|
Athletic metaphors are commonly used in analyzing life situations. Often they are overstated and/or overused but there is one place where an athletic metaphor is apt in defining a critical point in healthcare: that is in the transitions of care from one venue of care to another. The metaphor is found in track and field relay races.
No matter how talented the members of a relay team are, the most critical point of their collective performance is in the transition from one runner to another. At this point, one runner, moving as fast as he/she can, must hand the baton to another runner, who has started running as fast as he/she can, before the first runner has even arrived in the "transfer zone." As if this were not complex enough, the rules of the race require that the transfer of the baton must take place within a certain zone.
If the baton is dropped or if the transfer is not made in the prescribed time, the team, no matter how gifted will be disqualified and will lose the race. As with life and with healthcare, it is not always the brightest, fastest, best person who wins. It is the person, in this case, the team, which not only performs well in their individual area of responsibility but who also performs well in transferring the results of his/her performance to the next participant and who does so within the constraints of the rules. Often, it is forgotten that the member of the healthcare delivery team who carries the "baton" for the majority of the time is the patient and/or the family member who is the principal caregiver. If the "baton" is not effectively transferred to the patient or caregiver, then the patient's care will suffer.
In healthcare there are transition points-of-care, where the "baton", which now represents the transfer-of-care responsibility from one person to another, must be smoothly, efficiently and timely accomplished, or the value of the care provided by each care giver will be diminished to the point that the overall quality of care may be less than the sum of the contributions of each care giver. This diminishing of the value of care occurs when only a small part of the value of each participant's contribution is successfully transferred to the next point-of-care. This occurs when the "baton" is dropped.
These transfer points or interfaces of care are:
- From the healthcare provider to the patient in the clinic setting.
- From the emergency department to the inpatient setting.
- From the inpatient setting to the patient or family at home.
- From the inpatient setting to the rehabilitation unit or the nursing home.
- From one provider to another provider.
Integrated - Coordinated - Continuous
It may be that within each patient encounter, the level of care is "fairly good." When a patient is seen by a family physician, internist, or nurse practitioner, the quality of the visit as measured by the content is good. The same is the case with procedures, labs, specialty referrals, and other points of care. The deficiencies seem to come at the transition points, or at the interface of care, i.e., when the patient is leaving the clinic, emergency department, inpatient hospital, or other point of care and moving into another sphere of care.
The most common transition of care for a patient is the moving into the sphere of personal care, family care, home care or however you wish to define, describe or denote that the patient is "going home." Often instructions, training or understanding is inadequate or absent in these transitions. Whether the interface is between the inpatient/home, clinic/home, laboratory/home, procedure/home, specialist/home or a number of others, the patient's vulnerability and the decreasing of the quality of their care most often happens at these points.
Southeast Texas Medical Associates (SETMA) has attempted to create methods for improving these transitions (interfaces) with the following tools. Each tool can be seen as a "baton" which must be successfully grasped by one provider and passed on to another in order for the content and value of one provider's work to be available to another. Remember, in the list of the providers of healthcare, the one who spends more time giving healthcare to a particular patient is the patient himself or herself. The "batons" or the "transition tools" designed and employed by SETMA and the transition points are:
- Patient attends clinic
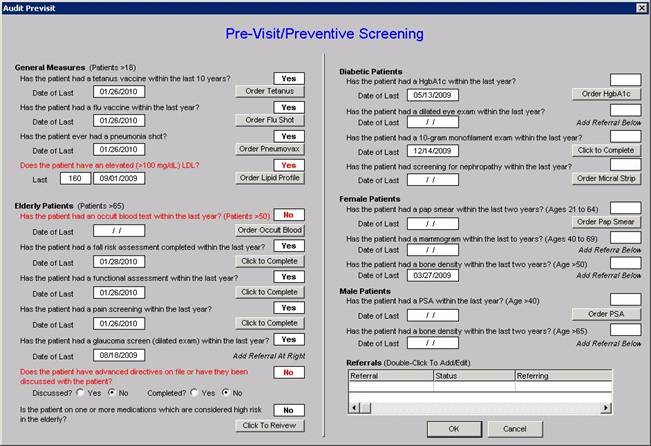
- A "previsit preventive care and screening care audit" - this audit is performed on the patient via SETMA's COGNOS Project (for more information on this project see www.jameslhollymd.com under "Public Reporting") before the visit, empowering the healthcare team to fulfill all elements of preventive care and screening care immediately and easily. The same audit function is also displayed in SETMA's EMR. It is the first thing nurses and healthcares providers review at the beginning of a visit.
The following is the template which automatically tracks the status of these issues in the patient care. On this template, everything is black applies to the patient and has been completed. Everything in grey does not apply to the patient. Everything in red applies to the patient and has not been done. If a needed intervention has not been done, the clicking of the "order" button, orders the test, posts it to the patient's chart, sends it to the nurse, lab, etc and documents that it has been done. This fulfills SETMA's EMR design which requires that we "make it easier to do it right than not to do it at all."
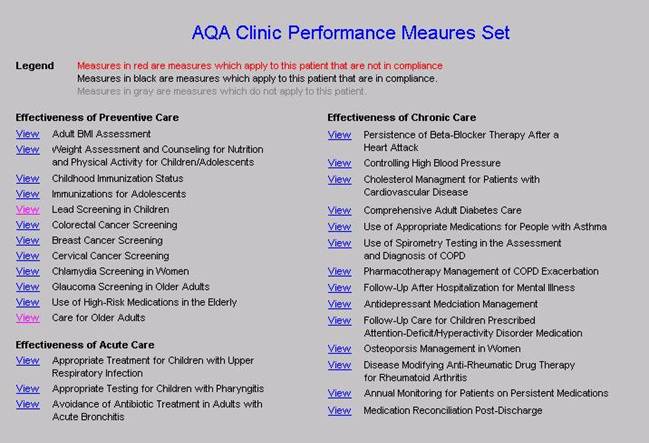
- The "ambulatory care quality measurement set" -- endorsed by the Ambulatory Care Quality Alliance (AQA), the AQA Measurement Set is reviewed by every nurse and every provider at every visit. The legend is the same as for the above template.
- "Coordination of Care Review" - This "baton" is a document which summaries the status of a patient's care. It includes identification of care givers with contact information, medical power of attorney, emergency care instructions if an evacuation is called, code status, evaluation of barriers of care, readiness to change evaluations, patient instructions for end-of-life management, and the status of multiple quality measures standards including HEDIS, AQA, NQF, PCPI, and PQRI.
This "baton" is a Coordination-of-Care-Review document which given to the patient with instructions:
"Please review this document. Identify the information which is missing from your chart, such as power-of-attorney, etc. Please bring that with you to your next visit, e-mail your provider with the information or call your health care provider and give them this information. Also, please review the quality measures listed. If any apply to you and are NOT completed, please ask your provider to address these issues the next time you come to the office."
- Plan of Care and Treatment Plan -- The patient is seen. All acute problems or complaints are dealt with and all chronic disease conditions are addressed such as diabetes, hypertension, dyslipidemia, chronic renal disease, CHF, asthma, cardiometabolic risk syndrome, chronic stable angina, etc.
It is here that a major interface occurs and where the baton is often dropped. As a result, SETMA has designed disease management "plans of care' and "treatment plans" which are created easily through the use of disease-management programs which aggregate treatment standards, goals, status, treatments and planned interventions.
These tools include personalized, written recommendations to patients and often include appointments to care coordinators and SETMA's education department. These evaluations always included extensive "risk stratification" which allows the provider to recommend precise, evidenced-based treatment to the patient.
NOTE: SETMA has placed printers in every examination room to make the preparing of personalized healthcare information for each patient easy to produce and to give to the patient.
- Follow-up telephone calls - SETMA does not think that every patient seen in the clinic will benefit significantly from a follow-up contact via telephone but for those who are vulnerable, at risk, fragile or alone, each provider can schedule a nurse follow-up call via a follow-up telephone-call function built into our EMR. Nurses. who work full-time only contacting patients, will make the call when the provider designates (1 day; 3 days, 1 week; 1 month, any interval noted). The result of the call will be communicated back to the provider and further follow-up contact or intervention can be recommended.
The timing of these calls is done via an "electronic tickler file." Also, home visits can be scheduled by the provider for safety evaluation, skilled nursing needs, or other concerns. These are done through our EMR Referral template.
- Laboratory, procedure and other reports - via a template entitled "Provider Response to lab Results" the provider is able to give a precise evaluation to the patient concerning the results of their laboratory results.
- Telephone Inquiry Response - via a "Telephone Inquiry template" every telephone contact is responded to via provider generate instruction. The standard is "every call from every patient answered every day."
- Medication Reconciliation - another major interface is between the medication the patient has been prescribed, the medication the provider thinks the patient is taking and the medication the patient is actually taking. At every clinic visit, a medication reconciliation is completed and an accurate, personalized medication lists is given to the patient with the date of the visit on the list.
- Patient is in the hospital
It must be remembered that when a patient leaves the hospital, until they are seen in the office or home, the provider team member who is in charge of the patient's care is the patient or a family member. Therefore the baton must be successfully passed to the patient, if the coordination, integration and continuity of care is to be maintained.
- The patient-care interface with the hospital is seamless because SETMA uses the EMR in the hospital for Admission History and Physical and Discharge summaries.
When the patient leaves the hospital they are given "hospital follow-up instructions" which includes an accurate, reconciled medical list, follow-up instructions with appointments and follow-up procedures, tests, etc., already made. Any tests results not reported at the time of discharge are noted and are automatically follow-up on two days later.
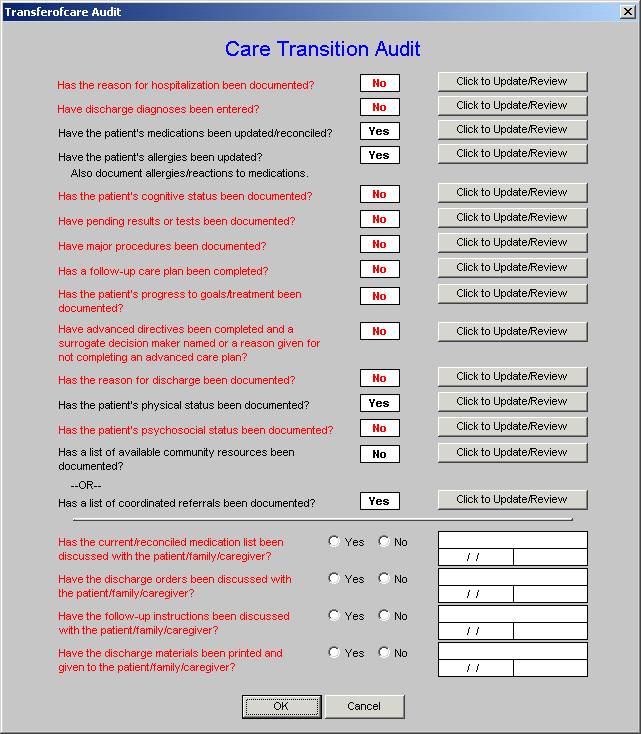
- Care Transition - in June, 2009 the AMA released the "PCPI Care Transitions measurement set". Due to SETMA's having used the EMR for discharge summaries for ten years, it was apparent that with very slight modification, we were fulfilling all of these measures. We implemented this measurement set and are performing at 100%.
As can be seen by reviewing the 14 data points and the 4 actions required by the audit, when the elements of this audit are met and when the discharge summary and follow-up document are completed with this material and are given to the patient and/or family, almost all of the continuity of care issues are resolved. The legend is that everything in black is done and everything in red has not been done. For the elements which have not been done, the "Click to updateReview" button takes the provider back to the place in the Discharge Summary where the data point at issue should be documented.
This transition audit is one of the tools used to "build" the "baton" and then to make sure that the complete "baton" has been transferred to the next team member.
- Medication Reconciliation - it is imperative that careful medication reconciliation takes place at the end of any and every hospitalization and that a copy of the appropriate list of medications is given to the patient/family. In that SETMA completes the discharge summary in the EMR, the hospital medication reconciliation is automatically a part of the patient's outpatient record. Nevertheless, when the patient comes back to the office, a medication reconciliation is repeated each time.
- Telephone follow-up - Every patient discharged from the emergency department or inpatient status receives a telephone call the day following their discharges. Subsequent calls can be scheduled as indicated. The follow-up call addresses current condition, medications, reactions, special needs and follow-up appointments.
Since SETMA began this five months ago, it has increased patient satisfaction, patient safety and the quality of patient care. It is early yet, but we believe it will decrease our readmission rate which is already very low.
There are other transitions and/or interfaces for which SETMA has designed equally robust solutions such as inpatient to nursing home, nursing home to home, inpatient to hospice, inpatient to home heath, etc. As healthcare continues to be transformed, the "passing of the baton" will increasingly be improved. (All of these "batons" are described and explained on SETMA's website at www.jameslhollymd.com)
|