|
The following is a review of the requirements for using the new Transition of Care Management Codes (TCM) with a review of the process development which SETMA has done to make it possible for SETMA providers to respond to this opportunity for enhanced reimbursement with clarity and accuracy.
Over the past fifteen years, SETMA has developed the use of electronic, systems-wide solutions which often were not reimbursed. We have always believed that the day would come when we would be compensated for the quality of our work. The TCM codes, along with the Physician Quality Reporting System, Meaningful Use and Bridges to Excellence are the most recent example of why our hard work is now “paying off, both for our patients and our practice.
Below, we review each of the requirements for billing for TCM and then we discuss SETMA’s information technology and organization structural development for performing each of the tasks required. The solutions are discussed under the heading of “Preparation.” It is, I think, remarkable that except in one instance, SETMA has built functionalities which answer every element of the complex TCM Codes. That one issue is follow-up calls within 2 days for patients discharged from the hospital on Friday. We are already devising a solution for that need.
In order to bill for a TCM Service, the following must occur:
- The provider must have contact with the patient within two days of the patient leaving the hospital.
Preparation -- In August, 2010, SETMA began care coaching calls the day following a patient’s discharge from the hospital. We are now adding an MSW and an RN for home visits following hospitalization and for fragile patients who are at increased risk of hospitalization.
- Communicating (via direct contact, telephone, electronic) with the beneficiary and/or caregiver, including education of patient and/or caregiver within 2 business days of discharge based on a review of the discharge summary and other available information such as diagnostic test results, including each of the following tasks:
Preparation - In 2001, SETMA began completing hospital discharge summaries in our EMR making them instantly available in the clinic, in the Nursing Home and in all other venues where patients are treated. In 2005, SETMA reorganized the hospital care team such that now, 98.7% of the time the discharge summary is completed at the time the patient leaves the hospital. In June 2009, the Physician Consortium for Performance Improvement published a Transitions of Care Measurement Set. SETMA immediately deployed that quality measure set and has audited our hospital charts since as to our performance on these measures. At www.jameslhollymd.com under Public Reporting, we publicly report by provider name these measures for 2009, 2010, 2011 and 2012. (See http://jameslhollymd.com/public-reporting/public-reports-by-type)
Going forward this audit is published quarterly. In August 2010, SETMA’s Care Coordination Department began making care coaching calls to all discharged patients the day after discharge. In September, 2010, SETMA renamed the “discharge summary.” The new name is “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.” This plan includes a reconciled medication list, an assessment for potential of readmission, and all follow-up information.
- Education of the patient or caregiver regarding the on-going care plan and the potential complications that should be anticipated and how they should be addressed if they arise.
- The patient’s diagnoses
- Potential Complications
- An explanation of the patient’s risk of readmission,
- The details of patient’s follow-up care with appointment times and places,
- Any additional consultations, which are visits with providers who were not involved in the hospital care,
- An order for the care coaching call including discussion of potential complications and what to do it any such occurs.
- Etc.
- Assessment of the need for and assistance in establishing or re-establishing necessary home and community based resources.
Preparation - A simplified solution to this is a referral template to the Care Coordination Department which requires less than five seconds of the provider’s time in order to obtain assistance in obtaining home health, physical therapy, provide in-home provider support, Meals on Wheels, medications, financial support, DME, education, etc. This referral includes the ability to request patient support from The SETMA Foundation. Each year the partners of SETMA give $500,000 to the Foundation which money is used to help patients obtain care they cannot afford. None of that money can benefit SETMA.
- Addressing the patient’s medical and psychosocial issues, and medication reconciliation and management.
Preparation -- At the time of discharge from the hospital and at the post-hospital visit, the SETMA healthcare team assesses Fall Risk, Pain, Function, Wellness and Stress. The tools which SETMA has deployed for these functions can be reviewed at http://jameslhollymd.com/epm-tools/Patient-Centered-Medical-Home-Annual-Questionaires these tools allow SETMA providers and staff to uncover unspoken needs in the patient’s care.
- In lieu of a call, in cases of patients who are very high risk of re-admission, a face-to-face visit in the home by an MSW or an RN would qualify for the contact within 48 hours.
Preparation - SETMA completes a “readmission risk assessment” at the time a patient is admitted to the hospital. This is given to the patient in a document entitled, “Hospital Care Plan.” This document tells the patient why they were admitted, what they can expect as far as treatment and length of stay, gives them a reconciled medication list and gives them the admission estimate of their risk of readmission. The risk assessment is repeated upon discharge and is reported to the patient or caregive4 in the Hospital Care Summary and Post Hospital Plan of Care which they are given at discharge. The security and confidence the MSW and RN give to the patient that their healthcare needs are and will be met is significant. It begins breaking the link with the idea that the emergency department is their healthcare safety net.
- Have Medication Reconciliation done prior to or at the time of the provider face-to-face visit.
Preparation - a medication reconciliation is done at admission, at discharge, at the time of the care coaching call the day after discharge and at the hospital follow-up visit which takes place in two days for patients at high risk of readmission and within five days for all others.
- Have a follow-up visit which is a 99214 (there will be very many of these) or a 99215 (there will be very few of these). This requirement is not specific to the provider face-to-face encounter but is designated as “Medical decision making of at least moderate complexity during the service period.” The entire coding system for TCM is “for the service period,” which is thirty-days post discharge.
Preparation - SETMA has the ability to correctly assess the complexity of medical decision making based on published CMS guidelines. This allows SETMA to assess the correct Evaluation and Management code in order to correctly determine if the Transition of Care Management codes are appropriately used.
- Have a follow-up face-to-face with the provider (this must be done by a Nurse Practitioner or by a Physician) within 7 days for a 99496 or within 14 days for a 99495.
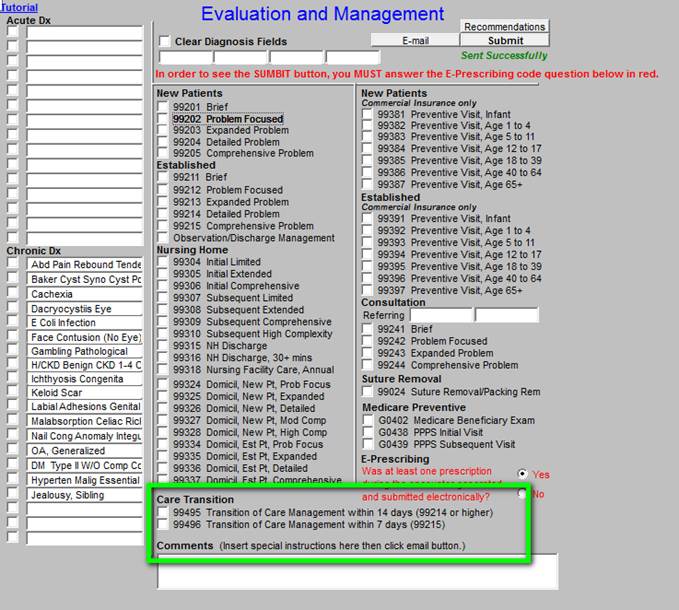
Preparation - SETMA has launched functionality in the EMR to make these management codes available. (see below) This functionality includes automation of the determination of whether the:
- Level of E&M is achieved which is required for the TCM,
- Contact within two days post discharge was done,
- Patient is seen within seven or fourteen days post discharge,
- Medication reconciliation has taken place,
- Plan of care and treatment plan has been given to the patient or caregiver.
Ongoing training will take place with SETMA’s providers to make certain that these codes are used properly. Ongoing auditing of provider compliance with CMS requirements will be done.
- At the face-to-face, this service would include:
- Assuming responsibility for the beneficiary’s care without a gap.
Preparation - The SETMA team is seamless between the inpatient and the ambulatory care setting. The same EMR is used in both. All care is documented in the same data base. The four medication reconciliations for each admission are all performed on the same medication list. The hospital admission plan of care, the hospital care summary and post hospital plan of care and treatment plan, the care coaching call and the follow-up face-to-face visit are all competed in the same data base. While there is continuity of personalities helping with the patient’s care, the ultimate continuity of care is data driven by the EMR being used at ALL points of care.
- Obtaining and reviewing the discharge summary.
Preparation - The discharge summary, which for SETMA is a much more robust and dynamic document is instantly available in the ambulatory setting whether that is the clinic, the emergency department, the nursing home, the SNF, the home health, the hospice, or any other venue of care. A SETMA provider, performing a TCM face-to-face visit, has the entire hospital documentation immediately available at the time of discharge.
- Reviewing diagnostic tests and treatments.
Preparation - the Hospital Care Summary includes all diagnostic tests, consultations, treatments and assessments. Once again the continuity of care is seamless because the records are simultaneously and instantly available everywhere. As an aside, SETMA’s confidentiality and security of patient information is state-of-the art with two factor identification and random, eight digits, numerical codes which change ever sixty seconds and which codes are uniquely tied to each provider so that every provider gets a different code which changes every sixty seconds.
- Updating of the patient’s medical record based on a discharge summary to incorporate changes in health conditions and on-going treatments related to the hospital or nursing home stay within 14 business days of the discharge.
Preparation - The diagnoses, assessments, medications, laboratory results are not only instantly available but they are dynamically interactive with the rest of the record. For instance, a hemoglobin A1C which is done in the hospital is documented in SETMA’s records and will display on Disease-specific Management tools. So, if you are accessing the most recent HbA1C after a hospitalization or an LDL the last one displayed will be the one from the hospital and not one from the clinic four weeks before.
- Establishing or adjusting a plan of care to reflect required and indicated elements, particularly in light of the services furnished during the stay at the specified facility, and to reflect result of communication with beneficiary.
Preparation - Because the plan of care and treatment plan established at discharge is a part of the patient’s permanent record, it is automatically incorporated into the ongoing plan of the patient based on diagnoses, medications, treatment plans and treatment goals.
- An assessment of the patient’s health status, medical needs functional status, pain control, and psychosocial needs following the discharge. (This summary is from the American College of Physicians)
Preparation - As addressed above, at the time of discharge from the hospital and at the post-hospital visit, the SETMA healthcare team assesses Fall Risk, Pain, Function, Wellness and Stress. The tools which SETMA has deployed for these functions can be reviewed at http://jameslhollymd.com/epm-tools/Patient-Centered-Medical-Home-Annual-Questionaires these tools allow SETMA providers and staff to uncover unspoken needs in the patient’s care.
- When indicated for a specific patient, the post-discharge transitional care service would also include:
- Communication with other health care professionals who will (re)assume care of the beneficiary, education of patient, family, guardian, and/or caregiver.
Preparation - SETMA’s Care Coordination department is electronically linked with all other SETMA providers. Internal referrals to specialists, education or testing are seamless. Referrals and transmittal of information to those providers external to SETMA are completed easily with documentation of “sent” and “received.”
- Assessment of the need for and assistance in coordinating follow-up visits with health care providers and other necessary services in the community.
- Establishment or reestablishment of needed community resources.
- Assistance in scheduling any required follow-up with community providers and services.
SETMA’s Deployment of Tools for TCM
|