|
The following is NCQA’s explanation of their “New Distinction in Patient Experience Reporting.”

NCQA developed the optional Distinction in Patient Experience Reporting to help practices capture patient and family feedback through the newly developed Consumer Assessment of Healthcare Providers and Systems (CAHPS) Patient-Centered Medical Home (PCMH) Survey. Because consumer experience is a critical component of quality of care, giving more prominence to patient engagement is a crucial change to the PCMH program. The CAHPS PCMH Survey assesses several domains of care:
- Access
- Information
- Communication
- Coordination of care
- Comprehensiveness
- Self-management support and shared decision making.
NCQA PCMH-Recognized practices may use the CAHPS PCMH survey to obtain the distinction. Practices without recognition may still submit CAHPS PCMH results, but may earn distinction only after achieving NCQA PCMH Recognition. Submitted data will be used to develop a benchmarking database that will allow comparison across practices. In addition to earning distinction and being listed in directories as having distinction, practices will receive credit in PCMH 2011.
The program details include:
- Practices must use an NCQA certified vendor to ensure a standardized method of data collection and reporting. Click here for a list of trained and certified 2014 CAHPS PCMH survey vendors.
- NCQA-Recognized practices, or practices applying for recognition, are eligible for the distinction. All practices may submit data, but may not be eligible for the distinction. CAHPS PCMH Distinction Frequently Asked Questions for practices document is NOW available. Click here to access the FAQs.
- There are two data submission periods per year: the first is in April; the second in September.
- The distinction is effective for one year after NCQA receives the practice's data. Practices must submit data annually (through the vendor) to maintain distinction. Practices have the option of submitting data during both data submission periods, but it is not required.
As a practice makes the transformation from traditional healthcare to patient-centered medical home, new tools are needed for measuring the effectiveness of the changes. New concepts such as “shared decision making” between patient and provider new measurement. In the old healthcare system best practices depended upon “patient satisfaction surveys” to measure quality. That system of care was based upon volume of work done. On the PC-MH model of care, focus on volume has been replaced with the value of the healthcare which is being delivered and patient satisfaction is being replaced with the concept of “patient-centeredness” of care.
“Patient-centeredness” includes concepts such as patient activation and patient engagement. Details of these concepts can be found at: SETMA.com | Medical Home | Teaching Tool for PC-MH Course - Patient Care Activation, Engagement, Shared-Decision Making --http://jameslhollymd.com/medical-home/teaching-tool-for-pc-mh-course. Essentially, it means that a patient is prepared to lead their healthcare throughout the year. It means that the majority of time, patients are in charge of their own healthcare. This is illustrated by the fact that if a patient is receiving a great deal of healthcare, he or she will be in the provider’s present 8-20 hours a year. In that there are 8,760 hours in the year, this means that the patient is in charge of their own care 8,740 to 8,752 hours a year. If the patient is not prepared to guide their own care, all efforts to maintain excellent care and/or treatment will fail.
Essentially, the medical home model means that you are no longer a passive recipient of healthcare instructions from a healthcare provider, but you are now an active participant in your own care. Viewed as a “race,” your health-care is yours to run. Viewed as a “baton” in a relay race, you will carry your baton for the majority of your life. With 8760 hours in a year, and with your formal healthcare received from a healthcare provider occupying fewer than twenty hours a week, you are in charge of your care for over 8740 hours a year.
SETMA being a medical home means that your care will be “coordinated”, i.e., you will know where, when and how to obtain the care you and your provider have determined that you require. It means that you will receive a plan of care which is more than a prescription and a follow-up visit. It means that in a process called “shared-decision making,” you and your SETMA provider agree upon comprehensive steps to retain or regain your health. It means that because active learning is the only effective way for you to participate in your own healthcare decision making, your “activation” occurs when you gain the knowledge and skills needed. This is called “activation,” after which you become “engaged” in your care.
The foundation of this new dynamic is the patient-centric conversation in which you and your provider discuss your healthcare concerns and needs in a dialogue which is an active process rather than the traditional monologue where you passively received information and instructions. Under the old model of care, which might be referred to as a “paternalistic” healthcare system, you were very often told what to do and it was expected that you would follow the healthcare providers’ instructions without modification.
“Paternalism” meant “treating you in a fatherly manner, especially by providing for your needs without giving you rights or responsibilities.” The medical home redefines your relationship with your provider and changes how you relate! Rather than healthcare encounters being didactic (to lecture or teach, as one with knowledge instructions or informs), where the healthcare provider tells you what to do, how to do it and when to do it, the patient-centric encounter becomes a dialogue (an exchange of ideas or opinions) - where you and your provider discuss mutual concerns and together come to a conclusion with a mutually agreed upon plan. This new relationship is somewhat like a partnership.
The concept of a patient encounter being a dialogue where your interests and desires are respected is alien to the old paternalistic model of care. The only way in which the patient-centric conversation in a healthcare encounter can be a dialogue is where you and your provider become collegial and where you both enter into a collaborative relationship.
In Your Life Your Health, January 1, 2014, SETMA’s performance on CAHPS for October-November, 2013 was reported. That report can be reviewed at:
http://jameslhollymd.com/Your-Life-Your-Health/ncqas-new-distinction-in-patient-experience-reporting. Now we report on SETMA’s CAHPS for January-March, 2014.
SETMA uses the data listed below to review our patients’ perception of the care they are receiving in order to find ways in which we can improve that care. And, On April 17th, we will have the first SETMA Community Council meeting. Made up of patients, providers, citizens and other, the Council will be introduced to the structures and practices of SETMA. The Council will be asked to give their opinions of how effectively we are meeting our goals of meeting the needs of our patients and they will be asked to suggest ways in which we can improve our care.
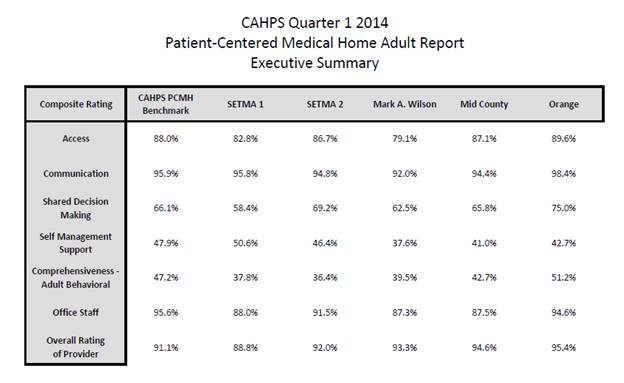
The first table is an Executive Summary of seven categories with the aggregate total result.
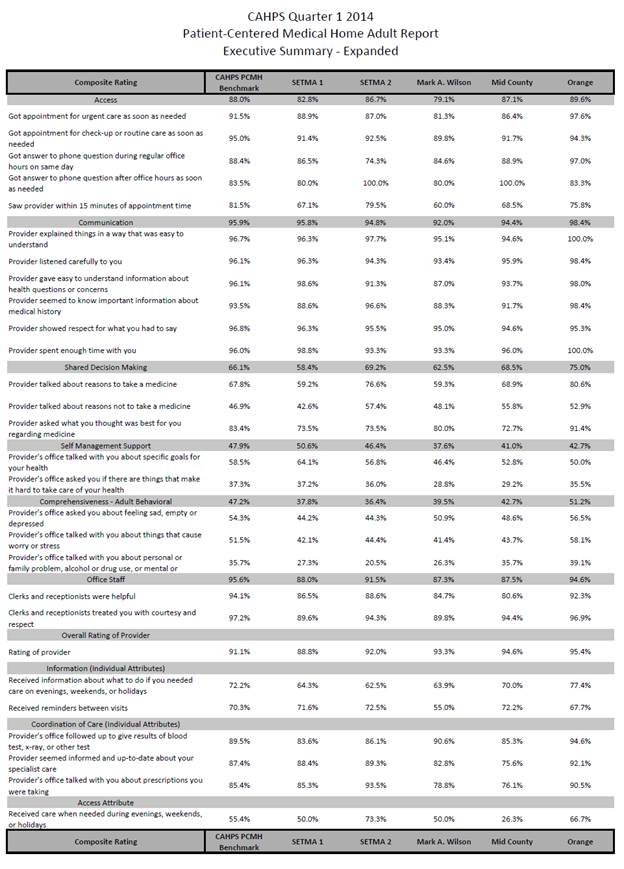
The larger table seen below gives more detail about each category of SETMA providers’ performance.
|