|
From multiple perspectives, attention continues to be focused upon preventable readmissions to the hospital within thirty days of discharge. Often, it is assumed that these readmissions are a systems failure related to effectiveness of care, care transitions, coordination of care, medication reconciliation, barriers to care, patient support, or other preventable causes.
The driving forces behind the goal to decrease readmission are multiple and include:
- Patient safety
- Quality of care
- Improvement of outcomes
- Cost of care.
Strategies for Preventing Readmissions
The American Hospital Association (AHA) identified thirteen strategies which have been analyzed for their benefit in preventing hospital readmission rates.
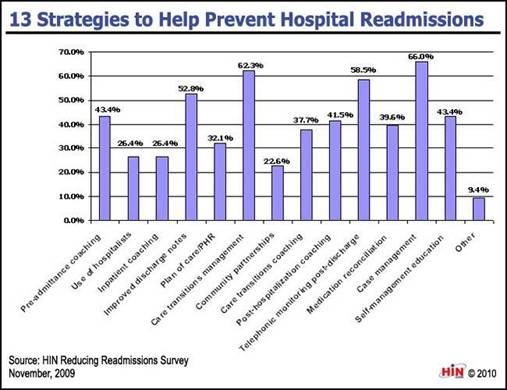
The four most effective according to this report are: improved discharge notes, care transitions management, telephonic monitoring post-discharge, and case management. Remarkably, these are the four major emphasis of SEMTA’s program.
All Readmissions are not preventable
Another study addressed the realities of readmissions:
“Critical to the analysis of readmissions is appropriateness. Some readmissions may be unavoidable. Other readmissions may be avoidable, but nevertheless occur, due to a lack of follow-up care coordination or some other problem. Obtaining a readmissions rate of zero is not feasible and may even indicate poor quality care, as many readmissions are medically appropriate due to an unavoidable change in condition or a new condition. For example, physicians may provide patient-centered care by discussing early discharge with patients, with the mutual understanding that readmission may be necessary.
“On the other hand, behavioral choices, such as non-compliance with dietary recommendations, may also trigger an avoidable readmission despite proper outpatient care coordination. Other readmissions may occur as a result of a medical error or adverse event that occurred during the initial hospitalization or as a result of a lack of social support, follow-up care, understanding of discharge instructions, or communication following discharge. These avoidable readmissions that occur as a result of a breakdown along the care continuum were the focus of meeting discussion and of this brief.”
Key to the entire question of readmissions is patient safety and patient health. While decreasing preventable readmissions will contribute to the both, an artificial of decreasing readmissions by simply refusing to admit a patient whose condition requires it, is not the solution.
Surviving a Hospital Stay and decreasing Readmissions
Actually, it is possible to avoid all readmissions, theoretically, but the method is unacceptable. How? You simply keep patients in the hospital until they are totally well, or until they succumb to their illness. This is obviously ludicrous but it does establish one extreme of this analysis. The principal absurdity of this idea is that the hospital setting itself is unhealthy. In a previous Your Life Your Health article, we described three ways of surviving a hospital stay: “eat up” (maintain proper nutrition, as malnutrition aggravates all chronic conditions), “get up” (maintain activity and mobility, as inactivity and immobility are at the basis of most chronic illnesses), and “get out”: (have as the principal goal, getting out of the hospital as quickly as possible).
SETMA’s Program to Decrease Hospital Readmissions
SETMA began focusing on readmission rates in 2009 when we first began an aggressive program for improving Care Transitions and using Business Intelligence software to analyze potential leverage points for decreasing readmissions.
As an NCQA Tier III Patient-Centered Medical Home and an AAAHC (Accreditation Association for Ambulatory Health Care) accredited Medical Home and accredited Ambulatory Care Practice, Care Coordination and Care Transitions are a critical part of what SETMA does. To our previous efforts to decrease readmissions, we are now paying special attention to patients at high risk of readmissions.
We have added a new function to our Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan (This is the new name for what was previously called the “Discharge Summary). Part of the discharge planning for SETMA’s patients is now the determination as to whether the patient is a high risk for readmissions. The below shows where this is documented on the Hospital Care Summary:
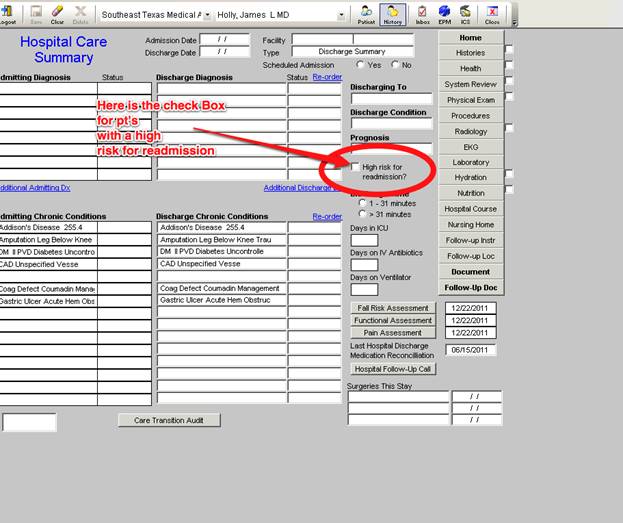
When a person is identified as a high risk for readmissions, SETMA’s Department of Care Coordination is alerted. The following ten steps are then instituted:
- Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan is giver to patient, care giver or family member.
- The post hospital, care coaching call, which is done the day after discharge, goes to the top of the queue for the call - made the day after discharge by SETMA’s Care Coordination Department. It is a 12-30 minute call.
- Medication reconciliation is done at the time of discharge, is repeated in the care coordination call the day after discharge and is repeated at the follow-up visit in the clinic.
- MSW makes a home visit for need evaluation, including barriers and social needs for those who are socially isolated.
- A clinic follow-up visit within three days for those at high risk for readmission.
- A second care coordination call in four days.
- Plan of care and treatment plan discussed with patient, family and/or care giver at EVERY visit and a written copy with the patient’s reconciled medication list, follow-up instructions, state of health, and how to access further care needs.
- MSW documents barriers to care and care coordination department designs a solution for each.
- The patient’s end of life choices and code status are discussed and when appropriate hospice is recommended.
- Referral to disease management is done when appropriate along with tetehealth monitoring measures.
This addition to our hospital readmissions program is the result of the analytics which we have been performing for the past 30 months. We have discovered that there are two major leverage points were the risk of readmission s can be reduced:
- Did the patient receive a post-hospital care coaching call the day after discharge?
- Did the patient have a follow-up visit with their personal physician within six days of discharge?
If these two steps were taken, the risk of readmission is decreased by 22%. As can be seen by comparing the 13 strategies for decreasing readmissions identified by the AHA, SETMA’s plan recognizes that tradition healthcare will not solve this problem. New and innovative styles and types of care are going to be required to solve this problem.
Other metrics continue to be evaluated for potential in reducing readmissions. They are:
- Age
- Gender
- Ethnicity
- Socioeconomic Status
- Morbidities
- Co-morbidities
- Length of Stay
- And others
Some of these metrics are unchangeable which means that their contribution to the risk of readmission is not solvable but lets us know how complex this problem is.
Predictive Modeling and Changes in Care Management
Currently, SETMA’s determination of whether patients are high risk for readmissions is intuitively determined, i.e., at discharged based on experience and judgment, a patient is designated as potentially high risk for readmission. SETMA is designing a “predictive model” for identifying patients at high risk for readmissions and instituting the above plan for interdicting a readmission. This is an attempt to quantify the most effective opportunities for decreasing preventable readmissions.
There is a significant body of science associated with “predictive modeling.” It is clear that tradition models of care delivery will not “work” in a sustainable program for decreasing readmissions. Traditional disease management will not result in changing the patterns of care. In a January/February, 2012 Professional Care Management Journal article, the following abstract addressed changes needed to affect a decrease in preventable readmissions:
“Purpose/Objectives: The move to the Accountable Care Organization model of care calls for broad-sweeping structural, operational, and cultural changes in our health care systems. The use of predictive modeling as part of the discharge process is used as a way to highlight just one of the common processes that will need to be transformed to maximize reimbursement under the Accountable Care Organization model. The purpose of this article is to summarize what has been learned about predictive modeling from the population health management industry perspective, to discuss how that knowledge might be applied to discharge planning in the Accountable Care Organization model of patient care, and then to outline how the Accountable Care Organization environment presents various challenges, opportunities, and implications for the case management role.
“Findings/Conclusions: The development of predictive models to identify patients at risk for readmission is described and how such models can positively impact the discharge planning process by lowering readmission rates. Examples of the structural, operational, cultural, and case management role changes necessary to maximize the benefits of an Accountable Care Organization are described.
“Implications for Case Management Practice: There is a growing need for advanced practice nurses to fill the leadership, resource management, analytical, informatics-based, and organizational development roles that are sorely needed to advance the Accountable Care Organization model of care. Case managers are well-positioned to lend their expertise to the development efforts, but they will need to be educationally prepared for the many advanced practice roles that will emerge as our nation evolves this new system of health care delivery.”
SETMA has recognized the unique skills of nurse practitioners (NPs) for improving healthcare. Rather than viewing NPs as competitors, SETMA seems them as collaborators who help us all deliver better healthcare. The NPs who are trained at the doctoral level are particularly prepared to help in the restricting healthcare delivery to solve the problems associated with preventable readmissions.
SETMA’s Predictive Modeling Goal
Our goal is to continue to identify leverage points which will facilitate the reduction of 30-day, preventable readmissions. This will include new structures to healthcare delivery with the increased utilization of the special skills of nurse practitioners, care coordinators, social workers and others. The elements which we are examining this Predictive Modeling is that the patient:
- Has been readmitted in the past twelve months
- Has inadequate social support, I.e., lives alone, sick spouse,
- Has issues of independence with activities of daily living.
- Has inadequate resources.
- Has mental impairment.
- Has any of the following chronic conditions:
- COPD
- CHF
- Crohns Disease
- Asthma
- MI
- CABG
- Respiratory Failure
- CVA
- Post-op complication
- Multiple bed sores
- In hospital more than 7 days
- Discharged in Observation
- ESRD
- Nursing Home Patients - SETMA plans to update our plan of care for nursing home residents to includes letter to the administrator and director of nursing for strategies to not send patient back to hospital - medication reconciliation)
- Failure to thrive
- Malnutrition
- Unrealistic family expectations
- Feeding tube
- Drain
- Wound care
- Impaired Mobility
- Refused custodial care when it was recommended
- Refused Hospice when it was appropriate
- No code status
While an effective predictive modeling tool will help us identify patients in need of special attention, the modeling does not necessarily identify what care changes will effectively intervene in that risk. The complexity of preventable readmissions will require creative, innovative, systems wide and team-based changes in care delivery.
|