10,000 needed to "fix" the problem. It has transformed her life.
Another patient who came to the clinic angry, hostile and bitter was found not to be a bad person but depressed because he could not work, could not afford his medication and was losing his eye sight. He was depressed. He left the clinic with The Foundation buying all of his medications, giving him a gas card to get to our ADA certified DSME program, the fees waived for the classes, help in applying for disability, and an appointment to an experimental program for preserving the eyesight of patients with diabetes. He returned in six weeks with something we could not prescribe. He had hope and joy. By the way, his diabetes was to goal for the first time in years. This is PCMH and it is humanitarianism. They may be the same thing.
3. How has health IT enabled your organization to fulfill the requirements of the PCMH?
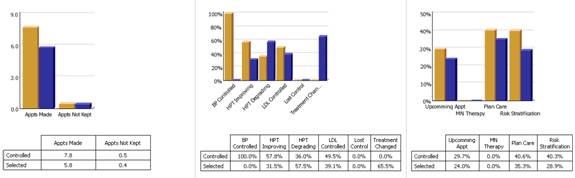
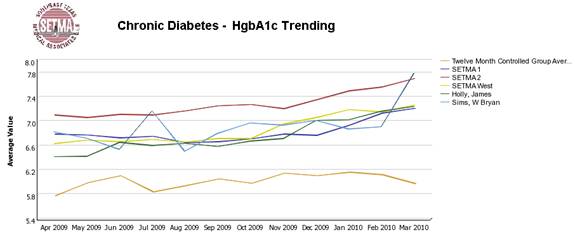
Without IT, SETMA could not address the complex patient-care issues which are required by 21st Century, technological healthcare, not to mention the complex needs of patients with multiple diseases. IT has allowed us to imbed hundreds of quality metrics - both process and outcomes - into our EMR, making it "easier to it right than not to do it at all." We daily and individually track all HEDIS measures on every patient. We participate in PQRI tracking far more quality metrics than those required. We measure Ambulatory Care Quality Alliance (AQA) standards. We track the Physician Consortium for Performance Improvement (PCPI) metrics for diabetes, hypertension , CHF, Chronic Stable Angina, Chronic Renal Diseases, etc. And, where no agency, or organization has endorsed quality measures, such as for Lipids and Chronic Renal Disease State I-III, SETMA wrote our own. We are able to look at patient populations by practice or provider to see longitudinally whether their treatment is to goal and to compare those who are not at goal with those who are. This allows us to see if patterns of care emerge which allow us to improve everyone's care. We are able to look at populations from socio-economic and ethnic perspectives to make sure we have eliminated disparities in care which traditionally afflict these groups.
Without IT, we could not practice the standard of healthcare to which we aspire.
4. How has quality been transformed in your organization and what role has health IT played? For instance, the ability to measure, monitor, trend?
Using digital dashboard technology, SETMA analysis provider and practice performance in order to find patterns which can result in improved outcomes practice wide for an entire population of patients. We analyze patient populations by:
- Provider Panel
- Practice Panel
- Financial Class - payer
- Ethic Group
- Socio-economic groups
We are able to analyze if there are patterns to explain why one population or one patient is not to goal and others are. WE can look at:
- Frequency of visits
- Frequency of testing
- Number of medications
- Change in treatment
- Education or not
- Many other metrics
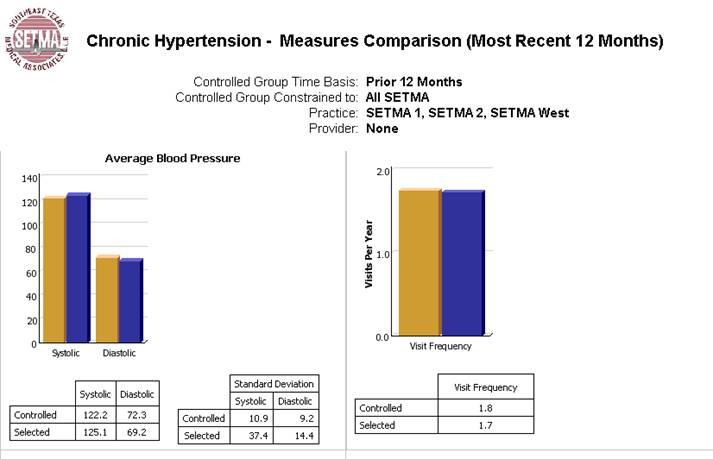
We are able to present over-time patient results comparing:
- Provider to practice
- Provider to provider
- Provider current to provider over time
- Trending of results to see seasonal changes, etc.
5. What are your next steps, and how will health IT factor into your success?
Keep dreaming and moving forward. Change in healthcare is like breathing, it is inevitable and essential. We will add to our auditing ability. We will add functions to our patient care. We will find innovative ways of solving complex problems. We will participate in the transformation of healthcare and healthcare IT, which in ten years will be very much different than it is now. For instance with the human genome detailed and with more and more genetic foundations for disease being discovered, we believe that in ten years or less, it will be necessary to have medical informatics capabilities to store, analysis and to utilize each patient's genome in their treatment. That is a huge data-base task which we are already discussing and designing solutions for. We will all get there one step at a time. At times we will lead the development and at other times we will follow the lead of others. Together, we will change.
6. What tips would you provide to others in preparing for and going through the process?
- Get started! In my life, I have started many things which I never finished, but I have never finished anything I didn't start. No matter how daunting the task, the key to success is to start.
- Compete with yourself, not others! In his book, If Aristotle Ran General Motors, Tom Morris states, ""I do not try to dance better than anyone else. I only try to dance better than myself - Mikhail Baryshnikov." It doesn't matter what someone else is or is not doing; set your goal and pursue it with a passion. Measure your success by your own advancement and not by whether someone else is ahead or behind you. In the same way, share your success with others. In helping others succeed, you will find true fulfillment.
- Don't give up! The key to success is the willingness to fail successfully. Every story of success is filled with times of failure but is also characterized by the relentlessness of starting over again and again and again until you master the task.. When we started our IT project, we told people about what we are doing. We call that our "Cortez Project". Like Cortez, we scuttled our ships so there was no going back. We had to succeed.
- Have fun! Celebrate! Enjoy what you are doing and celebrate where you are. In May of 1999, my co-founding partner of SETMA lamented about our EMR work; he said, "We are not even crawling yet." I said, "You are right but let me ask you a question. 'When your son turned over in bed, d id you shout and say to your wife, "this retard, dimwitted brat can't even crawl, all he can do is turn over in bed?" Or, did you shout to your wife, "He turned over in bed?" Did you celebrate his turning over in bed?" He smiled and I added, "I am going to celebrate that we have begun. If in a year, we aren't doing more, I will join your lamentation, but today I celebrate!" We have had a celebratory spirit since that day and we have gone from success to success.
You may note that none of these tips have to do with process or content but with attitude and "frame-of-mind." These are the elements of success. The process and content are easy.
In addition to the six questions above, if you have any additional materials, guidance and/or knowledge to share, it would certainly be appreciated.
Our website site has an eleven-part series on PCMH. That series reflects our growth and development. Other materials there (under Your Life Your Health) show how we continue to learn and to grow. Under Medical Home at www.jameslhollymd.com we display the tools we have developed and will continue to post new tools that we develop. Under EPM, we display all of our electronic patient management tools. Under Public Reporting, we display our providers' performance on all of the quality measures we are following.
In many ways, SETMA has only begun, but wherever we are, we are celebrating, having fun and desiring to help others succeed.
|