|
As the pressure increases for healthcare organizations and for healthcare providers to produce quality outcomes in healthcare delivery, to prove that they are delivering quality and to report the results of their performance, there is an increasing number of agencies who are publishing standards of measurement of quality. The simplest way to measure quality is via data analysis, but this restricts measurement to processes or outcomes which can be expressed numerically or with simply "yes" or "no" answers. The problem with identifying and measuring quality is that quality in healthcare is often the result of complex processes which are not subject to simple measurement.
Diabetes is a target of quality measures for several reasons:
- Process Quality Measures, i.e., was a hemoglobin A1c (HgbA1c) done, and Outcomes Quality Measures, i.e., what was the HgbA1c value, are easy to determine and to report.
- The treatment goals for the elements of diabetes are generally known and accepted.
- Standardization of methods for laboratory testing is generally accepted.
- These three make diabetes a model for the idea of "precision medicine" presented in The Innovator's Prescription: A Disruptive Solution for Health Care. "Precision medicine," exists "Only when diseases are diagnosed precisely...can therapy that is predictably effective ...be developed and standardized. We term this domain precision medicine." The care of diabetes calls for little intuitive judgment or guess work. Anyone willing to learn the principles can do excellent care of diabetes.
- Diabetes is a devastating disease but evidence-based medicine demonstrates that aggressive and successful treatment dramatically changes the outcome of the disease.
- Diabetes is a major public health problem in that the increasing prevalence of diabetes is almost on the scale of a pandemic.
- The cost of caring for diabetes and its complications is enormous making the potential benefit of treating the illness both for the individual and for the society large.
Each of these makes diabetes an ideal condition for the development of quality metrics. There are currently at least five different national organizations that have a quality measurement set for diabetes:
- Physician Consortium for Performance Improvement (PCPI, published by the AMA)
- National Quality Forum
- Physician Quality Reporting Initiative (PQRI,. published by CMS)
- Healthcare Effectiveness Data and Information Set (HEDIS published by NCQA)
- Ambulatory Care Quality Alliance (AQA)
One of the problems with quality measures is demonstrated here. These "comprehensive diabetes quality measures sets" are different. They are not contradictory; they are just not the same. This complicates tracking and auditing of provider performance.
SETMA and others are encouraging that one standardized quality measures set for diabetes be adopted by all. Eventually this will happen, but even as we argue that the treatment of diabetes is an example of "precision medicine," some of the elements of that process are imprecise.
SETMA's Model of Care
SETMA tracks all of these measurement sets and provides each healthcare provider the ability to evaluate their own performance at the point of service. SETMA also audits each of these quality measurement sets. The difference in tracking and auditing is that tracking is done one patient at a time, while auditing looks at a group of patients. Third, SETMA analyzes the diabetes treatment data with statistical analysis in order to evaluate the validity of our treatment method and to see where we need to improve that care. In this analysis, we can identify disparities of care, gaps in care, opportunities for improvement of diabetes care overall and which of SETMA's providers may need additional training in the treatment of diabetes.
The last two steps in SEMTA's plan is to publicly report our providers' performance on various quality metrics for the treatment of diabetes. We do this at www.jameslhollymd.com. Then with the tracking and auditing data, and with the analysis and in the face of public reporting which encourages and compels improvement by all providers in their individual performance, SETMA designs disease quality improvement initiatives.
We have defined this as SETMA's Model of Care which has the following points:
- Tracking which relates to the individual patient
- Auditing which relates to a group of patients.
- Analyzing which relates to differences in care between patients who are treated to goal and those who are not, making it possible to design steps for improving care.
- Public Reporting which motivates improved performance by providers.
- Quality initiative planning and program execution
One Assessment of Quality Performance
In order to influence quality in the care of patients with diabetes, one national organization has published a set of criteria for the evaluation of the care being delivered by healthcare providers. These criteria have a weighted value with a possible 100 total points.
In order to qualify, by this organization, each provider must achieve a 75% score on the following:
Clinical Measure |
Criteria |
Points |
|
|
|
HgbA1c Poor Control >9.0% |
<15% |
12 |
HgbA1c Control <8.0% |
60% of patients in sample |
8 |
HgbA1c Control <7.0% |
40% of patients in sample |
5 |
Blood Pressure Control 140/90 mm Hg |
<35% of patients in sample |
15 |
Blood Pressure Control <130/80 mm Hg |
25% of patients in sample |
10 |
Eye Examination |
60% of patients in sample |
10 |
Smoking Status and Cessation Advice or Treatment |
80% of patients in sample |
10 |
LDL Control >130 mg/dl |
<37% of patients in sample |
10 |
LDL Control <100 mg/dl |
36% of patients in sample |
10 |
Nephropathy Assessment |
80% of patients in sample |
5 |
Foot Examination |
80% of patients in sample |
5 |
|
Total Points |
100 |
|
Points needed to Achieve Recognition |
75.0 |
SETMA questioned whether or not we met these standards, or if perhaps we exceeded them. Measuring from March 1 to May 24, 2010, we found the following results.
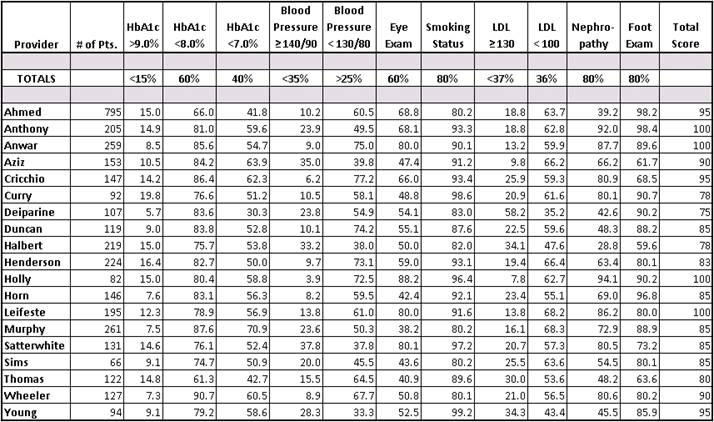
- The standard is that more than 40% of patients with diabetes have a HgbA1c below 7.0%. Almost all SETMA providers had more than 50% and some more than 60% of their patients in this group.
- The standard is that 25% of patients with diabetes have a blood pressure below 130/80. SEMTA providers have 50 and 60% of patients with diabetes whose blood pressure is below 130/80.
- The standard is that less than 37% of patients with diabetes have an LDL (Bad Cholesterol) above 130 mg.dl. SETMA provider results are significantly better ranging to as lows as 8%.
Our audit shows that all SETMA providers who care for patients with diabetes meet this organization's standards. Not satisfied, we examined SETMA's providers' data for all of 2009 and for all of 2008 and found that we meet these standards for all patients who were treated for diabetes in each of these years.
As has been previously reported, SETMA has a consistent, linear improvement in the care of diabetes as measured by HgbA1c values for the ten years from 2000 to 2009. In the years that we have been tracking standard deviations, we improved dramatically from 2008 to 2009. This means that a majority of our patients received excellent diabetes care.
The limitations of Quality Metrics
Even as we want to talk about "precision medicine" and even as we want to measure quality using quantifiable processes and outcomes, we still have to admit that there are limitations to quality metrics. Because healthcare does not deal with machines but with people, there will always be subjective, poorly quantifiable elements to quality in healthcare. This question of the balance between technology and humanity was the subject of Your Life Your Health, May 6, 2010. It can read at www.jameslhollymd.com under Your Life Your Health.
There are several critical steps which can help bridge the gap between quality metrics and true quality in healthcare. These were discussed in the April 22, 2010, Your Life Your Health. Part of that discussion addressed the place of patient-centered medial home, Medicare Advantage and Evidenced-based medicine.
Patient-Centered Medical Home (PC-MH) or Health Home
At the foundation of quality healthcare, there is an emotional bond - a trust bond - between the healthcare provider and the patient. It is possible to fulfill all quality metrics without this bond; it is not possible to provide quality healthcare without it. That is why the patient-centered medical home, coupled with the fulfilling of quality metrics is the solution to the need for quality healthcare.
The genius of PC-MH is to discover the true implications of SETMA's motto which was adopted in August, 1995, which is, "Healthcare Where Your Health is the Only Care." It is to put the patient and their needs first. And, it is to include the patient as a member of the healthcare team. There are 8,760 hours in a year. If responsibility for a patient's healthcare is seen as a "baton," the patient carries that "baton" for over 8,700 hours a year. PC-MH promotes methods for effectively "passing the baton" to the patient so that the patient's healthcare does not suffer under the patient's own care. SETMA has also placed the patient's healthcare at the center of our healthcare delivery in many ways. One way is that we developed The SETMA Foundation through which we help provide funding for the care of our patients who cannot afford it. Our resources are meager in comparison with the need, but it is a start.
The following is one example of how PC-MH and the SETMA Foundation have worked together to produce quality healthcare. A patient came to the clinic angry, hostile and bitter and was found not to be a bad person but depressed because he could not work, could not afford his medication and was losing his eye sight. He left the clinic with The Foundation paying for his medications, giving him a gas card to get to our ADA certified DSME program, waiving the fees for the classes, helping him apply for disability, and getting him an appointment to an experimental program for preserving his eyesight. He returned in six weeks with something we could not prescribe. He had hope and joy. By the way, his diabetes was to treated to goal for the first time in years.
This is PC-MH; it is caring and it is humanitarianism.
Medicare Advantage
As the Patient-Centered Medical Home is restoring the personal aspect of healthcare, the Medicare Advantage (MA) program and/or the Accountability of Care Organizations (ACO) are modifying the "piece" payment system of healthcare. While the President has been convinced that Medicare Advantage is the problem; it is the solution. The supposed increase in the cost of Medicare Advantage is because it is being compared to traditional Medicare costs where the administrative cost of Medicare is not calculated in the formulae. There are bright examples of success with Medicare Advantage, success marked by quality outcomes and high patient satisfaction. That success also is marked by a dramatic change in the trajectory of health care cost while maintaining its quality.
Quality Metrics: Process and Outcomes
The third piece to true healthcare transformation is including quality process and quality outcomes in the payment formula. There are fledgling programs such as the Physician Quality Reporting Initiative (PQRI) where healthcare providers are being paid for the demonstration of quality outcomes rather than just for piece work. The accountability of the public reporting of provider performance on quality measures completes this picture. This is why SETMA has begun quarterly reporting on our website of our providers' performance on multiple quality metrics. Included in that reporting is the examination of whether disparities of care in ethnic and socio-economic groups have been eliminated.
Conclusion
Quality healthcare is a complex problem. Measureable processes and outcomes are only one part of that complexity. Communication, collaboration and collegiality between healthcare provider and patient, between healthcare provider and healthcare provider, between healthcare providers and other healthcare organizations are important aspects of that complexity also. Data and information sharing within the constraints of confidentiality add another layer of complexity. All of these aspects of healthcare quality can be addressed by technology but only when that technology is balanced by humanitarianism.
The good news is that the right questions are being asked and historically in that setting the right answers have been found.
|