|
In 2002, SETMA began a relationship with Diabetes Center of Excellence in Boston, Massachusetts, which is affiliated with Harvard Medical School and in 2010 formalized this relationship as a Diabetes Center of Excellence. Prior to this relationship and particularly following its beginning, SETMA realized that in a multi-specialty setting it is not enough to have an excellent diabetes treatment program; it is important to have an excellent diabetes prevention program which includes a diabetes screening program.
In preventing diabetes, it is important for all of SEMTA’s patients to know how type II diabetes develops. The sequence of events is depicted below:
Insulin Resistance
The first step in the development of diabetes is the development of “insulin resistance,.” where your body, particularly muscles and liver, do not respond to insulin the way they should Normally, insulin signals the muscles to absorb sugar so that it can be used as an energy supply and insulin signals the liver to stop making sugar in a process referred to as gluconeogenesis (the making of new glucose or sugar). There are four known conditions which make a person at higher risk for insulin resistance. They are: genetics, aging, obesity and inactivity.
Anyone can develop diabetes, but most people who do, have a genetic predisposition to diabetes. That means that there will be some close family member who had or who has diabetes, particularly a parent or a sibling. It is important to remember, however, that a genetic predisposition does not mean that you will inevitably develop diabetes. It only means that you have a higher likelihood than someone with no genetic link to diabetes. With proper diet and activity, you will not develop diabetes.
Screening for Insulin Resistance
Insulin is produced by the pancreas. It is needed by the body to regulate, along with other substances, the blood sugar level of the body. Insulin principally works by moving blood sugar into the liver and into muscles. Insulin also "signals" the liver to stop making sugar (glucose) out of the protein and carbohydrates you have eaten. In a number of circumstances, the liver and muscles do not respond to insulin. This is called "insulin resistance," and is the precursor to type 2 diabetes. When the body does not respond to insulin properly, the body assumes that more insulin is needed creating a condition referred to as “hyperinsulinism,” which simply means more insulin is made than should be needed.
SETMA providers can evaluate your risk of insulin resistance. The following template does that.
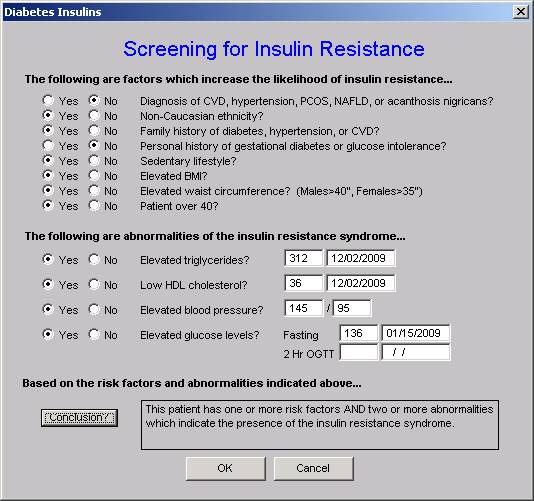
The elements of the “Screening for Insulin Resistance” template are automatically populated, allowing your SETMA healthcare provider to click the “Conclusion” button to determine whether, or not you are at a higher risk of insulin resistance. In addition, SETMA providers calculate several numerical scores which indicate the presence of insulin resistance; they are:
- HDL/Triglyceride ratio -- if this ratio is above 2, it is indicative of insulin resistance. Your SETMA provider can give you your results whenever your cholesterol is checked.
- Cardiometabolic Risk Syndrome -- Previously referred to as Syndrome X, Insulin Resistance Syndrome, or Metabolic Syndrome, the presence of the Cardiometabolic Risk Syndrome is indicative of the presence of insulin resistance. Your SETMA provider routinely assesses the presence of this condition with three different diagnostic criteria published by the World Health Organization, the ATP-III (Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) and by the International Diabetes Federation.
- HOMA-IR (Homeostasis Model Assessment of Insulin Resistance) -- this score is normally used in research programs, and is based on an equation calculated with a fasting insulin level and a fasting blood sugar. When the HOMA-IR is above 2, it is indicative of the presence of insulin resistance.
- Fasting Insulin Level -- when elevated insulin is present in the fasting state, it is suggestive of insulin resistance which results in increased insulin levels to compensate for the liver and muscles decreased response to insulin. Your fasting insulin level should be below 10 uUnits/ml. Higher than that suggests hyperinsulinism due to insulin resistance.
- Hemoglobin A1c €“ this is a test which measures the amount of glucose (sugar) which is attached in an abnormal way to your red blood cells. The value is expressed as a “%.” The following table shows the relationship between the HbA1c and the ‘estimated average glucose (sugar).”
| HbA1c (%) | eAG |
| 12 | 298 (240-347) |
| 11 | 269 (217-214) |
| 10 | 240 (193-282) |
| 9 | 212 (170-249) |
| 8 | 183 (147-217) |
| 7 | 154 (123-185) |
| 6 | 126 (100-152) |
| 5 | 97 (76-120) |
| 4 | 68 (51-86) |
If your HbA1c is below 6.5% and above 6.0% you are said to have pre-diabetes and active steps must be taken to avoid the development of full-blown diabetes. If your HbA1c on two different occasions is above 6.5%, you have diabetes.
If you have insulin resistance and do not yet have diabetes, you MUST take steps to lose weight, exercise, stop smoking, reduce stress, and get proper sleep in order to delay or avoid diabetes.
Reversing Insulin Resistance and preventing diabetes
Of the four contributors to the development of insulin resistance, two are unchangeable: genetics and age. The other two €“ obesity and inactivity €“ are related to lifestyle choices.
These are addressed in SETMA’s LESS Initiative which encourages you to lose weight and to exercise.
The results of the Diabetes Prevention Program Work Group, published in the New England Journal of Medicine (N Engl J Med 2002; 346:393-403February 7, 2002), showed that the diabetes drug metformin reduced the risk of diabetes in those with pre-diabetes but was much less successful than losing weight and increasing activity. At present, no drug has been approved by the Food and Drug Administration (FDA) specifically for insulin resistance or pre-diabetes.
In a May 5, 2010 report to the United States Senate Subcommittee on Labor in support of a request for 2011 Education Appropriations, the following was stated:
"For type 2 diabetes, prevention appears to be the name of the game. This form can be averted or delayed by lifestyle factors. The NIH-funded Diabetes Prevention Program (DPP) trial showed that one the most effective ways to lower the risk of type 2 diabetes is through regular exercise and modest weight loss. There is good reason to believe that such efforts may lead to a lifetime of health benefits. A recent follow-up study of DPP participants found the protective effects of weight loss and exercise persist for at least a decade.”
Scientists established the following numbers to help people set goals that will reduce their risk of developing glucose metabolism problems, i.e., diabetes:.
- Weight. Body mass index (BMI) is a measure used to evaluate body weight relative to height. You can use BMI to find out whether you are underweight, normal weight, overweight, or obese. SETMA determines the BMI for every patient seen in our clinic. Ideally, your BMI should be below 15 and a value above 30 puts you at significant risk for insulin resistance and diabetes.
- Blood pressure. Blood pressure is expressed as two numbers that represent pressure in your blood vessels when your heart is beating (systolic pressure) and when it is resting (diastolic pressure). The numbers are usually written with a slash€”for example, 140/90, which is expressed as "140 over 90." For the general population, blood pressure below 130/85 is considered normal, although people whose blood pressure is slightly elevated and who have no additional risk factors for heart disease may be advised to make lifestyle changes€”that is, diet and exercise€”rather than take blood pressure medicines. People who have diabetes, however, should take whatever steps necessary, including lifestyle changes and medicine, to reach a blood pressure goal of below 130/80.
- Cholesterol. Your cholesterol is usually reported with three values: low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and total cholesterol. LDL cholesterol is sometimes called "bad" cholesterol, while HDL cholesterol is called "good" cholesterol. To lower your risk of cardiovascular problems if you have diabetes, you should try to keep your LDL cholesterol below 100 and your total cholesterol below 200.
If you have the cardiometabolic risk syndrome, your doctor will recommend weight loss with diet and exercise, as well as possibly recommending medication to lower your cholesterol and blood pressure levels.
Stop Smoking
In addition to increasing your risk of cancer and cardiovascular disease, smoking contributes to insulin resistance. Quitting smoking is not easy, but it could be the single smartest thing you can do to improve your health. You will reduce your risk for respiratory problems, lung cancer, and diabetes.
Be Active and Eat Well
Physical activity helps your muscle cells use blood glucose because they need it for energy. Exercise makes those cells more sensitive to insulin.
The Diabetes Prevention Program (DPP) confirmed that people who follow a low-fat, low-calorie diet and who increase activities such as walking briskly or riding a bike for 30 minutes, five times a week, have a far smaller risk of developing diabetes than people who do not exercise regularly. The DPP also reinforced the importance of a low-calorie, low-fat diet. Following a low-calorie, low-fat diet can provide two benefits. If you are overweight, one benefit is that limiting your calorie and fat intake can help you lose weight. DPP participants who lost weight were far less likely to develop diabetes than others in the study who remained at an unhealthy weight. Increasing your activity and following a low-calorie, low-fat diet can also improve your blood pressure and cholesterol levels and has many other health benefits.
Before the pancreatic Beta cells, which produce insulin, fail, producing type 2 diabetes, they are put under stress by the increasing demand for more insulin produced by insulin resistance. The factors which produce insulin resistance are genetic and acquired, such as obesity, aging and a sedentary life style.
If you want to read more about “insulin resistance,” you can at www.jameslhollymd.com under Your Life Your Health, Cardiometabolic Risk Syndrome Part II: Insulin Resistance, December 7, 2006.
|