|
In a September, 2012 article entitled, “Atypical Antipsychotic Use in Patients With Dementia: Managing Safety Concerns,” the American Journal of Psychiatry stated:
“In the elderly population, the largest number of prescriptions for atypical antipsychotics is written for the neuropsychiatric symptoms (NPS) of dementia, e.g., delusions, depression, agitation which affect up to 97% of people with dementia.
“This Treatment is especially challenging because, while the symptoms often cause significant distress, no effective alternative medication treatments are available. Efficacy seems best, albeit modest, for atypical antipsychotics, but these must be used with great caution due to risk of adverse events including stroke and death. Before an antipsychotic is started, comprehensive assessment must be performed to rule out a medical etiology, as well as environmental and caregiving factors that could be provoking the targeted behavior.
An antipsychotic trial is warranted when non-pharmacological intervention is unsuccessful and behaviors cause significant distress and/or pose a safety risk. Low doses should be used, with slow titration as needed. Patients and surrogate decision-makers should be educated about side effects to observe for, such as fall, Parkinsonism, and sedation. Metabolic parameters should be regularly monitored, although metabolic adverse effects may be of less concern in the elderly. Face-to-face visits are essential to monitor response, tolerance, and the need for continued treatment, and a discontinuation trial should be strongly considered in patients with a 3-6 month history of behavioral stability.
Until better treatment options become available, atypical antipsychotics continue to have an important, albeit limited, role in dementia care. Safety risks can be minimized through careful selection of appropriate patients for treatment, education of patients and surrogate decision-makers, and close monitoring, with the understanding that for many patients, short term treatment is sufficient.”
In an effort to decrease the inappropriate use of antipsychotic medications in Texas Nursing Homes, The Texas Medical Foundation and the Texas Department of Aging and Disability provided this toolkit. Because SETMA provides care to over 80% of the long-term care residents in Southeast Texas, which comprises a five county area, and because SETMA documents the care of those patients in our electronic patient record (EMR), we have taken this tool kit and created a Clinical Decision Support tool to improve the care of the patients for whom we have responsibility.
The following are the templates and functionalities which are now deployed in SETMA’s EMR.
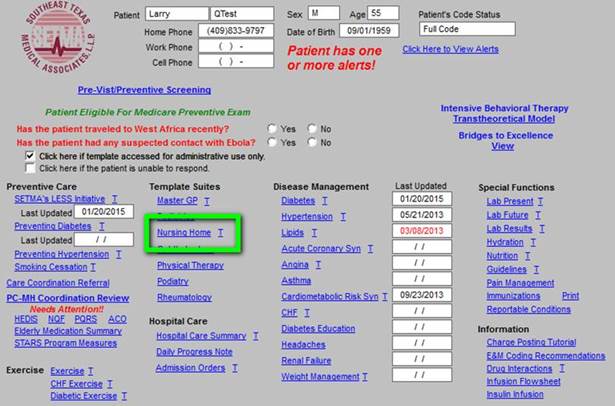
First is the principle template which launches all of our electronic patient care. Outlined in green on this template is the hyperlink which launches the Nursing Home suite of templates.
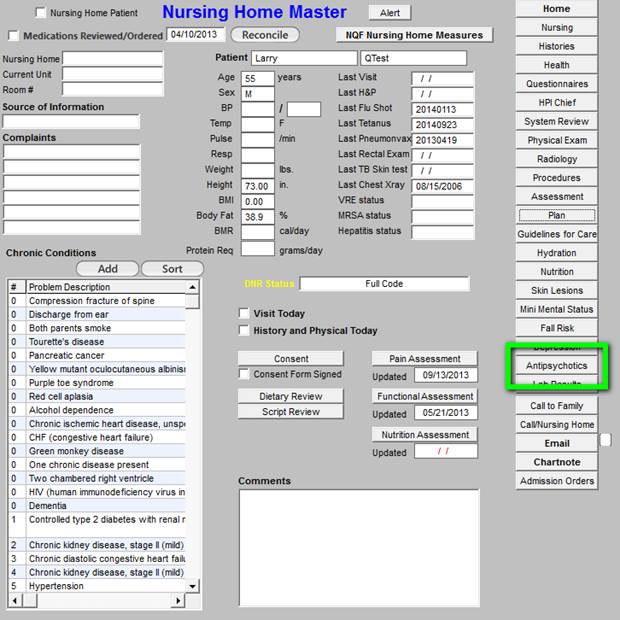
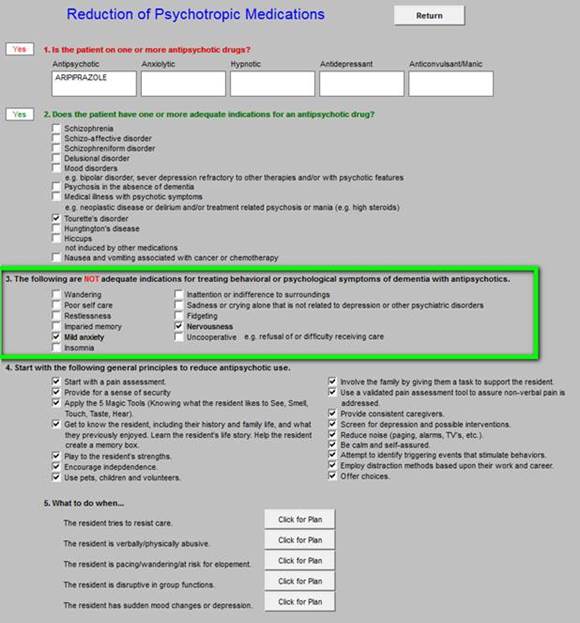
When the Nursing Home hyperlink is deployed the Nursing Home Master template is displayed. Outlined in green is the button which launches the Antipsychotics Toolkit. There are five sections to the tool kit:
- Is the patient on one or more antipsychotic drugs?
- Does the patient have one or more diagnoses for an antipsychotic drug?
- The following are not adequate indications for treating behavioral or psych9ological symptoms of dementia with antipsychotics.
- Start with the following general principles to reduce antipsychotic use.
- What to do when?
When this button is deployed, the EMR is searched for Antipsychotic Drugs in these Classifications:
- Antipsychotic
- Anxiolytic
- Hypnotic
- Antidepressant
- Anticonvulsant/Manic
This is a partial list of psychotropic drugs commonly used in the long-term care setting. Some of these drugs are listed under their official classifications, but may be seen with the intended use of the above classifications to alter/change mood or behavior. Any drugs which are found are automatically listed under its category.
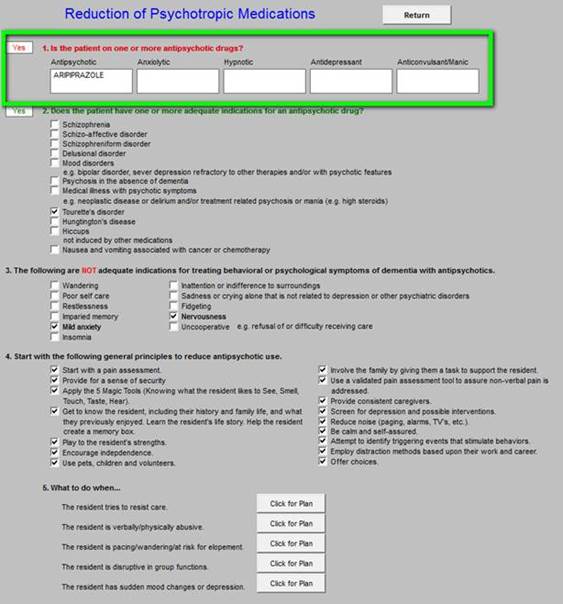
In section 2 of this template, the computer automatically denotes: “Does the patient have one or more adequate indications for an antipsychotic drug?” See below for details.
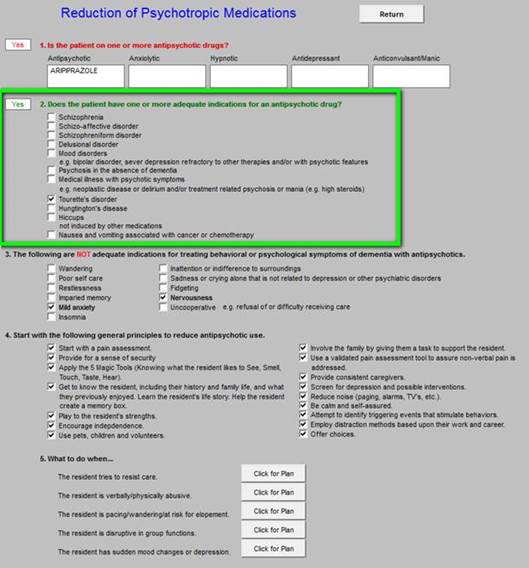
If there is no appropriate diagnosis for the use of an antipsychotic medication, consideration should be given for discontinuing the medication and/or for employing one of more of the therapeutic or environment interventions provided below.
Section 3 of the tool kit lists the indications for which antipsychotics are often used but which are inadequate indications for such use.
Section 4 lists alternatives for antipsychotic medications when there is not an indication for their use. This section lists 16 actions which can be instituted to decrease the use of antipsychotic medications. The example shows all of the actions checked off but generally you would only began a few a time.
Those which you check off will appear on the chart note to be placed on the nursing home chart or on the chart of a patient in the clinic.
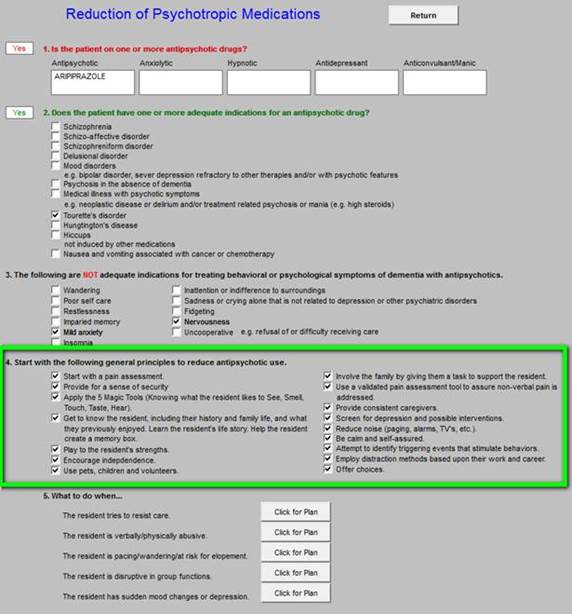
The above principles are used for the reduction of the use of physical restraints. The most important actions are to start with a pain assessment and a screen for depression. These assessments can be done with tools provided by SETMA: see Patient-Centered Medical Home Annual Questionaires for: Fall Risk, Pain Assessment, Functional Assessment, Wellness and Stress; see Depression Tutorial for depression evaluation.
Fear is created by disorientation and confusion. The “5 Magic Tools” are helpful in enhancing orientation and decreasing confusion. These “Magic Tools” involving “knowing what the resident likes to See, Smell, Touch, Taste, Hear.” Remember that new and/or strange environments can disorient and confuse patients. Using these five sensory perceptions to create a familiar and pleasant environment can help patients regain their sense of security and safety.
Section five is entitled “What can be done when?” Each of the five “What Can Be Done” recommendations give specific guides for helping patients cope with their new surroundings and with their decreasing menial acuity.
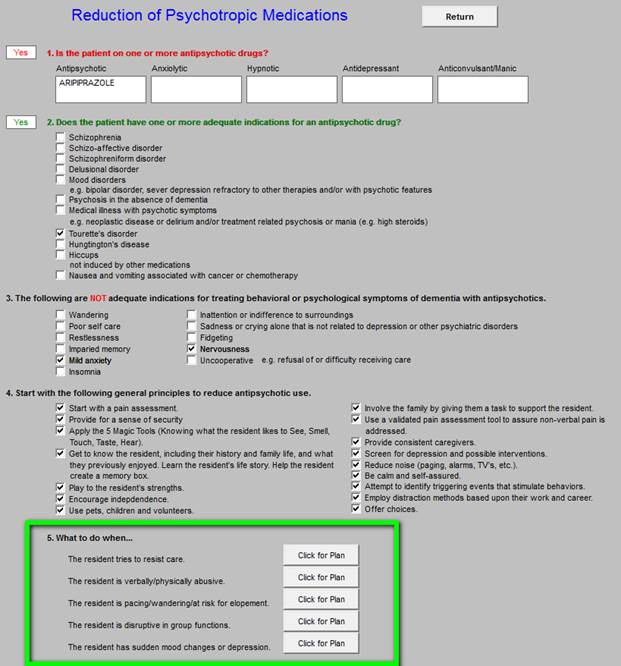
The five categories of “What to do when?” are:
- The resident tries to resist care
- The resident is verbally/physically abusive
- The resident is pacing/wandering/at risk for elopement
- The resident is disruptive in group functions
- The resident has sudden mood changes or depression
The first is “what to do when the patient resists care.”
|